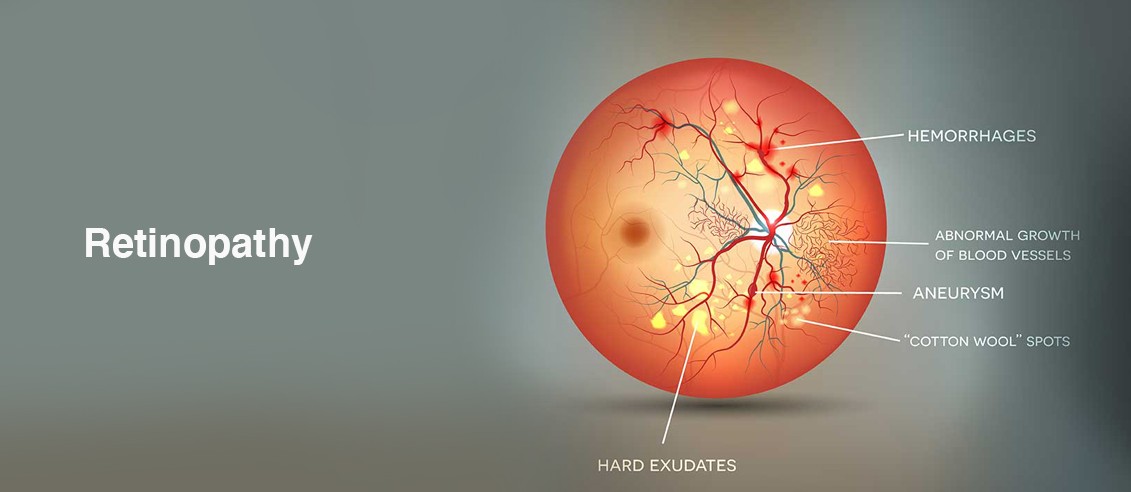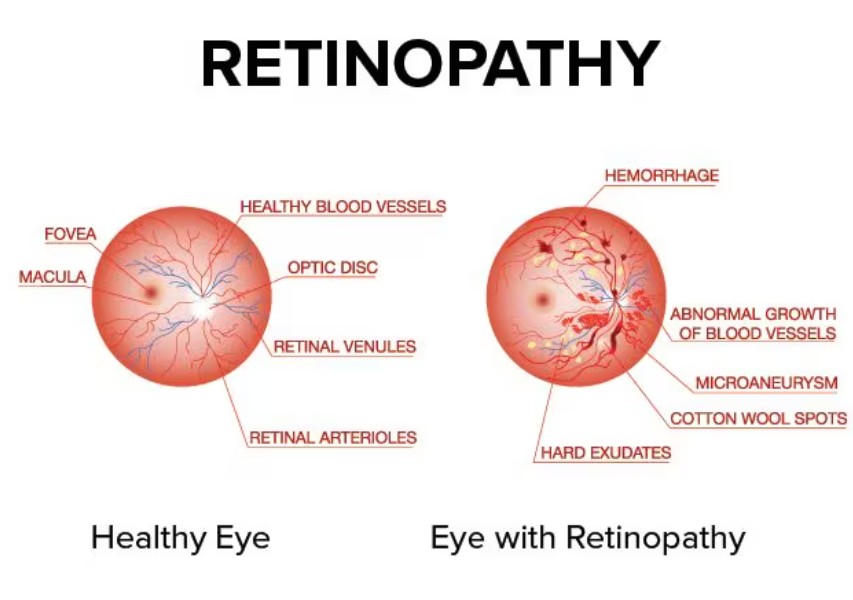
Retinopathy refers to damage or abnormalities in the retina, the light-sensitive tissue at the back of the eye responsible for capturing visual images and transmitting them to the brain via the optic nerve. When the retina becomes damaged, it can impair vision, and if left untreated, the condition can lead to permanent blindness. The term "retinopathy" broadly encompasses a variety of eye conditions that involve damage to the blood vessels in the retina, and the symptoms, causes, and treatments can vary significantly depending on the specific type of retinopathy.
The most common form of retinopathy is diabetic retinopathy, which affects individuals with diabetes. However, there are other types, such as hypertensive retinopathy, retinopathy of prematurity, and sickle cell retinopathy, among others. The condition may present with minimal symptoms in its early stages, making regular eye exams vital for early detection.
Retinopathy is a major cause of vision impairment worldwide, and with timely intervention and proper treatment, its progression can often be controlled, leading to better outcomes. Treatment depends on the cause and severity of the retinopathy, with options ranging from medications and laser therapy to surgical interventions.
The underlying causes and risk factors of retinopathy are primarily linked to vascular damage in the retina. Conditions such as diabetes, hypertension, and premature birth significantly increase the likelihood of developing retinopathy. Below are the key causes and risk factors associated with retinopathy:
1. Diabetes
Diabetic retinopathy is the most common cause of retinopathy, affecting people with both type 1 and type 2 diabetes. Chronic high blood sugar levels can damage the blood vessels in the retina, leading to leaking or blockage. Over time, new blood vessels may form (a process known as neovascularization), but these are often fragile and prone to leaking, leading to further damage to the retina. Poorly controlled diabetes, along with long duration of the disease, increases the risk of developing diabetic retinopathy.
2. Hypertension
Hypertensive retinopathy occurs when high blood pressure damages the blood vessels in the retina. It leads to narrowing, thickening, and potential leakage of these blood vessels. In severe cases, hypertensive retinopathy can cause retinal bleeding, fluid accumulation, and vision loss. Individuals with uncontrolled hypertension are at a higher risk of developing this condition.
3. Retinopathy of Prematurity
Retinopathy of prematurity (ROP) affects premature infants, especially those born before 31 weeks of gestation. In premature babies, the retinal blood vessels may not develop properly, leading to abnormal growth that can cause retinal detachment or other complications. ROP is one of the leading causes of blindness in children, but with advancements in neonatal care, its occurrence has decreased.
4. Sickle Cell Disease
Sickle cell retinopathy occurs in individuals with sickle cell disease. The condition causes the blood cells to become sickle-shaped, impairing blood flow and leading to vascular damage in the retina. This can cause hemorrhages or ischemia (lack of oxygen) in the retina, leading to vision loss over time.
5. Retinal Vein and Artery Occlusions
Retinal vein occlusion (RVO) and retinal artery occlusion (RAO) occur when the blood vessels in the retina become blocked. This can lead to retinal hemorrhages, fluid buildup, and tissue damage. Conditions such as high blood pressure, diabetes, and glaucoma increase the risk of retinal vein and artery occlusions.
6. Age
As people age, the risk of developing retinopathy, particularly diabetic retinopathy and hypertensive retinopathy, increases. Aging also increases the risk of other conditions that can lead to retinal damage, such as macular degeneration and vascular occlusions.
7. Family History and Genetics
A family history of diabetic retinopathy or other retinal diseases increases the risk of developing retinopathy. Genetic predispositions can affect how the body responds to changes in blood flow, blood pressure, and blood sugar levels, making some individuals more susceptible to retinal damage.
8. Other Medical Conditions
Several other health conditions can increase the risk of retinopathy, including:
-
Obesity
-
High cholesterol
-
Chronic kidney disease
-
Autoimmune diseases
-
Inflammatory conditions such as uveitis
In the early stages, retinopathy may not produce noticeable symptoms. As the condition progresses, it can cause a variety of visual disturbances. Common symptoms and signs include:
1. Blurred Vision
One of the most common symptoms of retinopathy is blurry vision. In diabetic retinopathy, changes in blood vessel function can lead to fluid leakage, causing the retina to become swollen, which affects the quality of vision.
2. Sudden Vision Loss
In severe cases of retinopathy, sudden or partial vision loss may occur. This can be due to retinal hemorrhages, retinal detachment, or optic nerve damage. This is particularly common in advanced stages of diabetic retinopathy and retinal vein occlusions.
3. Floaters
Floaters are small specks, threads, or shapes that appear in the field of vision, typically moving as the eyes move. These are caused by debris in the vitreous gel of the eye, which can become more noticeable in people with retinopathy.
4. Flashes of Light
Flashes of light or “lightning streaks” in the vision can occur as the retina becomes irritated or pulled during the progression of retinopathy. This symptom is most common in individuals with diabetic retinopathy or retinal detachment.
5. Distorted Vision
Individuals with advanced retinopathy may notice that straight lines appear wavy or distorted. This distortion is often due to macular edema (swelling in the central retina), which affects central vision.
6. Difficulty Seeing in Low Light
People with macular edema or damage to the retina may have difficulty seeing in dim lighting or low-light environments. This can significantly affect daily activities such as driving at night.
7. Color Vision Changes
Retinopathy can sometimes affect color perception, causing dulling of colors or difficulty distinguishing certain colors. This is often due to the damage to the macula, the part of the retina responsible for sharp central vision.
Diagnosing retinopathy involves a comprehensive eye exam and specialized tests. Early diagnosis is critical for preventing vision loss. The following diagnostic tools are typically used:
1. Comprehensive Eye Examination
An ophthalmologist will perform a thorough eye exam to assess visual acuity, pupil reflexes, and eye health. This includes examining the retina for signs of swelling, bleeding, and other abnormalities that could indicate retinopathy.
2. Dilated Fundus Examination
A fundus examination involves dilating the pupil with special eye drops, allowing the ophthalmologist to view the retina in detail. The doctor will look for signs of retinal hemorrhages, swelling, and abnormal blood vessels that are characteristic of retinopathy.
3. Optical Coherence Tomography (OCT)
OCT is a non-invasive imaging technique that produces cross-sectional images of the retina. It is commonly used to detect macular edema and measure the thickness of the retina. OCT can also be used to assess changes in the retina that may not be visible during a standard eye exam.
4. Fluorescein Angiography
Fluorescein angiography involves injecting a special dye into the bloodstream to highlight the blood vessels in the retina. A camera is then used to take images of the retina, allowing the ophthalmologist to detect areas of leakage, ischemia, or abnormal blood vessel growth.
5. Visual Field Testing
A visual field test is used to detect areas of vision loss or blind spots. This test helps assess the extent of any damage to the retina and is essential for monitoring progression in conditions like diabetic retinopathy.
The treatment for retinopathy depends on the underlying cause and the severity of the condition. The goal of treatment is to prevent further damage, preserve vision, and manage any associated health issues. Treatment options include:
1. Medications
-
Anti-VEGF injections: These are used in conditions like diabetic retinopathy and age-related macular degeneration (AMD) to inhibit vascular endothelial growth factor (VEGF), a protein that promotes the growth of abnormal blood vessels in the retina.
-
Steroid injections: These are used to reduce inflammation and swelling in the retina, especially in conditions like uveitis or diabetic macular edema.
-
Oral medications: Medications to control blood pressure, blood sugar, and cholesterol are essential for managing the underlying risk factors that contribute to retinopathy.
2. Laser Therapy
-
Laser photocoagulation: This treatment uses a laser to seal leaking blood vessels in the retina, thereby preventing further leakage and reducing swelling. It is commonly used for diabetic retinopathy and retinal vein occlusions.
-
Pan-retinal photocoagulation: This type of laser treatment is used in more advanced stages of diabetic retinopathy to shrink abnormal blood vessels and prevent further damage.
3. Vitrectomy
A vitrectomy is a surgical procedure used to treat advanced cases of retinopathy, particularly when there is severe bleeding in the vitreous gel or tractional retinal detachment. The procedure involves removing the vitreous gel and replacing it with a gas or silicone oil to help reattach the retina.
4. Cryotherapy
Cryotherapy involves freezing the tissue around retinal tears or abnormal blood vessels to prevent further leakage and encourage healing. It is often used in conjunction with laser treatment for retinal conditions.
While retinopathy cannot always be prevented, managing risk factors and adopting a proactive approach to eye health can help reduce the likelihood of developing the condition. Here are key strategies for prevention and management:
1. Regular Eye Exams
Routine eye exams are essential for the early detection of retinopathy, especially for individuals with diabetes, hypertension, or a family history of eye diseases. Early treatment can prevent vision loss and minimize complications.
2. Control Blood Sugar and Blood Pressure
Maintaining healthy blood sugar levels and managing high blood pressure are crucial for preventing diabetic retinopathy and hypertensive retinopathy. Regular monitoring and medication adherence are key to reducing the risk of eye complications.
3. Healthy Diet and Exercise
A healthy diet rich in antioxidants, vitamins, and minerals supports eye health. Regular exercise also helps control blood sugar, blood pressure, and cholesterol levels, further reducing the risk of retinopathy.
4. Avoid Smoking
Smoking increases the risk of vascular diseases, including those that affect the eyes. Quitting smoking can significantly reduce the risk of developing retinopathy and other eye conditions.
If left untreated, retinopathy can lead to several complications:
1. Vision Loss
The most significant complication of retinopathy is permanent vision loss. If the retina detaches or if there is significant damage to the macula, central vision can be lost irreversibly.
2. Diabetic Macular Edema
In diabetic retinopathy, diabetic macular edema (DME) can occur when fluid leaks into the central part of the retina, causing swelling and blurring of vision. If not treated, DME can lead to severe vision impairment.
3. Retinal Detachment
In advanced stages of retinopathy, scar tissue may cause the retina to detach, leading to significant vision loss and requiring surgical intervention to reattach the retina.
4. Glaucoma
Individuals with diabetic retinopathy or other retinal conditions are at an increased risk of developing glaucoma due to changes in the eye's internal pressure. This condition can further damage the optic nerve and lead to irreversible vision loss.
Managing retinopathy involves not only medical treatment but also making lifestyle changes to adapt to vision changes. Individuals living with retinopathy can take the following steps:
1. Follow-Up Care
Regular follow-up visits with an ophthalmologist are necessary to monitor the progression of the condition and ensure that the retina remains healthy. Early detection of complications is crucial for preserving vision.
2. Vision Aids
For individuals with vision loss, low-vision aids such as magnifiers, large-print books, or text-to-speech technology can help maintain independence in daily activities.
3. Emotional Support
Living with a chronic eye condition like retinopathy can be emotionally challenging. Support groups, counseling, or vision rehabilitation programs can provide coping strategies and improve quality of life.
1. What is retinopathy?
Retinopathy is a condition that affects the retina, the light-sensitive tissue at the back of the eye, causing damage to the blood vessels in the retina. This damage can lead to vision impairment or even blindness if not treated. The two most common types of retinopathy are diabetic retinopathy, which occurs as a result of diabetes, and hypertensive retinopathy, which is due to high blood pressure.
2. What causes retinopathy?
Retinopathy is typically caused by damage to the blood vessels in the retina. Common causes include:
-
Diabetes: High blood sugar levels can damage the blood vessels in the retina, leading to diabetic retinopathy.
-
Hypertension: High blood pressure can cause the blood vessels in the retina to constrict and leak, leading to hypertensive retinopathy.
-
Prematurity: Retinopathy of prematurity (ROP) affects premature infants and occurs due to abnormal blood vessel growth in the retina.
-
Other conditions: Retinopathy can also result from other medical conditions like high cholesterol, vascular diseases, or eye injuries.
3. What are the symptoms of retinopathy?
In the early stages, retinopathy often has no noticeable symptoms. As the condition progresses, symptoms may include:
-
Blurred or fluctuating vision.
-
Seeing floaters or spots in your field of vision.
-
Difficulty seeing at night.
-
Vision loss: In advanced stages, retinopathy can cause significant vision impairment or even blindness.
Because retinopathy often progresses without pain or obvious symptoms, regular eye exams are important, especially for people with diabetes or high blood pressure.
4. How is retinopathy diagnosed?
Retinopathy is typically diagnosed during a comprehensive eye examination, which may include:
-
Dilated eye exam: The doctor uses special eye drops to dilate the pupils and examine the retina for damage.
-
Fundus photography: A special camera takes detailed images of the retina to identify any changes or abnormalities.
-
Fluorescein angiography: A dye is injected into the bloodstream, and a camera is used to take pictures of the blood vessels in the retina to assess their condition.
-
Optical coherence tomography (OCT): This imaging technique provides detailed cross-sectional images of the retina, helping to detect any fluid buildup or damage.
5. How is retinopathy treated?
Treatment for retinopathy depends on the type and severity of the condition:
-
Diabetic retinopathy:
-
Laser therapy: Laser treatment can seal leaking blood vessels and reduce swelling in the retina.
-
Anti-VEGF injections: These injections help stop the growth of abnormal blood vessels and reduce swelling in the retina.
-
Vitrectomy: In more advanced cases, surgery may be required to remove blood or scar tissue from the vitreous gel in the eye.
-
-
Hypertensive retinopathy: The primary treatment is managing the underlying high blood pressure, which may help reduce further damage to the retina.
-
Retinopathy of prematurity (ROP): Treatment may include laser therapy or cryotherapy to prevent further damage to the retina.
6. Can retinopathy be prevented?
While not all forms of retinopathy can be prevented, there are steps you can take to reduce your risk:
-
Manage diabetes: Keep blood sugar levels within target range to reduce the risk of diabetic retinopathy.
-
Control blood pressure: Proper management of high blood pressure can prevent or slow the progression of hypertensive retinopathy.
-
Regular eye exams: If you have diabetes or high blood pressure, regular eye exams can help detect retinopathy early before it causes significant damage.
-
Healthy lifestyle: Eating a balanced diet, exercising regularly, and avoiding smoking can improve overall health and reduce the risk of retinopathy.
7. Is retinopathy a serious condition?
Retinopathy can be a serious condition if left untreated, as it can lead to permanent vision loss or blindness. Early detection and treatment are crucial for managing retinopathy and preventing further damage. The severity of the condition varies depending on the type of retinopathy, its progression, and the effectiveness of treatment.
8. Who is at risk for developing retinopathy?
People who are at higher risk for developing retinopathy include:
-
Individuals with diabetes: Diabetic retinopathy is the leading cause of blindness in adults.
-
People with high blood pressure: Hypertensive retinopathy can occur when blood pressure is poorly controlled.
-
Premature infants: Retinopathy of prematurity (ROP) is a concern for babies born prematurely.
-
Individuals with high cholesterol or a family history of vascular diseases may also be at higher risk.
Regular monitoring and early intervention can help prevent significant vision problems for these high-risk groups.
9. Can retinopathy cause blindness?
Yes, if left untreated, retinopathy can lead to permanent vision loss or blindness. In diabetic retinopathy, for example, uncontrolled blood sugar levels can cause damage to the retina over time, leading to significant vision impairment. Similarly, hypertensive retinopathy can lead to vision loss if high blood pressure is not controlled. Early detection and timely treatment can prevent severe vision loss or blindness from retinopathy.
10. How often should I have an eye exam if I have diabetes or high blood pressure?
If you have diabetes or high blood pressure, it is recommended to have a comprehensive eye exam at least once a year. More frequent exams may be necessary if you already have signs of retinopathy or if your condition is poorly controlled. Regular eye exams allow your eye doctor to detect any early signs of retinopathy and begin treatment before significant damage occurs. Early intervention is key to preserving vision.
The other Ophthalmology Procedures are
Few Major Hospitals for Retinopathy are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.