Corneal transplantation, also known as corneal grafting or keratoplasty, is a surgical procedure in which a damaged or diseased cornea (the clear, dome-shaped surface that covers the front of the eye) is replaced with a healthy cornea from a donor. This procedure is commonly performed to restore vision in individuals whose corneas are severely damaged by disease, injury, or degeneration. The goal of corneal transplantation is to improve visual function, alleviate pain, and enhance the quality of life for individuals affected by corneal disorders.
The cornea plays a vital role in vision as it focuses light entering the eye. Any condition that impairs its clarity, such as scarring, swelling, or thinning, can lead to blurred vision, discomfort, or even blindness. Corneal transplant surgery is one of the most frequently performed and successful types of organ transplant surgeries worldwide, offering high success rates and significant improvements in visual acuity.
There are several types of corneal transplantation, depending on the extent of the damage and the part of the cornea affected. These include penetrating keratoplasty (PK), where the full thickness of the cornea is replaced, and lamellar keratoplasty, which replaces only part of the cornea. The choice of procedure depends on the specific condition and needs of the patient.
The need for corneal transplantation arises from a variety of conditions that lead to corneal dysfunction. These conditions may cause clouding, scarring, or thinning of the cornea, impairing its ability to transmit light effectively. Below are the primary causes and risk factors associated with corneal transplantation:
1. Corneal Disease and Degeneration
Several diseases affect the structure of the cornea, leading to visual impairment and the need for a transplant. These include:
-
Fuchs’ Endothelial Dystrophy: A hereditary condition that causes the cells in the innermost layer of the cornea to deteriorate, leading to swelling and scarring.
-
Keratoconus: A progressive thinning of the cornea that causes it to bulge outward, leading to irregular astigmatism and distorted vision.
-
Bullous Keratopathy: A condition where the corneal endothelial cells fail to pump excess fluid out of the cornea, causing fluid buildup, pain, and vision loss.
2. Trauma and Injury
Injuries to the cornea, including chemical burns, blunt trauma, or penetrating wounds, can damage the delicate corneal tissue, leading to scarring or irregularities that affect vision. Trauma may also result in infections or other complications that necessitate corneal transplantation.
3. Infections
Infections of the cornea, such as bacterial keratitis, fungal keratitis, and viral infections (including herpes simplex virus), can lead to corneal scarring, opacification, or thinning. If the infection causes permanent damage that cannot be repaired with medical treatment, a corneal transplant may be required.
4. Genetic and Autoimmune Conditions
Inherited conditions, such as corneal dystrophies and autoimmune disorders, can affect the cornea’s clarity and health. Autoimmune diseases like rheumatoid arthritis and Steven-Johnson syndrome can also affect the corneal tissue and cause progressive damage.
5. Previous Eye Surgery
In some cases, complications from prior eye surgeries, including cataract surgery or refractive surgery (e.g., LASIK), may lead to corneal irregularities that necessitate a transplant.
6. Age and Gender
Although corneal transplantation can be performed at any age, it is more common in adults over the age of 50. Some conditions, like keratoconus, are more frequently diagnosed in younger individuals, especially those in their late teens and 20s. Gender can also influence the likelihood of certain corneal conditions, with men often being more prone to developing keratoconus.
7. Previous Infections and Scarring
A history of repeated infections or inflammation of the eye can increase the likelihood of developing corneal scarring, which may eventually require a corneal transplant for vision restoration.
Corneal transplantation is typically indicated when a person experiences significant symptoms related to vision loss, pain, or discomfort due to corneal disease. The symptoms and signs that may lead to the recommendation for a corneal transplant include:
1. Blurred or Distorted Vision
The most common symptom of corneal disease is blurred vision or distorted vision, often due to scarring, clouding, or thinning of the cornea. If these symptoms cannot be corrected with glasses, contact lenses, or other refractive surgery, a corneal transplant may be necessary.
2. Pain and Discomfort
Pain and discomfort in the eye are often associated with conditions like keratoconus, Fuchs' dystrophy, or corneal injury. Individuals with these conditions may experience eye irritation, light sensitivity, and foreign body sensation.
3. Light Sensitivity (Photophobia)
Individuals with corneal disease may experience increased sensitivity to light, making it difficult to see clearly in bright conditions. This symptom is often seen in conditions that cause corneal swelling or opacification.
4. Halos Around Lights
When the cornea is not clear or has irregularities, individuals may notice halos or glare around lights, especially at night or in low-light conditions. This is often a result of corneal scarring or swelling.
5. Eye Redness and Inflammation
In some cases, corneal disease or injury may lead to chronic redness or inflammation of the eye, which can result in discomfort, pain, or a feeling of pressure in the eye.
Diagnosing the need for corneal transplantation involves a thorough eye examination and assessment of the patient’s visual function. Several tests may be used to determine the extent of corneal damage and to evaluate whether a transplant is necessary:
1. Comprehensive Eye Examination
A comprehensive eye exam is the first step in diagnosing corneal conditions. The ophthalmologist will assess the patient's visual acuity (clarity of vision), inspect the cornea for any signs of scarring, clouding, or irregularities, and evaluate the overall health of the eye.
2. Slit Lamp Examination
A slit lamp microscope is used to provide a detailed view of the anterior (front) structures of the eye, including the cornea. This allows the doctor to assess the extent of corneal damage, look for signs of infection, and evaluate the overall condition of the corneal tissue.
3. Corneal Topography
Corneal topography is a diagnostic tool that maps the surface of the cornea. It is used to detect irregularities or distortions in the corneal shape, which are common in conditions like keratoconus. This test helps determine if a corneal transplant is needed.
4. Pachymetry
Pachymetry is the measurement of the corneal thickness. It is particularly useful for evaluating conditions like Fuchs' dystrophy, where the cornea may become swollen or thickened.
5. Fluorescein Staining
Fluorescein staining involves placing a special dye in the eye to check for damage to the corneal surface. This test is helpful in detecting corneal abrasions or ulcers, which may indicate a need for transplant surgery.
Treatment for corneal disease depends on the specific condition, but in cases where the cornea is severely damaged or diseased, corneal transplantation is the most effective option. There are several types of corneal transplantation procedures:
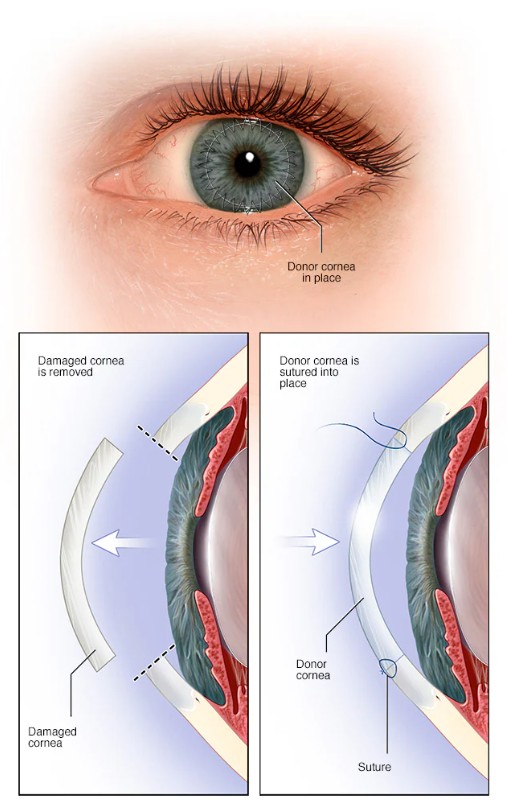
1. Penetrating Keratoplasty (PK)
Penetrating keratoplasty (PK) is the most common type of corneal transplant, where the entire thickness of the cornea is replaced with a donor cornea. This procedure is typically used for cases of severe corneal scarring, injury, or disease that affect the entire cornea.
2. Lamellar Keratoplasty
Lamellar keratoplasty involves replacing only the superficial layers of the cornea, preserving the deeper layers. This procedure is often performed for conditions like Fuchs’ dystrophy or keratoconus, where only part of the cornea is affected.
3. Endothelial Keratoplasty (EK)
Endothelial keratoplasty is a newer technique used to replace the endothelial layer of the cornea, which is the innermost layer. It is particularly useful for Fuchs’ endothelial dystrophy and bullous keratopathy, where the endothelial layer of the cornea has deteriorated, causing swelling and vision loss.
4. Descemet’s Membrane Endothelial Keratoplasty (DMEK)
DMEK is a type of endothelial keratoplasty that involves replacing only the Descemet’s membrane and the endothelial layer of the cornea. It offers better outcomes in terms of visual recovery and rejection rates compared to traditional PK.
While corneal transplantation cannot always be prevented, early diagnosis and treatment of corneal diseases can help delay the need for surgery. Preventive measures and management strategies include:
1. Regular Eye Exams
Early detection of corneal diseases is crucial for preventing the progression of damage. Regular eye exams with an ophthalmologist can help identify conditions such as keratoconus, Fuchs’ dystrophy, or corneal scars that may require intervention.
2. Protecting the Eyes
Wearing sunglasses that block UV rays can help prevent UV-related damage to the cornea, reducing the risk of cataracts or other corneal diseases. Additionally, using protective eyewear during sports or activities that pose a risk of eye injury can help prevent trauma-induced corneal damage.
3. Managing Underlying Conditions
For individuals with diabetes or autoimmune diseases, proper management of these conditions is crucial for preventing complications that can affect the cornea. Keeping blood sugar levels under control and adhering to prescribed medications can help reduce the risk of corneal disease.
4. Post-Transplant Care
After a corneal transplant, patients must follow a strict post-operative care regimen, including taking prescribed medications (e.g., anti-rejection drugs), attending follow-up appointments, and avoiding eye trauma. Adhering to these guidelines is essential for preventing complications like rejection or infection.
While corneal transplantation is highly successful, there are potential complications that patients should be aware of:
1. Rejection
The immune system may mistakenly recognize the transplanted cornea as foreign tissue, leading to graft rejection. This is a serious complication that can result in the loss of the transplant. Anti-rejection medications are often prescribed to prevent this.
2. Infection
As with any surgical procedure, there is a risk of infection following corneal transplantation. Infections can lead to graft failure and loss of vision if not treated promptly.
3. Graft Failure
Graft failure occurs when the transplanted cornea does not function properly or becomes damaged. This can happen due to infection, rejection, or trauma.
4. Glaucoma
Increased intraocular pressure (IOP) is a common complication after corneal transplantation. If left untreated, elevated IOP can lead to glaucoma and cause optic nerve damage.
After corneal transplantation, many individuals experience significant improvements in vision, especially if the transplant is successful. However, living with a corneal transplant requires lifelong monitoring and care to prevent complications. Post-operative care includes:
1. Regular Follow-Up Appointments
Patients need to attend frequent follow-up visits with their ophthalmologist to monitor the success of the transplant, check for signs of rejection or infection, and adjust medications as needed.
2. Vision Rehabilitation
Some patients may need vision rehabilitation to adjust to changes in their eyesight following the transplant. This may include learning new techniques to perform daily activities and using magnification devices.
3. Long-Term Medication Use
Patients who undergo corneal transplantation will typically need to take anti-rejection medications for several months or even years. Regular monitoring of these medications is essential to prevent side effects or complications.
1. What is corneal transplantation?
Corneal transplantation, also known as a corneal graft or keratoplasty, is a surgical procedure where a damaged or diseased cornea is replaced with a healthy cornea from a donor. The cornea is the clear, dome-shaped surface that covers the front of the eye and helps focus light. Transplantation is often needed when the cornea becomes clouded, scarred, or deformed, impairing vision.
2. Why is corneal transplantation performed?
Corneal transplantation is typically performed to treat conditions that cause severe vision impairment due to corneal damage or disease. Some of the most common reasons for a corneal transplant include:
-
Keratoconus: A condition where the cornea becomes thin and cone-shaped, distorting vision.
-
Corneal scarring: From injury, infection, or previous eye surgery.
-
Fuchs' dystrophy: A genetic condition that affects the corneal endothelium, leading to swelling and vision loss.
-
Corneal edema: Swelling caused by various conditions.
-
Trauma or injury: Damage to the cornea from accidents or burns.
3. How is corneal transplantation performed?
Corneal transplantation is typically done under local anesthesia, though general anesthesia may be used for children or anxious patients. The surgeon removes the damaged or diseased portion of the cornea and replaces it with a donor cornea. The donor cornea is stitched into place using very fine sutures. Depending on the type of transplant, recovery times and post-operative care may vary. The most common types of corneal transplants are:
-
Full-thickness (penetrating keratoplasty): The entire cornea is replaced.
-
Partial-thickness (lamellar keratoplasty): Only part of the cornea, such as the endothelial layer, is replaced.
4. What are the different types of corneal transplants?
The two main types of corneal transplants are:
-
Penetrating Keratoplasty (PK): This is the traditional full-thickness corneal transplant where the entire thickness of the cornea is replaced.
-
Lamellar Keratoplasty: This includes techniques like Deep Anterior Lamellar Keratoplasty (DALK) and Descemet’s Membrane Endothelial Keratoplasty (DMEK), where only the affected layers of the cornea are replaced, leaving the healthy layers intact.
The choice of transplant depends on the condition being treated and the health of the cornea.
5. What is the recovery process like after corneal transplantation?
Recovery after corneal transplantation varies but generally involves:
-
Post-operative medications: These include eye drops (antibiotic, anti-inflammatory, and sometimes steroids) to prevent infection and control inflammation.
-
Sutures: In most cases, sutures are used to secure the donor cornea in place and may remain for several months.
-
Follow-up visits: Frequent visits to the eye doctor to monitor healing and check for any complications.
-
Vision improvement: Full visual recovery may take months to a year, as the cornea heals and the sutures are gradually removed.
-
Avoiding physical strain: Patients are advised to avoid heavy lifting or rubbing their eyes during the initial recovery period to reduce the risk of complications.
6. What are the risks and complications of corneal transplantation?
While corneal transplantation is generally safe, there are potential risks and complications, including:
-
Rejection of the donor cornea: The immune system may attack the transplanted tissue.
-
Infection: Infection is a risk, especially during the initial healing period.
-
Glaucoma: Increased eye pressure may develop after the surgery.
-
Cataracts: A cataract may form after surgery, especially in older patients.
-
Astigmatism: The corneal shape may change after surgery, leading to blurry vision.
-
Failure of the transplant: In rare cases, the transplant may not take or may fail over time.
7. How successful is corneal transplantation?
Corneal transplantation has a high success rate, with over 90% of patients experiencing improved vision after the procedure. Success depends on factors such as the patient’s overall health, the condition being treated, and how well the transplant heals. People who follow post-operative care instructions and attend regular follow-up appointments typically have better outcomes. However, the risk of complications, such as transplant rejection or infection, exists, so ongoing monitoring is essential.
8. What is the life expectancy of a corneal transplant?
The life expectancy of a corneal transplant can vary. A transplant may last for many years, but some people may need a second transplant at some point in their lives. Factors such as transplant rejection, infection, or trauma to the eye can affect the longevity of the transplant. On average, a well-functioning corneal transplant can last from 10 to 20 years, with some patients experiencing a stable result for even longer periods.
9. Can corneal transplantation restore perfect vision?
While corneal transplantation can significantly improve vision, it may not always restore perfect vision. The outcome depends on several factors, such as the health of the donor cornea, the type of transplant, and the condition being treated. Some patients may achieve near-normal vision, while others may still need corrective lenses like glasses or contact lenses after the transplant. Regular eye exams are essential for managing vision after surgery.
10. Who is a candidate for corneal transplantation?
Candidates for corneal transplantation include individuals who:
-
Have corneal disease or damage that causes significant vision impairment, such as keratoconus, Fuchs' dystrophy, or corneal scarring from injury or infection.
-
Have not responded to other treatments, such as medications or contact lenses.
-
Are generally in good health and able to undergo surgery, although people with certain underlying health conditions may need additional evaluation.
A thorough eye examination by an ophthalmologist or corneal specialist will determine whether corneal transplantation is the appropriate treatment option.
The other Ophthalmology Procedures are:
Few Major Hospitals for Corneal Transplantation are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



