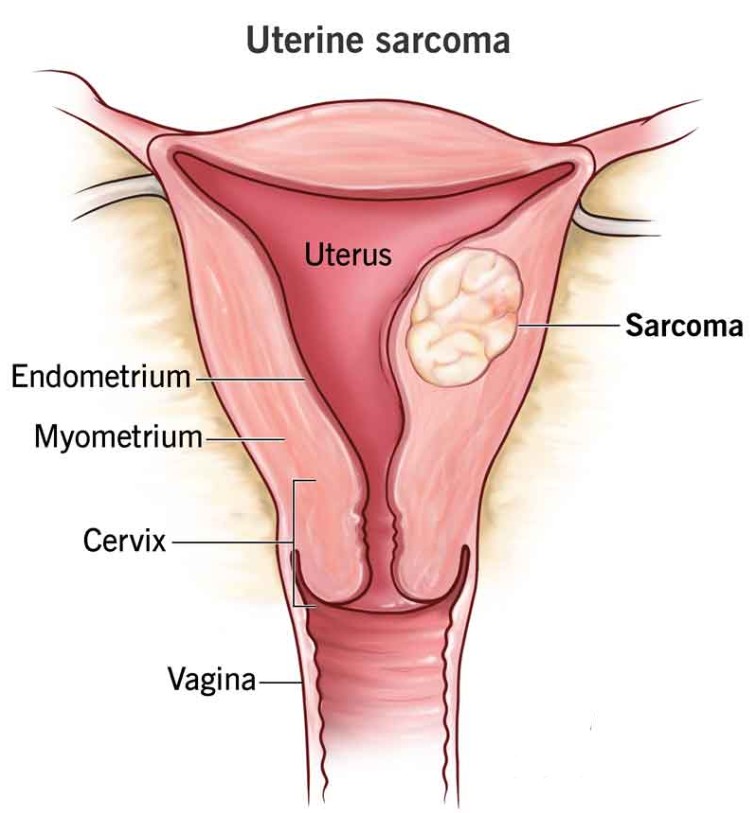
Uterine sarcoma is a rare and aggressive type of cancer that originates in the smooth muscle or connective tissues of the uterus. Unlike endometrial cancer, which arises in the lining of the uterus, uterine sarcomas develop within the uterine walls and are typically classified into three main types: leiomyosarcoma, endometrial stromal sarcoma, and carcinosarcoma. Each type has distinct characteristics, with leiomyosarcoma being the most common and aggressive, while endometrial stromal sarcoma may be less aggressive and occur at a younger age. Carcinosarcoma, which has both epithelial and mesenchymal components, is highly aggressive and often presents with a poor prognosis. Uterine sarcomas account for only a small percentage of all uterine cancers, making them difficult to diagnose and treat effectively.
The exact cause of uterine sarcoma is still unknown, but certain risk factors have been identified. These include advancing age (typically occurring in women aged 50-60), a history of uterine fibroids or other benign uterine conditions, and exposure to certain environmental factors such as radiation. Hormonal factors and genetic predispositions, such as those linked to Lynch syndrome, may also increase the risk. Symptoms of uterine sarcoma are often non-specific and may include abnormal vaginal bleeding, pelvic pain or pressure, and the presence of an enlarged uterus. These symptoms can easily be confused with other gynecological issues like fibroids, making early detection more challenging.
Diagnosis typically involves a combination of imaging tests, such as ultrasounds and MRIs, along with biopsy or endometrial sampling. However, uterine sarcomas can sometimes be misdiagnosed as benign fibroids or other conditions, delaying proper treatment. In many cases, a hysterectomy (surgical removal of the uterus) is the primary treatment for uterine sarcoma, and additional therapies such as chemotherapy or radiation may be necessary, especially if the cancer has spread beyond the uterus. While uterine sarcoma is an aggressive form of cancer, early diagnosis and treatment can improve survival outcomes, though the prognosis depends largely on the type and stage of the cancer at diagnosis.
The rarity and complexity of uterine sarcoma make it essential for women experiencing symptoms, especially those in the high-risk age group, to seek medical advice and undergo thorough evaluations. Treatment plans should be tailored to each patient's specific needs, involving a multidisciplinary team of oncologists, gynecologists, and other specialists to optimize care and improve the chances of recovery.
The exact cause of uterine sarcoma remains largely unknown, but several factors are believed to contribute to the development of the disease. Understanding these risk factors can help in early detection and prevention strategies.
1. Age
The risk of developing uterine sarcoma increases with age, with most cases diagnosed in women over the age of 50. The incidence is particularly high in postmenopausal women, as the disease is thought to be influenced by hormonal changes that occur with age.
2. Hormonal Therapy and Estrogen Exposure
Hormonal therapies that increase estrogen levels have been linked to a higher risk of uterine sarcomas. Women who have used estrogen replacement therapy (ERT) or tamoxifen (a medication used in breast cancer treatment) may have an increased risk, as prolonged exposure to estrogen may encourage the growth of uterine tumors.
3. Previous Uterine Conditions
Women who have had certain conditions, such as fibroids (benign growths of the uterine muscles), may have an increased risk of developing uterine sarcoma, particularly if these fibroids have been present for a long time. In some cases, the sarcoma can develop within or near pre-existing fibroids.
4. Genetic Factors
Some genetic conditions and inherited syndromes may increase the risk of uterine sarcoma. For example:
-
Li-Fraumeni Syndrome: This inherited condition increases the risk of several types of cancer, including uterine sarcoma.
-
Cowden Syndrome: This genetic disorder, which predisposes individuals to develop tumors in various parts of the body, also increases the risk of uterine cancers.
-
Hereditary Nonpolyposis Colorectal Cancer (HNPCC): Also known as Lynch syndrome, this inherited condition increases the risk of several cancers, including uterine and endometrial cancers.
5. Previous Radiation Therapy
Women who have undergone radiation therapy to the pelvic area for the treatment of other cancers (such as breast cancer or lymphoma) may have an increased risk of developing uterine sarcoma later in life. Radiation exposure can cause cellular damage that leads to the development of cancerous growths.
6. Obesity
Obesity is another significant risk factor for uterine cancer. Women who are overweight or obese may have higher levels of estrogen in their bodies, which can increase the likelihood of developing uterine sarcoma and other forms of uterine cancer.
The symptoms of uterine sarcoma are often nonspecific and may overlap with symptoms of other, more common uterine conditions, such as fibroids or endometrial cancer. As a result, uterine sarcoma can be difficult to diagnose at an early stage. However, some common symptoms that may indicate the presence of uterine sarcoma include:
1. Abnormal Vaginal Bleeding
One of the most common symptoms of uterine sarcoma is abnormal vaginal bleeding, which can occur between menstrual periods or after menopause. This may include:
-
Heavy or prolonged menstrual periods.
-
Bleeding after sexual intercourse.
-
Bleeding between periods.
-
Postmenopausal bleeding.
2. Pelvic Pain or Pressure
Women with uterine sarcoma may experience persistent pelvic pain, which can range from a dull ache to sharp or stabbing pain. The pain may occur during sexual intercourse, bowel movements, or urination. This pain is often associated with the tumor growing and pressing on surrounding tissues and organs.
3. Abdominal Swelling or Bloated Feeling
As the tumor grows, it can cause swelling or a feeling of fullness in the abdomen. This symptom may be more noticeable as the cancer advances and affects the size of the uterus or surrounding organs.
4. Unexplained Weight Loss
Significant, unexplained weight loss may occur in advanced stages of uterine sarcoma. This is a general symptom of many cancers and can result from the body’s efforts to fight the disease or due to metabolic changes caused by the tumor.
5. Fatigue
Fatigue is another common symptom experienced by many women with uterine sarcoma. This can result from the body’s response to the cancer, anemia (due to blood loss), or the side effects of cancer treatment.
6. Frequent Urination or Difficulty Urinating
If the tumor grows large enough to press on the bladder, it can cause urinary symptoms, including the frequent need to urinate or difficulty emptying the bladder completely.
Due to the rarity and nonspecific symptoms of uterine sarcoma, early diagnosis is challenging. However, a combination of medical history, physical examinations, imaging tests, and biopsy procedures can help in diagnosing the condition.
1. Physical and Pelvic Exam
During a pelvic examination, a doctor may detect signs of uterine enlargement or abnormal masses that could indicate the presence of a tumor. If uterine sarcoma is suspected, the physician may also conduct a rectovaginal examination to assess for deeper abnormalities.
2. Imaging Tests
Imaging tests are essential in diagnosing uterine sarcoma and determining its extent:
-
Ultrasound: A transvaginal ultrasound can help visualize abnormalities in the uterus and detect signs of a mass or growth.
-
CT Scan (Computed Tomography): A CT scan can provide detailed images of the uterus, pelvis, and surrounding tissues. It helps assess the size and location of the tumor and whether the cancer has spread.
-
MRI (Magnetic Resonance Imaging): MRI is particularly useful for assessing the size, extent, and involvement of surrounding tissues in uterine sarcoma. It provides a detailed view of the uterus and pelvic organs.
3. Biopsy
A biopsy is the most definitive diagnostic tool for uterine sarcoma. A sample of tissue is taken from the suspected tumor and examined under a microscope to confirm the presence of cancer and determine its type and grade.
4. Hysteroscopy
A hysteroscopy allows a doctor to examine the inside of the uterus with a thin, lighted tube inserted through the cervix. It may be used to view abnormal growths or masses in the uterine cavity and to guide biopsy procedures.
Treatment for uterine sarcoma depends on several factors, including the type and stage of the cancer, the woman’s overall health, and whether the cancer has spread. The main treatment options for uterine sarcoma include:
1. Surgery
Surgery is typically the first line of treatment for uterine sarcoma. The goal is to remove as much of the tumor as possible, and in many cases, the uterus is removed entirely. Surgical options include:
-
Total Hysterectomy: Removal of the uterus, including the cervix. This is often combined with the removal of nearby lymph nodes if the cancer has spread.
-
Oophorectomy: Removal of the ovaries, especially if the cancer is found to involve them or if the patient is at a higher risk of recurrence.
2. Radiation Therapy
Radiation therapy uses high-energy rays to target and kill cancer cells. It may be used after surgery to kill any remaining cancer cells, particularly if the tumor was large or if the cancer has spread to surrounding tissues. In some cases, radiation may be used before surgery to shrink the tumor.
3. Chemotherapy
Chemotherapy involves using powerful drugs to kill or control cancer cells. It is often used for more advanced uterine sarcomas, especially when the cancer has spread beyond the uterus. Chemotherapy may be used in combination with surgery or radiation therapy to treat the cancer more effectively.
4. Hormone Therapy
For certain types of uterine sarcoma that are hormone-sensitive, hormone therapy may be used to block the hormones that promote cancer growth. This is not typically used for all forms of uterine sarcoma but may be an option in specific cases.
5. Targeted Therapy and Immunotherapy
Targeted therapies and immunotherapies are emerging treatments for uterine sarcoma, especially in cases where the cancer is resistant to other treatments. These therapies target specific molecules or pathways involved in cancer cell growth and can be used to treat advanced or recurrent cancers.
While uterine sarcoma cannot always be prevented, certain strategies can help reduce the risk and improve management:
1. Genetic Counseling and Testing
For women with a family history of uterine or other reproductive cancers, genetic counseling may help assess the risk of hereditary cancer syndromes. Genetic testing can help identify mutations that increase the risk of uterine sarcoma and guide decisions about screening and prevention.
2. Early Detection and Screening
Since uterine sarcoma is rare, there are no established screening guidelines for the general population. However, women with known risk factors (such as those with Lynch syndrome or a history of radiation therapy) may benefit from regular pelvic exams and imaging tests.
3. Healthy Lifestyle Choices
Maintaining a healthy weight, avoiding smoking, and limiting exposure to known carcinogens can reduce the risk of uterine sarcoma and other types of cancer. Regular physical activity and a balanced diet rich in fruits and vegetables also contribute to overall health.
Treatment for uterine sarcoma can lead to several complications, including:
1. Fertility Issues
Since uterine sarcoma often requires the removal of the uterus and possibly ovaries, women who wish to preserve fertility may face challenges. Fertility preservation options, such as egg or embryo freezing, should be discussed with a fertility specialist before treatment.
2. Recurrence of Cancer
Uterine sarcoma has a high rate of recurrence, particularly if the tumor was not completely removed during surgery. Regular follow-up care is essential for detecting and managing recurrence.
3. Sexual and Psychological Effects
The removal of the uterus and/or ovaries can lead to changes in sexual function, including vaginal dryness, discomfort, and decreased libido. The psychological effects of cancer treatment, such as depression and anxiety, can also impact quality of life.
Living with uterine sarcoma involves ongoing monitoring, emotional support, and lifestyle adjustments:
1. Long-Term Follow-Up Care
Women who have been treated for uterine sarcoma require regular follow-up appointments to monitor for recurrence, manage side effects, and assess overall health. Follow-up care may include imaging tests, blood tests, and pelvic exams.
2. Emotional and Psychological Support
A uterine cancer diagnosis can be emotionally challenging. Support groups, counseling, and mental health care are essential to help women cope with the emotional and psychological impact of the disease and its treatment.
3. Rehabilitation and Lifestyle Adjustments
Physical therapy and rehabilitation may be needed to address physical symptoms and improve mobility or pelvic function. Lifestyle adjustments, including a healthy diet, regular exercise, and stress management, can support overall well-being and improve quality of life.
1. What is uterine sarcoma?
Uterine sarcoma is a rare and aggressive form of cancer that originates in the muscular or connective tissues of the uterus. Unlike endometrial cancer, which begins in the lining of the uterus, uterine sarcoma arises from the smooth muscle (myometrium) or connective tissue (stroma) of the uterus. It accounts for a small percentage of all uterine cancers and is often diagnosed at advanced stages.
2. What are the types of uterine sarcoma?
There are several types of uterine sarcoma, including:
-
Leiomyosarcoma: The most common and aggressive form, arising from smooth muscle cells in the uterus.
-
Endometrial Stromal Sarcoma (ESS): Originates from the connective tissue of the endometrium.
-
Undifferentiated Uterine Sarcoma (UUS): A highly aggressive form that is challenging to classify.
-
Carcinosarcoma (Malignant Mixed Mullerian Tumor): Contains both carcinoma (epithelial cancer) and sarcoma (connective tissue cancer) components.
3. What causes uterine sarcoma?
The exact cause of uterine sarcoma is not well understood, but several factors may increase the risk. These include genetic mutations, prior radiation therapy to the pelvic area, and conditions such as inherited cancer syndromes (e.g., Lynch syndrome). Additionally, advanced age and a history of other cancers, like breast or endometrial cancer, may increase the risk.
4. What are the symptoms of uterine sarcoma?
Common symptoms of uterine sarcoma include:
-
Abnormal vaginal bleeding (especially after menopause)
-
Pelvic pain or pressure
-
Abdominal bloating or a palpable mass
-
Unexplained weight loss
-
Fatigue or weakness
These symptoms can be similar to those of other, less serious conditions, making early diagnosis challenging.
5. How is uterine sarcoma diagnosed?
Diagnosis typically involves a combination of imaging tests (such as ultrasound, CT scan, or MRI) to evaluate the size and location of the tumor. A biopsy may be performed to confirm the diagnosis. In some cases, a hysteroscopy (a procedure to look inside the uterus) may be used. Because uterine sarcomas are often diagnosed at later stages, additional tests may be needed to determine the extent of cancer spread.
6. What are the stages of uterine sarcoma?
Uterine sarcoma is staged based on how far the cancer has spread. Staging typically ranges from Stage I (localized to the uterus) to Stage IV (spread to distant organs such as the lungs, liver, or lymph nodes). The stage of the cancer plays a critical role in determining treatment options and prognosis.
7. What are the treatment options for uterine sarcoma?
Treatment for uterine sarcoma often involves a combination of:
-
Surgery: The primary treatment for uterine sarcoma is the removal of the uterus (hysterectomy), and in some cases, the removal of the ovaries and fallopian tubes may also be necessary.
-
Chemotherapy: Used after surgery or for advanced stages to kill cancer cells that may have spread.
-
Radiation therapy: May be used for localized tumors or as a follow-up to surgery.
-
Targeted therapy or immunotherapy: These newer treatment options may be used in specific cases, especially for advanced or recurrent sarcomas.
8. What is the prognosis for uterine sarcoma?
The prognosis for uterine sarcoma depends on the type of sarcoma, the stage at diagnosis, and how well it responds to treatment. Early-stage uterine sarcoma has a relatively good prognosis if treated aggressively with surgery. However, the prognosis can be less favorable for advanced or metastatic cases, especially if the cancer has spread to distant organs.
9. Can uterine sarcoma be prevented?
There is no guaranteed way to prevent uterine sarcoma, but certain lifestyle changes and reducing known risk factors may help lower the risk. This includes maintaining a healthy weight, avoiding excessive use of hormone replacement therapy (HRT), and stopping smoking. Women who have had radiation therapy to the pelvic region in the past may also want to discuss their risk with their doctor.
10. What is the survival rate for uterine sarcoma?
The survival rate for uterine sarcoma depends on various factors, including the type, stage at diagnosis, and response to treatment. In general, the 5-year survival rate for women with localized uterine sarcoma is higher, but it drops significantly if the cancer has spread to other organs. Since uterine sarcoma is an aggressive cancer, early detection and prompt treatment are critical for improving survival rates.
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.