Phacoemulsification is a modern, highly effective surgical technique used to treat cataracts, a condition where the natural lens of the eye becomes cloudy, impairing vision. This technique is one of the most commonly performed eye surgeries worldwide, offering a quick, minimally invasive solution for cataract removal and vision restoration.
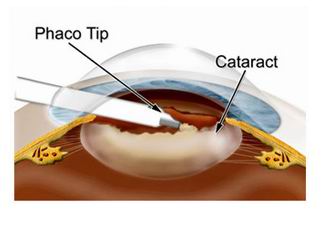
The term phacoemulsification comes from two Greek words: “phaco”, meaning lens, and “emulsification”, which refers to the process of breaking down the lens into small fragments. In this procedure, the surgeon uses ultrasonic waves to break up the cloudy lens into tiny pieces, which are then suctioned out of the eye. After the cataract is removed, an intraocular lens (IOL) is implanted to replace the natural lens and restore clear vision.
Phacoemulsification has revolutionized cataract surgery due to its high success rates, reduced recovery times, and minimal discomfort. Patients often experience significant improvements in vision within days of the procedure, with many regaining their ability to perform daily activities like driving, reading, and working without the need for glasses.
The procedure is typically performed under local anesthesia and can be done as an outpatient procedure, meaning the patient can go home on the same day.
Phacoemulsification is primarily used for treating cataracts, which form when the natural lens of the eye becomes cloudy or opaque, disrupting the passage of light to the retina. The main cause of cataracts is aging, but there are several other factors and conditions that can contribute to the need for this surgery:
Causes of Cataracts Requiring Phacoemulsification
-
Aging:
-
Age-related cataracts are the most common type of cataracts and develop as the lens of the eye naturally becomes less transparent with age. Over time, proteins in the lens begin to break down, causing cloudiness and vision impairment.
-
-
Trauma:
-
Eye injuries or trauma can cause the lens to become cloudy or damaged, leading to cataract formation. Phacoemulsification can be used to remove cataracts resulting from these injuries.
-
-
Genetic Conditions:
-
Some genetic conditions or inherited syndromes can lead to early cataract formation, such as Down syndrome or marfan syndrome.
-
-
Medical Conditions:
-
Diabetes is a significant risk factor for cataract development. Elevated blood sugar levels can lead to changes in the lens of the eye, increasing the likelihood of cataracts forming earlier in life.
-
Hypertension and other systemic diseases, such as obesity or high cholesterol, can also increase the risk of cataracts.
-
-
Medication Use:
-
Prolonged use of steroid medications can increase the risk of cataracts, particularly in the posterior lens capsule. Medications such as corticosteroids are linked to accelerated cataract formation.
-
-
UV Exposure:
-
Prolonged exposure to ultraviolet (UV) light from the sun can accelerate the development of cataracts, particularly for individuals who do not wear UV-protective sunglasses.
-
-
Smoking and Alcohol Use:
-
Both smoking and excessive alcohol consumption have been linked to the early onset of cataracts. These lifestyle choices increase oxidative stress, leading to cataract formation.
-
-
Other Eye Conditions:
-
Certain eye conditions, such as glaucoma, uveitis, or previous eye surgeries, may contribute to cataract formation, making phacoemulsification a necessary procedure.
-
The primary symptom of cataracts is vision loss, and the severity of this vision impairment increases as the cataract progresses. The need for phacoemulsification arises when cataracts interfere with daily activities and cannot be effectively managed by glasses, contact lenses, or other non-surgical treatments. Common symptoms and signs include:
1. Blurred or Cloudy Vision:
-
One of the first signs of a cataract is blurred or cloudy vision, which may affect one or both eyes. The cloudiness is caused by changes in the lens that prevent light from passing clearly through.
2. Difficulty Seeing at Night:
-
Individuals with cataracts often experience increased difficulty seeing in low-light conditions, such as driving at night. This is due to the scattering of light as it passes through the cloudy lens.
3. Glare and Halos Around Lights:
-
A person with a cataract may notice glare or halos around lights, especially when driving at night or in bright sunlight. This happens as light is scattered by the cloudy lens, causing blurred and distorted images.
4. Fading of Colors:
-
Cataracts can cause colors to appear faded or yellowed. This happens because the clouded lens filters and distorts the light entering the eye, making it difficult to distinguish between similar colors.
5. Frequent Changes in Eyeglass Prescription:
-
Individuals with cataracts often need to change their eyeglass prescription more frequently as the lens becomes cloudier over time. This may be a sign that cataract surgery, such as phacoemulsification, is necessary.
6. Double Vision:
-
In some cases, cataracts can cause double vision, where a single image appears as two overlapping images. This occurs because the lens distorts light as it enters the eye.
The diagnosis of cataracts and the decision to undergo phacoemulsification surgery are based on a thorough eye examination, including several diagnostic tests:
1. Comprehensive Eye Exam:
-
The ophthalmologist will perform a comprehensive eye exam, which includes testing the patient's visual acuity to assess how well they can see at different distances.
2. Slit-Lamp Examination:
-
A slit-lamp is used to examine the anterior segment of the eye, including the cornea, iris, lens, and retina. The slit-lamp allows the doctor to observe the cataract's size and location in the lens.
3. Retinal Examination:
-
The fundus exam involves dilating the pupils and examining the retina and optic nerve for any damage or signs of other eye conditions that could affect vision.
4. Visual Acuity Test:
-
A visual acuity test is performed to measure how well the patient can see at different distances. If visual acuity is significantly impaired due to cataracts, surgery may be recommended.
5. Tonometry:
-
Tonometry measures the intraocular pressure (IOP) inside the eye. Elevated IOP can be an indication of glaucoma, which may also be present in individuals with cataracts.
The main treatment option for cataracts is phacoemulsification surgery, which involves using an ultrasonic device to break up and remove the cloudy lens and replace it with an intraocular lens (IOL). Various IOL options are available depending on the patient’s needs:
1. Standard Monofocal IOL:
-
Monofocal IOLs provide clear vision at a single distance (usually for distance vision). Patients who opt for this type of lens may still need glasses for near vision (e.g., reading).
2. Multifocal IOLs:
-
Multifocal IOLs offer near, intermediate, and distance vision. These lenses allow for greater visual flexibility, reducing the need for reading glasses or bifocals after surgery.
3. Toric IOLs:
-
Toric IOLs are specifically designed for patients with astigmatism. These lenses correct the irregular shape of the cornea, improving both distance vision and astigmatism.
4. Accommodative IOLs:
-
Accommodative IOLs are designed to mimic the natural focusing ability of the eye. They shift slightly within the eye to allow for clear vision at various distances, which is particularly useful for presbyopia (age-related near vision loss).
5. Extended Depth of Focus (EDOF) IOLs:
-
EDOF IOLs provide a continuous range of clear vision, from near to far distances, without the need for multiple focal points.
The choice of IOL is made based on factors such as lifestyle needs, budget, and eye health. Your ophthalmologist will help guide the decision based on these factors.
While cataracts are a natural part of the aging process, there are ways to manage and potentially slow their progression:
1. UV Protection:
-
Wearing sunglasses with UV protection can help prevent cataract formation or slow their progression by shielding the eyes from harmful ultraviolet (UV) rays.
2. Healthy Diet:
-
Eating a diet rich in antioxidants, such as vitamins C and E, can help protect the eyes from oxidative damage that may contribute to cataract formation.
3. Smoking Cessation:
-
Smoking is a significant risk factor for cataracts. Quitting smoking can help reduce the risk of cataract formation and other eye diseases.
4. Regular Eye Exams:
-
Regular eye exams are essential for monitoring cataract progression. Early detection allows for timely intervention and ensures that cataracts are treated before they severely impact vision.
5. Blood Sugar Control:
-
For individuals with diabetes, maintaining proper blood sugar levels can help reduce the risk of cataracts and other eye complications.
While phacoemulsification is generally safe, there are potential risks and complications associated with the procedure:
1. Infection:
-
As with any surgery, infection can occur. Post-operative care is essential to prevent infection, including the use of prescribed antibiotic eye drops.
2. Intraocular Pressure Increase (Glaucoma):
-
After surgery, some patients may experience increased intraocular pressure (IOP), which can lead to glaucoma if not managed properly. Regular monitoring of IOP is essential after surgery.
3. Posterior Capsule Opacification (PCO):
-
PCO, also known as secondary cataracts, can develop after phacoemulsification. This condition occurs when the posterior capsule of the lens becomes cloudy. It is treatable with a YAG laser capsulotomy.
4. Graft Dislocation:
-
In rare cases, the intraocular lens may shift out of position after surgery. If this occurs, the lens may need to be repositioned or replaced.
5. Retinal Detachment:
-
Although rare, retinal detachment can occur after cataract surgery, especially in individuals who are at high risk. Symptoms of retinal detachment include sudden flashes of light or the appearance of floaters.
After phacoemulsification surgery, most patients experience a significant improvement in their vision. However, living with the condition of cataracts or recovering from cataract surgery requires ongoing care and attention:
1. Post-Operative Care:
-
After surgery, it’s important to follow all post-operative care instructions, such as using eye drops, wearing protective shields while sleeping, and avoiding strenuous activities for a few weeks.
2. Regular Follow-Up Visits:
-
Regular follow-up visits are essential to monitor the healing process and ensure there are no complications, such as infection or increased intraocular pressure.
3. Eye Protection:
-
Wearing sunglasses for UV protection and avoiding eye trauma can help protect the newly operated eye.
4. Adjusting to Clear Vision:
-
Many patients experience a period of adjustment as their brain adapts to improved vision after cataract surgery. Some people may need to adjust to new prescription glasses for near or distance vision.
1. What is phacoemulsification?
Phacoemulsification is a modern cataract surgery technique that uses ultrasound waves to break up and remove a cloudy lens (cataract) from the eye. The surgeon uses a small incision to insert a probe that emits ultrasound energy, emulsifying the cloudy lens. The emulsified lens is then aspirated out of the eye, and an artificial intraocular lens (IOL) is implanted to restore vision.
2. How does phacoemulsification work?
During phacoemulsification surgery:
-
Anesthesia: Local anesthesia (eye drops) is used to numb the eye, ensuring no pain during the procedure.
-
Incision: A small incision is made at the edge of the cornea to access the lens.
-
Ultrasound energy: The surgeon uses a small ultrasound probe to break up the cataract into tiny pieces.
-
Aspiration: The fragmented lens material is removed from the eye using suction.
-
IOL implantation: An intraocular lens (IOL) is inserted to replace the natural lens, restoring clear vision.
The entire procedure typically takes 15-30 minutes and is performed on an outpatient basis.
3. What are the benefits of phacoemulsification over traditional cataract surgery?
Phacoemulsification offers several benefits over traditional cataract surgery:
-
Smaller incision: The small incision (often self-sealing) does not require sutures, reducing recovery time and the risk of infection.
-
Faster recovery: Most patients experience quicker recovery with minimal discomfort.
-
Reduced risk of complications: The precise nature of the surgery and the use of modern technology leads to fewer complications.
-
Better outcomes: Phacoemulsification often provides excellent visual outcomes with a high success rate.
-
Preserved corneal shape: Since the surgery is minimally invasive, there is less disturbance to the corneal structure.
4. Is phacoemulsification surgery painful?
Phacoemulsification surgery is generally not painful. Local anesthesia in the form of eye drops is used to numb the eye, so the patient won’t feel pain during the procedure. Some patients may experience mild discomfort, irritation, or a sensation of pressure during or after surgery, but this typically resolves within a few hours to a few days. Post-operative eye drops are often prescribed to reduce any discomfort or inflammation.
5. How long does it take to recover after phacoemulsification surgery?
Recovery after phacoemulsification surgery is generally quick:
-
First 24-48 hours: Vision may be blurry, and some discomfort or dryness may occur.
-
1-2 weeks: Most patients return to normal activities, though it is advised to avoid heavy lifting and strenuous activities for a couple of weeks.
-
1 month: Vision stabilizes, and the eye heals fully, with follow-up visits to ensure proper healing and IOL positioning.
-
Long-term: Most patients enjoy restored vision within a few days to weeks, with the final results becoming clear after 1-2 months.
6. Are there any risks or complications with phacoemulsification surgery?
Phacoemulsification is a safe procedure with a high success rate, but like any surgery, there are some potential risks and complications, including:
-
Infection: Though rare, infections can occur, leading to inflammation or even loss of vision.
-
Intraocular pressure (IOP) increase: Pressure inside the eye may rise temporarily after surgery.
-
Posterior capsule opacification (PCO): Sometimes called a “secondary cataract,” PCO can develop after surgery, causing blurry vision. This can be treated with a laser.
-
Retinal detachment: In rare cases, the retina may detach after surgery, requiring prompt treatment.
-
IOL displacement: The intraocular lens may shift out of position, requiring additional surgery.
7. How long will the intraocular lens (IOL) last after phacoemulsification?
The intraocular lens (IOL) used in phacoemulsification is designed to be a permanent implant. Once implanted, the IOL typically lasts a lifetime and requires no maintenance or replacement. It is made from materials like silicone, acrylic, or polymethyl methacrylate (PMMA), which are durable and biocompatible. However, as the eye ages, some patients may develop posterior capsule opacification (PCO), which can cause blurry vision but can be easily treated with a laser procedure.
8. Will I need glasses after phacoemulsification surgery?
Many patients experience significantly improved vision after phacoemulsification surgery and may no longer need glasses for everyday activities. However, the need for glasses depends on the type of intraocular lens (IOL) implanted:
-
Monofocal IOLs: These provide clear vision at one specific distance (near, intermediate, or far), so reading glasses or glasses for distance may still be needed.
-
Multifocal or accommodating IOLs: These IOLs can help correct vision at multiple distances, reducing or eliminating the need for glasses.
Some patients may still need glasses for specific tasks like reading or driving at night, even with advanced IOLs.
9. How soon can I drive after phacoemulsification surgery?
Most patients are able to resume driving within 24 to 48 hours after phacoemulsification surgery, once their vision has stabilized and they feel comfortable. However, it is important to avoid driving until you have had a follow-up appointment with your ophthalmologist and have received clearance. Vision recovery can vary, so some individuals may require a few days to feel confident in their ability to drive safely.
10. How much does phacoemulsification surgery cost?
The cost of phacoemulsification surgery varies depending on factors such as the surgeon’s experience, location, and the type of intraocular lens (IOL) used. On average, the cost can range from $2,000 to $4,000 per eye. This cost typically includes the surgery itself, pre-operative and post-operative care, and follow-up visits. Insurance may cover part of the cost if the surgery is deemed medically necessary, such as for cataract removal.
These FAQs provide a comprehensive understanding of phacoemulsification surgery, addressing common concerns and offering insight into the procedure, benefits, risks, recovery, and costs. Feel free to adapt the content to fit the tone and needs of your medical website!
The other Ophthalmology Procedures are
Few Major Hospitals for Phacoemulsification are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



