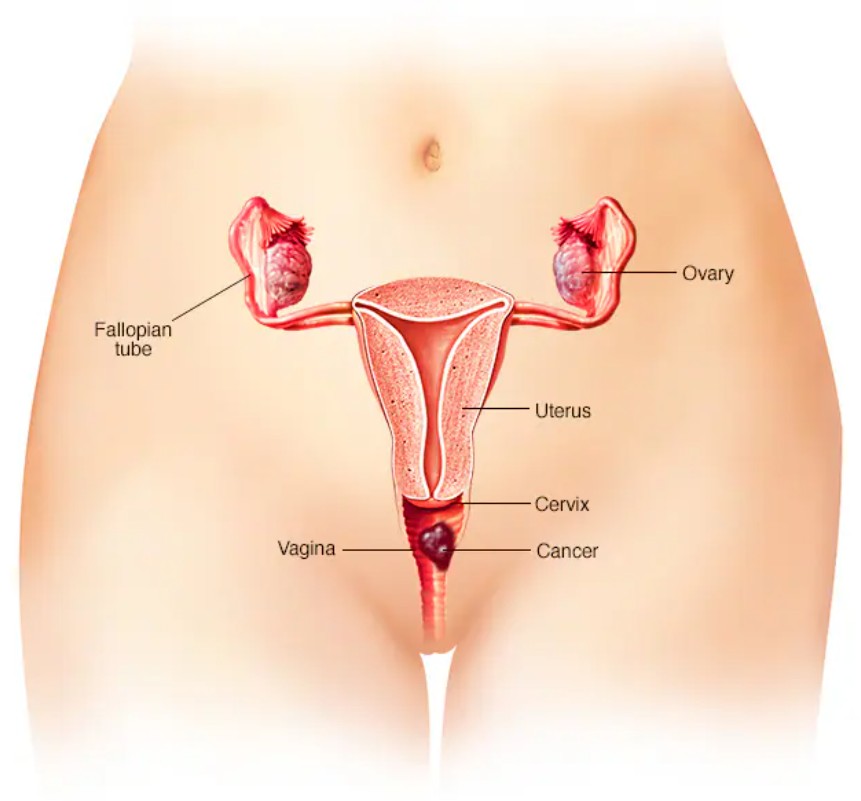
Vinal cancer is a rare form of cancer that develops in the tissues of the vagina, the hollow muscular tube that connects the external genitalia to the uterus. It is a type of gynecological cancer, and although it is much less common than other reproductive cancers such as cervical or uterine cancer, it still poses significant health risks. Vaginal cancer can affect women of any age but is more commonly diagnosed in women over the age of 60.
Vaginal cancer is typically categorized into two types: squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma, which arises from the squamous cells lining the vagina, is the most common type, accounting for about 90% of vaginal cancer cases. Adenocarcinoma, which begins in the glandular cells of the vaginal lining, is less common but tends to occur in women who have been exposed to diethylstilbestrol (DES), a synthetic estrogen used in the 1940s to 1970s to prevent miscarriages.
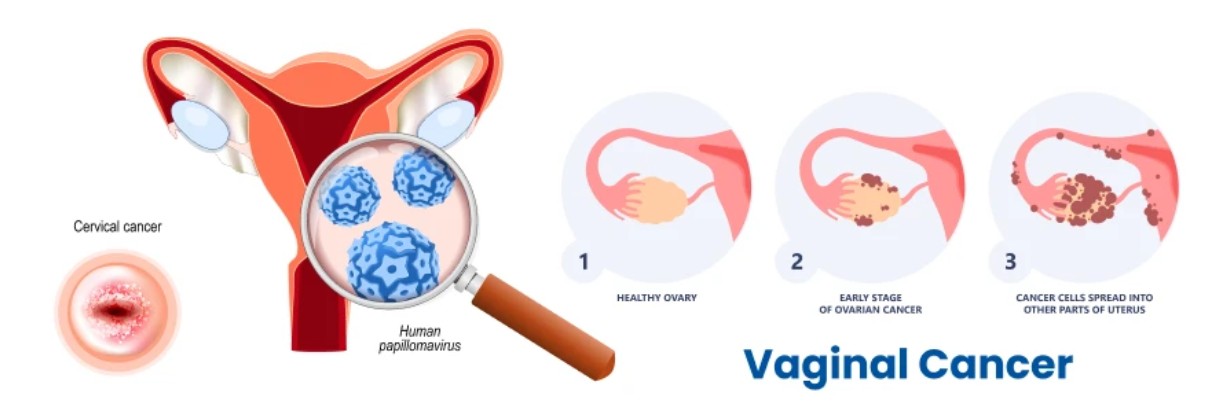
The exact cause of vaginal cancer is not fully understood, but several risk factors have been identified. A history of human papillomavirus (HPV) infection, especially strains linked to cervical cancer, is a major risk factor for vaginal cancer. Other factors include a weakened immune system, smoking, a history of radiation therapy to the pelvic area, and a previous diagnosis of cervical cancer or vulvar cancer.
Vaginal cancer may present with a range of symptoms, which can sometimes be mistaken for less serious conditions. These symptoms include abnormal vaginal bleeding (especially postmenopausal bleeding), unusual vaginal discharge, pain during intercourse, and pelvic pain. However, because these symptoms overlap with other gynecological issues, vaginal cancer may not be diagnosed until it reaches an advanced stage.
Diagnosis is typically made through a pelvic exam, followed by a biopsy of any suspicious tissue. Imaging tests like ultrasound, MRI, and CT scans are also used to determine the extent of cancer spread and to assist in staging the disease.
Treatment for vaginal cancer usually involves a combination of surgery, radiation therapy, and sometimes chemotherapy, depending on the stage and location of the tumor. If detected early, vaginal cancer has a higher chance of being treated successfully, and the overall prognosis improves significantly. However, because the disease is rare, it often presents at a later stage, making treatment more complex.
The survival rate for vaginal cancer varies depending on factors such as the stage of the cancer at diagnosis and the effectiveness of the treatment. Women who are diagnosed at an early stage have a significantly better chance of long-term survival.
Given the rarity of vaginal cancer, women should remain vigilant for unusual symptoms, especially if they have known risk factors like HPV infection or a history of pelvic radiation. Regular gynecological check-ups, early detection, and personalized treatment strategies are key to managing this rare and potentially serious condition.
The exact cause of vaginal cancer remains unclear, but several risk factors are believed to contribute to its development. These factors may increase the likelihood of developing vaginal cancer by affecting the cells within the vagina or the surrounding reproductive organs.
1. Human Papillomavirus (HPV) Infection
The most significant risk factor for vaginal cancer is HPV infection, particularly the high-risk strains such as HPV 16 and HPV 18. HPV is a sexually transmitted virus that can cause changes in the cells of the cervix, vagina, vulva, and anus. Persistent infection with high-risk strains of HPV can lead to cellular abnormalities, which may eventually develop into cancer.
In fact, most cases of vaginal squamous cell carcinoma are linked to HPV infection. Vaccines that protect against HPV, such as the Gardasil vaccine, have proven to be effective in preventing the types of HPV most commonly associated with vaginal cancer.
2. Age
Vaginal cancer is most commonly diagnosed in older women, particularly those over the age of 60. The risk increases with age, likely due to the cumulative effects of hormonal changes, chronic infections, and other risk factors over time. However, vaginal cancer can also occur in younger women, particularly those with a history of HPV or other genetic conditions.
3. History of Cervical Cancer
Women who have had cervical cancer are at an increased risk of developing vaginal cancer. Cervical cancer and vaginal cancer share many risk factors, including HPV infection, and both cancers can spread (metastasize) to nearby organs, including the vagina. If cervical cancer is not fully treated, there is a higher chance of it spreading to the vaginal area.
4. Smoking
Smoking is another significant risk factor for vaginal cancer. The chemicals in tobacco smoke can damage the cells of the cervix and vagina, increasing the risk of HPV infection and the development of cancer. Women who smoke are more likely to develop HPV-related cancers, including vaginal cancer, than non-smokers.
5. Weak Immune System
A weakened immune system, whether due to HIV/AIDS, immunosuppressive medications (such as those used in organ transplant recipients), or other health conditions, can increase the risk of vaginal cancer. A weakened immune system may not be able to effectively fight off HPV infection or prevent abnormal cell growth.
6. Diethylstilbestrol (DES) Exposure
Women who were exposed to the synthetic hormone DES (diethylstilbestrol) in utero have an increased risk of developing vaginal cancer, particularly a rare type known as clear cell adenocarcinoma. DES was prescribed to some pregnant women in the mid-20th century to prevent miscarriage, but it was later found to increase the risk of vaginal and cervical cancers in daughters exposed to the drug in the womb.
7. Family History
While vaginal cancer is not usually inherited, a family history of cancer, particularly gynecologic cancers like cervical, uterine, or ovarian cancer, may increase the risk of developing vaginal cancer. Certain inherited genetic conditions, such as Lynch syndrome, may also predispose women to various cancers, including vaginal cancer.
The symptoms of vaginal cancer can vary depending on the location, size, and stage of the tumor. In the early stages, vaginal cancer may not cause noticeable symptoms, which is why it is often diagnosed at a later stage. Common signs and symptoms of vaginal cancer include:
1. Abnormal Vaginal Bleeding
Abnormal bleeding is one of the most common symptoms of vaginal cancer. This may include:
-
Bleeding between menstrual periods.
-
Postmenopausal bleeding (bleeding after menopause).
-
Bleeding after sexual intercourse.
-
Excessive vaginal discharge that may be bloody or have a foul odor.
2. Vaginal Discharge
Women with vaginal cancer may notice an increase in vaginal discharge, which can become watery, blood-tinged, or have an unpleasant odor. This discharge can be a result of the tumor disrupting the vaginal tissue and causing inflammation.
3. Pelvic Pain or Discomfort
Pelvic pain or discomfort may occur as the tumor grows and presses against surrounding structures, such as the bladder, rectum, or uterus. The pain may be persistent or intermittent and can be aggravated during sexual intercourse or while urinating.
4. Painful Urination (Dysuria)
If the tumor grows near the bladder, it can cause pain or a burning sensation during urination. This may also cause frequent urination or difficulty emptying the bladder fully.
5. Pain During Sexual Intercourse
Vaginal cancer can cause dyspareunia (pain during sexual intercourse), particularly if the tumor affects the vaginal walls or surrounding tissues. This symptom may worsen as the cancer progresses.
6. Swelling in the Legs or Abdomen
In advanced stages of vaginal cancer, swelling in the legs, pelvis, or abdomen can occur due to the spread of the tumor to lymph nodes or other organs. This may also result in fluid retention and cause discomfort.
7. Unexplained Weight Loss
Unexplained weight loss without changes in diet or exercise is another possible sign of advanced vaginal cancer. This can be a result of the body’s response to the tumor or due to the tumor’s effect on metabolism.
Diagnosing vaginal cancer involves a combination of medical history review, physical examination, imaging tests, and laboratory procedures. Since the symptoms of vaginal cancer can overlap with those of other conditions, it is important to undergo a thorough examination to confirm the diagnosis.
1. Pelvic Examination
A pelvic exam is typically the first step in diagnosing vaginal cancer. During this exam, the doctor will visually inspect the vagina and cervix for any abnormalities, masses, or lesions. The doctor may also feel for irregularities in the size and shape of the uterus and other reproductive organs.
2. Colposcopy and Biopsy
If an abnormal area is found during the pelvic exam, the doctor may perform a colposcopy, which uses a magnifying device to closely examine the vagina and cervix. A biopsy may be performed during this procedure to remove a small sample of tissue from the suspected tumor for laboratory analysis.
3. Imaging Tests
-
CT Scan (Computed Tomography): A CT scan provides detailed images of the abdomen and pelvis and is used to assess the extent of the tumor and check for metastasis to nearby organs or lymph nodes.
-
MRI (Magnetic Resonance Imaging): MRI is particularly useful for assessing the size and location of the tumor and its involvement with surrounding tissues, including the bladder, rectum, and lymph nodes.
-
PET Scan (Positron Emission Tomography): A PET scan may be used to assess whether cancer has spread to other parts of the body and to evaluate the effectiveness of treatment.
4. Blood Tests
Blood tests may be used to assess the overall health of the patient, kidney and liver function, and to check for tumor markers. Elevated levels of CA-125 (a protein associated with ovarian and uterine cancers) may be seen in some women with vaginal cancer.
The treatment for vaginal cancer depends on the stage and type of cancer, the size and location of the tumor, and the patient's overall health. The main treatment options for vaginal cancer include:
1. Surgery
Surgery is typically the primary treatment for localized vaginal cancer. Surgical options may include:
-
Vaginectomy: Removal of the vagina, which may be necessary if the tumor is large or has spread throughout the vaginal walls.
-
Pelvic Lymphadenectomy: Removal of lymph nodes in the pelvic area if cancer has spread to the lymph nodes.
-
Radical Hysterectomy: If the tumor has spread to the uterus, a radical hysterectomy (removal of the uterus, cervix, and possibly surrounding tissues) may be performed.
2. Radiation Therapy
Radiation therapy is often used in combination with surgery to treat vaginal cancer. It uses high-energy rays to target and kill cancer cells, either as a primary treatment or after surgery to eliminate any remaining cancer cells. Radiation therapy can be delivered externally or internally (brachytherapy) depending on the location and size of the tumor.
3. Chemotherapy
Chemotherapy involves using drugs to kill cancer cells throughout the body. It is typically used for advanced or metastatic vaginal cancer or when surgery and radiation are not effective. Chemotherapy may be used alone or in combination with other treatments.
4. Hormone Therapy
Hormone therapy may be used in specific cases where the cancer is sensitive to hormones. This type of therapy involves the use of medications to block hormones that stimulate cancer growth.
Prevention and Management of Vaginal Cancer
While vaginal cancer cannot always be prevented, certain steps can help reduce the risk and improve early detection:
1. HPV Vaccination
The most effective way to reduce the risk of vaginal cancer is through HPV vaccination. Vaccines such as Gardasil protect against high-risk HPV strains that are associated with vaginal cancer and other HPV-related cancers.
2. Regular Screening and Pelvic Exams
Regular pelvic exams and Pap smears are important for early detection of abnormal cervical or vaginal changes. Women at higher risk, such as those with a history of HPV or cervical cancer, should discuss with their healthcare provider about appropriate screening intervals.
3. Healthy Lifestyle
Maintaining a healthy weight, avoiding smoking, and practicing safe sex by using condoms can help reduce the risk of HPV infection and vaginal cancer. A balanced diet rich in fruits, vegetables, and whole grains also supports overall health and immune function.
Treatment for vaginal cancer can result in several complications, including:
1. Sexual Dysfunction
Treatment for vaginal cancer, especially surgery and radiation, can result in vaginal dryness, narrowing, and scarring, which may make sexual intercourse painful or difficult. Women may require long-term treatment, such as vaginal dilators or lubricants, to manage these symptoms.
2. Infertility
If a woman’s uterus or ovaries are removed as part of the treatment for vaginal cancer, infertility may occur. Women wishing to preserve fertility before treatment should consider fertility preservation options such as egg or embryo freezing.
3. Lymphedema
If pelvic lymph nodes are removed during surgery, women may experience lymphedema, which is swelling in the legs or pelvic area due to the disruption of lymphatic drainage.
4. Recurrence of Cancer
Vaginal cancer has a relatively high rate of recurrence, particularly if it was not completely removed during surgery. Regular follow-up appointments, including imaging tests and pelvic exams, are essential for detecting and managing recurrence.
Living with vaginal cancer requires ongoing care, monitoring, and emotional support:
1. Long-Term Follow-Up Care
Women who have undergone treatment for vaginal cancer need regular follow-up care to monitor for recurrence and manage any ongoing symptoms or side effects. This may include pelvic exams, imaging studies, and blood tests.
2. Psychological and Emotional Support
A cancer diagnosis can be emotionally taxing. Psychological counseling, support groups, and mental health services can help women cope with the psychological challenges of the disease and its treatment.
3. Lifestyle Adjustments
Women recovering from vaginal cancer treatment may need to make lifestyle adjustments, including physical therapy, dietary changes, and stress management techniques, to improve overall well-being and quality of life.
1. What is vaginal cancer?
Vaginal cancer is a rare type of cancer that develops in the tissues of the vagina. It can arise from the cells lining the inside of the vagina (squamous cell carcinoma) or other types of cells. Vaginal cancer is most commonly diagnosed in women over the age of 60, though it can occur at any age. It may develop as a primary cancer or as a result of the spread of cancer from other parts of the reproductive system, such as the cervix or vulva.
2. What causes vaginal cancer?
The exact cause of vaginal cancer is not fully understood, but certain risk factors increase the likelihood of developing this condition. These include:
-
Human papillomavirus (HPV) infection, especially high-risk strains like HPV-16 and HPV-18.
-
Age, with the highest incidence seen in women over the age of 60.
-
History of cervical or vulvar cancer, as vaginal cancer can develop from the spread of cancer in these areas.
-
Smoking, which is linked to an increased risk of developing various cancers, including vaginal cancer.
-
Weakened immune system, such as in people with HIV or those taking immunosuppressive drugs.
3. What are the symptoms of vaginal cancer?
The symptoms of vaginal cancer can vary, but common signs include:
-
Unusual vaginal bleeding or discharge, especially after menopause
-
Pain during sexual intercourse (dyspareunia)
-
Pelvic pain or pressure
-
A visible lump or mass in the vagina
-
Pain or discomfort in the lower abdomen or pelvis
It’s important to note that early stages of vaginal cancer may not cause noticeable symptoms, which is why regular gynecological exams are important.
4. How is vaginal cancer diagnosed?
Vaginal cancer is typically diagnosed through a combination of physical exams and imaging tests. A pelvic exam is performed to check for any abnormalities or masses in the vaginal area. If suspected, a colposcopy (an examination using a magnifying instrument) or biopsy (removal of a small tissue sample) is done to confirm the diagnosis. Additional imaging tests, such as ultrasound, CT scans, or MRIs, may be used to determine the extent of cancer spread.
5. What are the stages of vaginal cancer?
Vaginal cancer is staged based on how far the cancer has spread from its original location. The stages range from Stage I (localized to the vagina) to Stage IV (advanced cancer that has spread to distant organs such as the bladder, rectum, or lymph nodes). Staging is crucial for determining the treatment approach and prognosis.
6. What treatment options are available for vaginal cancer?
Treatment for vaginal cancer depends on the stage and location of the cancer. Common treatment options include:
-
Surgery: The removal of the tumor, part of the vagina, or the entire vagina in some cases. In advanced cases, removal of surrounding tissues, such as the cervix, uterus, or lymph nodes, may be necessary.
-
Radiation therapy: Often used for localized cancers or in conjunction with surgery.
-
Chemotherapy: Typically used for advanced or metastatic vaginal cancer, especially when the cancer has spread to other organs.
-
Laser therapy or photodynamic therapy: May be used for early-stage or localized cancers to remove or shrink tumors.
7. Can vaginal cancer be prevented?
While there is no guaranteed way to prevent vaginal cancer, certain steps can help reduce the risk:
-
Vaccination against HPV: The HPV vaccine can significantly reduce the risk of cervical, vaginal, and other cancers caused by HPV infection.
-
Regular screening: Women should have regular Pap smears and pelvic exams to detect abnormal changes early, especially if they are at higher risk.
-
Avoid smoking: Quitting smoking can reduce the risk of several cancers, including vaginal cancer.
-
Safe sexual practices: Using condoms and limiting the number of sexual partners can help reduce the risk of HPV infection.
8. What is the prognosis for vaginal cancer?
The prognosis for vaginal cancer depends on various factors, including the stage at diagnosis, the cancer type, and the patient’s overall health. If caught early, the prognosis is generally favorable, with a higher chance of successful treatment. However, vaginal cancer can be aggressive, and advanced cases may have a less favorable outlook. Early detection and prompt treatment are key to improving the chances of a positive outcome.
9. What are the potential complications of vaginal cancer?
Potential complications of vaginal cancer and its treatment include:
-
Difficulty with sexual intercourse due to pain or vaginal changes after surgery or radiation therapy.
-
Urinary and bowel issues if the cancer spreads to surrounding organs like the bladder or rectum.
-
Lymphedema (swelling) if lymph nodes are removed during surgery.
-
Recurrence of cancer after treatment, which may require further interventions.
10. How do patients cope with the emotional impact of vaginal cancer?
A diagnosis of vaginal cancer can be emotionally challenging, as it may affect a woman’s body image, sexuality, and overall quality of life. It’s important for patients to seek emotional support through counseling, support groups, or therapy. Talking openly with healthcare providers, family members, and friends can help manage feelings of anxiety, depression, or isolation. Many hospitals and cancer centers offer psychological support services to help patients cope with the emotional aspects of cancer treatment.
The other Oncology Procedures are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | ../ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.