Pneumatic Retinopexy (PRP) is a minimally invasive surgical procedure used to treat retinal detachment. Retinal detachment occurs when the retina, the light-sensitive layer of tissue at the back of the eye, becomes separated from its underlying support tissue. This condition can lead to permanent vision loss if not treated promptly. Pneumatic retinopexy is an effective technique for addressing small, localized retinal detachments caused by retinal tears or holes, particularly in the superior (upper) region of the retina.
During the procedure, a gas bubble is injected into the eye, which applies pressure to the detached retina and pushes it back against the wall of the eye. After the retina is repositioned, a laser or cryotherapy (freezing treatment) is used to seal the retinal tear and prevent further fluid accumulation beneath the retina. The gas bubble helps to hold the retina in place while it heals. Over time, the gas bubble is gradually absorbed by the eye, and the retina remains attached.
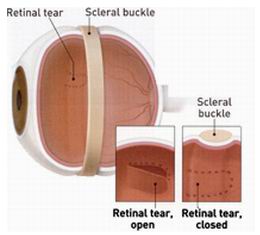
Pneumatic retinopexy is typically performed as an outpatient procedure under local anesthesia and is often preferred for small and uncomplicated retinal detachments. The procedure offers several advantages, including a shorter recovery time and the ability to avoid more invasive surgeries such as vitrectomy or scleral buckle surgery.

The need for pneumatic retinopexy arises from retinal detachment, which can occur due to a variety of causes and risk factors. Understanding these causes and risk factors can help in identifying individuals at higher risk for retinal detachment and in making decisions regarding treatment.
1. Retinal Tears and Holes
Retinal tears or holes are the primary causes of retinal detachment that can be treated with pneumatic retinopexy. A tear or hole in the retina allows fluid from the vitreous cavity (the gel-like substance in the eye) to seep underneath the retina, causing it to lift away from its underlying tissue. This fluid accumulation leads to a detached retina, which may require pneumatic retinopexy to reattach the retina.
2. Posterior Vitreous Detachment (PVD)
As people age, the vitreous gel in the eye begins to shrink and pull away from the retina, a process known as posterior vitreous detachment (PVD). PVD is a common condition, especially in individuals over 50 years old, and can lead to retinal tears, increasing the risk of retinal detachment. PVD is a significant risk factor for needing pneumatic retinopexy.
3. High Myopia (Nearsightedness)
Individuals with high myopia (severe nearsightedness) are at a higher risk for developing retinal detachment due to the elongation of the eye. This elongation puts added strain on the retina, which can lead to tears, holes, or detachment. Myopic individuals are more likely to require pneumatic retinopexy for retinal detachment treatment.
4. Trauma or Injury
Eye injuries, such as blunt force trauma or penetrating eye injuries, can cause damage to the retina and increase the likelihood of retinal detachment. Traumatic detachment often requires urgent intervention, including the possibility of pneumatic retinopexy, to restore vision and prevent permanent damage.
5. Family History and Genetics
A family history of retinal detachment or other retinal disorders can increase an individual's risk of developing retinal tears or detachments. Genetic factors may contribute to a weakened retina, making it more prone to tearing or detaching. If someone has a family member with a history of retinal problems, they may need more frequent eye exams to catch retinal detachment early.
6. Diabetic Retinopathy
Individuals with diabetic retinopathy, a complication of diabetes, are more likely to develop retinal issues that can lead to detachment. Neovascularization (the formation of new, fragile blood vessels) in the retina can cause bleeding and scarring, leading to retinal tears or detachment. Retinal detachment due to diabetic retinopathy may require pneumatic retinopexy if the detachment is limited.
7. Previous Eye Surgery
People who have undergone previous eye surgeries, such as cataract surgery or vitreoretinal surgery, may have an increased risk of retinal detachment. These surgeries can cause changes to the vitreous or retinal structures, making them more susceptible to tears or detachment.
The symptoms of retinal detachment that prompt the need for pneumatic retinopexy are usually sudden and noticeable. Individuals experiencing these symptoms should seek immediate medical attention:
1. Sudden Vision Loss
The most significant symptom of retinal detachment is sudden vision loss or blurry vision. When the retina detaches, it can no longer send clear visual signals to the brain, resulting in a rapid decrease in visual acuity, particularly in the affected eye.
2. Flashes of Light (Photopsia)
A common symptom of retinal tears and detachment is the presence of flashes of light in the field of vision, also known as photopsia. These flashes may appear suddenly, especially in the peripheral vision, and are caused by the retina being tugged by the vitreous gel as it pulls away.
3. Floaters
Individuals with retinal tears or detachment may experience an increase in floaters, which are small, shadowy spots or specks that appear in the field of vision. Floaters are typically caused by debris in the vitreous gel casting shadows on the retina. An increase in floaters, particularly if accompanied by flashes of light, warrants immediate attention.
4. Shadow or Curtain Effect
A shadow or curtain may seem to descend or move across the vision, particularly in the peripheral field. This symptom occurs when the retina begins to detach, leading to a portion of the visual field becoming obstructed. This can be a serious sign of retinal detachment.
5. Sudden Decrease in Vision
In more severe cases of retinal detachment, individuals may experience a sudden decrease in vision that affects the clarity and sharpness of vision. This often occurs when a larger portion of the retina detaches and disrupts the vision.
The diagnosis of retinal detachment and the decision to perform pneumatic retinopexy involve a series of steps to assess the eye’s condition:
1. Comprehensive Eye Examination
The ophthalmologist will conduct a detailed eye exam, including visual acuity tests, to assess the level of vision loss. A thorough examination helps determine the severity of the detachment and whether pneumatic retinopexy is appropriate.
2. Dilated Fundus Examination
In this procedure, eye drops are used to dilate the pupil, allowing the ophthalmologist to closely examine the retina for tears, holes, or detachment. The doctor looks for areas of detachment, the size and location of any tears, and the overall condition of the retina.
3. Ultrasound Imaging
If the retina is difficult to visualize due to fluid, bleeding, or other factors, ultrasound imaging may be used to examine the retina. The high-frequency sound waves create detailed images of the retina, helping the ophthalmologist assess the extent of detachment and confirm the need for pneumatic retinopexy.
4. Optical Coherence Tomography (OCT)
In certain cases, OCT may be used to capture detailed, cross-sectional images of the retina. This non-invasive imaging technique provides detailed information about the layers of the retina and helps in assessing retinal detachment, especially in cases of macula-on detachment.
The primary treatment for retinal detachment caused by tears or holes in the retina is pneumatic retinopexy. The steps involved in the procedure are:
1. Gas Bubble Injection
A small gas bubble is injected into the vitreous cavity of the eye. The gas bubble floats to the top of the eye and applies pressure on the detached retina, pushing it back into position. The bubble helps to keep the retina attached as it heals.
2. Laser or Cryotherapy
After the retina is reattached, a laser or cryotherapy (freezing) is used to seal the tear or hole in the retina. This helps prevent further fluid from entering underneath the retina and causing it to detach again. The laser creates small, precise burns around the tear, causing scar tissue to form and seal the retina in place.
3. Head Positioning
Post-operative care includes specific head positioning to ensure the gas bubble stays in the correct location, providing optimal pressure on the retina for proper reattachment. The patient may be instructed to maintain certain positions for several days to maximize the effectiveness of the treatment.
4. Follow-Up Care
Regular follow-up appointments are crucial to monitor the healing process and ensure that the retina remains attached. The ophthalmologist will monitor for complications such as increased intraocular pressure or infection.
While retinal detachment cannot always be prevented, certain steps can help minimize the risk and improve outcomes:
1. Regular Eye Exams
Regular eye exams are essential for early detection of retinal tears, holes, or other abnormalities that may lead to retinal detachment. Routine exams can identify at-risk individuals, allowing for earlier intervention.
2. Protecting the Eyes
Wearing protective eyewear during activities such as sports or work can prevent eye trauma and reduce the risk of retinal injury. Additionally, wearing sunglasses with UV protection helps prevent UV-induced retinal damage.
3. Managing Risk Factors
Managing health conditions such as diabetes and high blood pressure can help prevent retinal problems. For individuals with high myopia, regular monitoring is essential to catch retinal issues early.
Though pneumatic retinopexy is a relatively safe procedure, potential complications may arise:
1. Retinal Re-detachment
In some cases, the retina may re-detach after surgery, especially if the tear is large or not adequately sealed. This may require additional surgical intervention.
2. Infection (Endophthalmitis)
Infections within the eye, though rare, can occur after pneumatic retinopexy. Proper use of antibiotic eye drops and careful post-operative care reduces the risk of infection.
3. Increased Intraocular Pressure (IOP)
The gas bubble can cause an increase in IOP, which may lead to glaucoma if not managed properly. The ophthalmologist will monitor IOP closely after surgery.
4. Cataract Formation
Pneumatic retinopexy can sometimes lead to the development of a cataract, particularly in older individuals. If cataracts develop, further surgery may be necessary.
After pneumatic retinopexy, patients typically experience improved vision once the retina has reattached. However, there are important considerations for long-term recovery:
1. Post-Operative Care
Following the procedure, patients must adhere to the head positioning instructions and use prescribed eye drops to prevent infection and reduce inflammation. Rest and protecting the eye from trauma are essential for optimal healing.
2. Follow-Up Appointments
Regular follow-up appointments are required to monitor the progress of healing and detect any potential complications early, such as re-detachment or infection.
3. Lifestyle Adjustments
Patients should avoid strenuous activities and heavy lifting for several weeks after surgery. Additionally, wearing sunglasses with UV protection will help protect the eyes from further damage.
1. What is pneumatic retinopexy?
Pneumatic retinopexy is a minimally invasive surgical procedure used to treat retinal detachments. It involves injecting a gas bubble into the eye, which applies pressure to the retina, helping to reattach it to the back of the eye. This procedure is often used for treating certain types of retinal detachments, particularly those with a single tear or break.
2. How does pneumatic retinopexy work?
During pneumatic retinopexy:
-
Anesthesia: Local anesthesia is applied to numb the eye.
-
Gas injection: A small amount of gas is injected into the vitreous cavity of the eye.
-
Positioning: The patient is instructed to position their head in a way that allows the gas bubble to press against the detached retina, pushing it back into place.
-
Laser treatment or cryotherapy: To seal the retinal tear or break, the surgeon may use a laser or freezing treatment (cryotherapy) to help the retina adhere to the underlying tissue.
The gas bubble helps hold the retina in place while the eye heals.
3. What conditions can be treated with pneumatic retinopexy?
Pneumatic retinopexy is typically used to treat certain types of retinal detachments, especially:
-
Rhegmatogenous retinal detachment: Caused by a tear or hole in the retina, often resulting in fluid entering underneath the retina and causing it to detach.
-
Retinal tears or breaks: Especially when they are in the superior (upper) part of the retina.
This procedure is not suitable for all types of retinal detachments, and other surgical options, such as scleral buckle or vitrectomy, may be recommended depending on the complexity of the detachment.
4. Is pneumatic retinopexy painful?
Pneumatic retinopexy is not painful, as the procedure is performed under local anesthesia, which numbs the eye. You may feel slight pressure or discomfort during the gas injection, but it should not cause significant pain. After the procedure, mild discomfort or a foreign body sensation may occur, but this usually resolves within a few hours to days. Post-operative pain can typically be managed with over-the-counter pain relievers and prescribed medications.
5. What is the recovery process after pneumatic retinopexy?
The recovery process after pneumatic retinopexy is typically quick, but it requires careful adherence to instructions to ensure proper healing:
-
Head positioning: The patient may be instructed to keep their head in a specific position for several days, allowing the gas bubble to press against the retina and facilitate reattachment.
-
Vision changes: Vision may be blurry immediately after the surgery due to the gas bubble and inflammation, but this improves as the retina heals.
-
Post-operative care: Eye drops will be prescribed to prevent infection and reduce inflammation. Avoiding physical strain or heavy lifting is recommended for a few weeks.
-
Follow-up visits: Regular follow-up visits with the ophthalmologist are necessary to monitor the healing process and ensure the retina remains attached.
6. How long does it take for the gas bubble to dissipate after pneumatic retinopexy?
The gas bubble injected during pneumatic retinopexy typically takes about 2 to 6 weeks to dissipate, depending on the type of gas used. As the gas bubble slowly absorbs, vision may fluctuate during the recovery period. Patients are advised to avoid air travel and high-altitude areas during this time, as the expanding gas bubble could cause complications.
7. What are the risks and complications of pneumatic retinopexy?
While pneumatic retinopexy is generally safe, there are potential risks and complications, including:
-
Infection: Though rare, infection can occur after any surgery.
-
Increased intraocular pressure: The gas bubble can sometimes lead to elevated pressure inside the eye, requiring monitoring and treatment.
-
Re-detachment: In some cases, the retina may re-detach, necessitating further surgery.
-
Cataract formation: The procedure may contribute to cataract formation, especially in older patients.
-
Visual disturbances: Some patients may experience temporary visual disturbances, such as floaters or a shadow in their field of vision.
8. How effective is pneumatic retinopexy?
Pneumatic retinopexy has a high success rate, especially for treating uncomplicated retinal detachments with a single tear or break. Success rates are typically around 80-90%, but the procedure's effectiveness depends on factors such as the type and location of the retinal detachment, the size of the tear, and how well the patient follows post-operative instructions (such as head positioning). In some cases, additional procedures, such as laser treatment or cryotherapy, may be required to ensure the retina stays attached.
9. Can pneumatic retinopexy be performed on both eyes?
Typically, pneumatic retinopexy is performed on one eye at a time. This allows for careful monitoring and recovery of the treated eye before proceeding with treatment for the second eye, if necessary. In some cases, depending on the severity and location of retinal issues, both eyes may be treated at separate times, but it’s uncommon to treat both eyes in a single procedure.
10. Can I resume normal activities after pneumatic retinopexy?
After pneumatic retinopexy, patients are usually able to resume most normal activities within a few days to weeks, depending on their recovery. However, some restrictions apply during the initial recovery period:
-
Head positioning: The patient may need to maintain a specific head position for several days.
-
Avoid heavy physical activity: Strenuous activities, such as lifting heavy objects or exercising, should be avoided for a few weeks.
-
Driving: It is generally recommended to wait until vision stabilizes before resuming driving, which may take a few days or weeks.
Regular follow-up visits will help assess your recovery and determine when it’s safe to return to more active pursuits.
The other Ophthalmology Procedures are
Few Major Hospitals for Pneumatic Retinopexy are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



