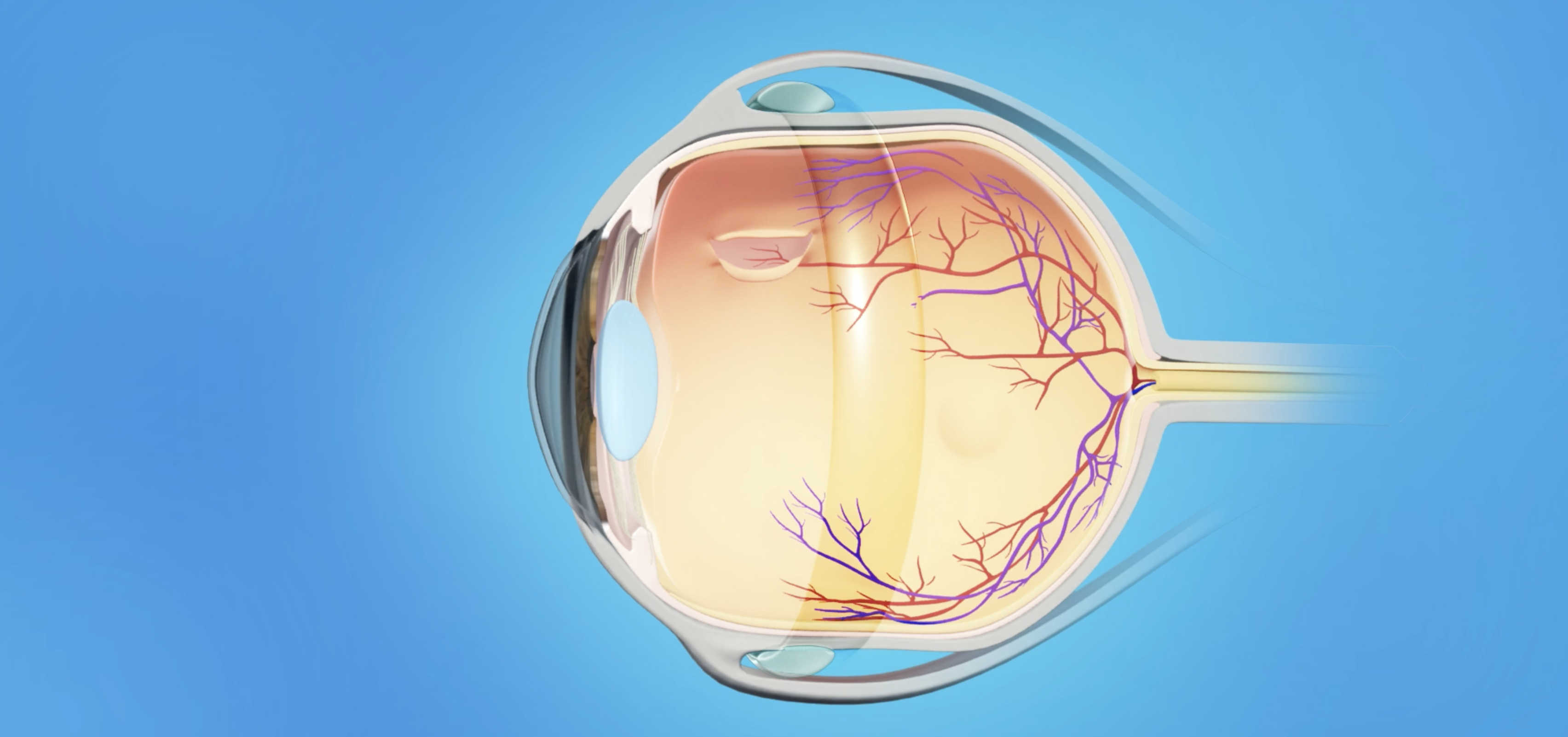
Scleral buckling surgery is a widely used procedure to treat retinal detachment, a serious eye condition where the retina becomes detached from its underlying tissue. The retina is a vital layer of the eye that captures light and sends signals to the brain to form visual images. When the retina detaches, it can cause vision loss and, if left untreated, can lead to permanent blindness. Scleral buckling surgery aims to reattach the retina to the back of the eye, restoring vision and preventing further damage.
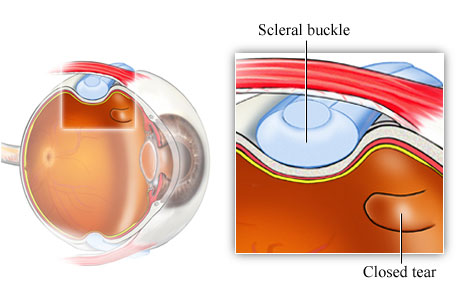
This procedure is one of the most common and effective methods for repairing rhegmatogenous retinal detachment, which is caused by a tear or hole in the retina. In scleral buckling surgery, a silicone band (also called a scleral buckle) is placed around the outside of the eye. This band gently compresses the eyeball, reducing the tension on the retina and helping it to reattach. The surgery can also involve cryotherapy (freezing treatment) or laser therapy to seal the tear in the retina and keep it in place during healing.
Scleral buckling is often performed under local anesthesia, and while it’s considered a minimally invasive procedure, it requires a skilled ophthalmic surgeon to ensure the best possible outcome. The surgery has a high success rate, but the timing of the intervention plays a critical role in its effectiveness.
Scleral buckling surgery is typically performed to treat retinal detachment, a condition that can arise from various causes and risk factors. Understanding the underlying conditions that lead to retinal detachment can help in the prevention and management of the disease. Here are some common causes and risk factors that may necessitate scleral buckling surgery:
1. Retinal Tears and Holes
The most common cause of retinal detachment that requires scleral buckling is the presence of a retinal tear or hole. These tears allow fluid from the vitreous gel (the jelly-like substance that fills the eye) to seep underneath the retina, causing it to separate from the underlying tissues. Tears are often caused by posterior vitreous detachment (PVD), which occurs naturally with aging, especially in individuals over the age of 50. The shrinking of the vitreous gel pulls on the retina, leading to tears that can cause detachment.
2. High Myopia (Nearsightedness)
People with high myopia (severe nearsightedness) are at a greater risk of retinal detachment. In these individuals, the eyeball is elongated, which places extra strain on the retina and increases the likelihood of developing retinal tears or holes. The retina of myopic individuals is also thinner and more susceptible to damage.
3. Eye Injury or Trauma
Physical trauma to the eye, such as a blow or injury from an accident, can lead to retinal detachment. Eye injuries may cause direct damage to the retina, leading to tears, holes, or even detachment. Retinal detachment resulting from trauma often requires surgical intervention, such as scleral buckling, to reattach the retina.
4. Diabetic Retinopathy
Diabetic retinopathy, a complication of diabetes, occurs when high blood sugar levels damage the blood vessels in the retina. This damage leads to the formation of abnormal blood vessels that can pull on the retina, causing retinal tears or detachment. In advanced cases of diabetic retinopathy, tractional retinal detachment can occur, and scleral buckling may be used as part of the treatment.
5. Family History and Genetic Factors
A family history of retinal detachment increases the likelihood of developing the condition. Certain genetic conditions, such as Ehlers-Danlos syndrome, Stickler syndrome, and Marfan syndrome, affect connective tissue and may increase the risk of retinal detachment, as these conditions can cause weaknesses in the retina.
6. Previous Eye Surgery
Individuals who have undergone eye surgeries, such as cataract surgery, may be at higher risk for retinal detachment, especially if there were complications during the surgery. Scleral buckling is often performed after cataract surgery if retinal detachment occurs as a complication.
7. Age and Gender
While retinal detachment can occur at any age, it is more common in individuals over the age of 50. Men are more likely to experience retinal detachment than women, particularly those with high myopia or a history of eye trauma.
Symptoms and Signs of Retinal Detachment
Retinal detachment is a serious condition that requires immediate medical attention. The symptoms of retinal detachment can vary, but common signs include:
1. Sudden Vision Loss
A key symptom of retinal detachment is sudden vision loss in one eye. This can range from partial vision loss (such as a blurred area) to complete blindness in the affected eye. If you experience a sudden loss of vision, it’s important to seek emergency medical help.
2. Flashes of Light (Photopsia)
Flashes of light, or photopsia, are a common symptom in individuals with retinal detachment. These flashes are often described as brief, lightning-like streaks of light, and they occur when the retina is tugged or pulled as a result of the detachment process.
3. Floaters
Floaters are small spots, cobweb-like lines, or threads that appear in the visual field and seem to drift as the eyes move. Floaters are common in individuals with retinal detachment and are caused by debris in the vitreous gel, which casts shadows on the retina.
4. Curtain or Shadow in the Visual Field
As retinal detachment progresses, individuals may experience a curtain-like shadow that moves across their field of vision. This shadow typically starts in the peripheral vision and can gradually cover the central vision. This is a hallmark sign of retinal detachment.
5. Wavy or Distorted Vision
In some cases, retinal detachment can cause wavy or distorted vision, especially when the macula (the central part of the retina responsible for sharp vision) is affected. Straight lines may appear curved or warped, and objects may appear out of focus.
The diagnosis of retinal detachment involves a thorough eye examination and imaging tests. Early detection is key to preventing vision loss. Common diagnostic methods include:
1. Comprehensive Eye Exam
A complete eye exam will assess visual acuity, pupil reflexes, and overall eye health. The ophthalmologist will check for any signs of retinal tears, holes, or swelling, and will inquire about the patient's symptoms (such as floaters or flashes).
2. Dilated Fundus Examination
During a dilated fundus examination, the ophthalmologist uses eye drops to widen the pupil, allowing a clearer view of the retina. This is essential for detecting retinal tears or detachment. The ophthalmologist will examine the retina for any abnormalities such as bleeding, tears, or swelling.
3. Optical Coherence Tomography (OCT)
OCT provides detailed, cross-sectional images of the retina and is helpful in diagnosing macular edema or fluid accumulation. It is often used to assess the severity of the detachment and the health of the macula.
4. Ultrasound Imaging
In cases of severe hemorrhage or cataracts that prevent a clear view of the retina, an ocular ultrasound can help determine if retinal detachment is present. Ultrasound imaging can provide detailed images of the retina and eye structures.
5. Fluorescein Angiography
Fluorescein angiography is used to examine the retinal blood vessels and detect areas of leakage, ischemia (lack of blood flow), or abnormal vessel growth. This diagnostic tool is helpful in understanding the extent of damage caused by the detachment.
Treatment for retinal detachment aims to reattach the retina and prevent further damage. The specific surgical method chosen depends on the type and severity of the detachment. The primary surgical options for retinal detachment include:
1. Scleral Buckling Surgery
Scleral buckling surgery is one of the most common treatments for retinal detachment. A silicone band is placed around the outside of the eye to compress the eyeball. This relieves the tension on the retina, encouraging it to reattach to the underlying tissue. The surgeon may also use cryotherapy (freezing) or laser therapy to seal the retinal tear or hole.
2. Vitrectomy
A vitrectomy is often used for more complex cases of retinal detachment, particularly if there is scarring or traction on the retina. During a vitrectomy, the surgeon removes the vitreous gel inside the eye, which may be pulling on the retina. The surgeon then uses a laser to seal any retinal tears and reattach the retina. A gas or silicone bubble is often inserted into the eye to help hold the retina in place.
3. Pneumatic Retinopexy
Pneumatic retinopexy is a less invasive option used for certain types of retinal detachment. A gas bubble is injected into the eye, and the patient is instructed to maintain a specific position to help the bubble push the retina back into place. A laser or cryotherapy is then used to seal the retinal tear.
4. Cryopexy
Cryopexy is used to treat retinal tears by applying extreme cold to freeze the area around the tear, creating a scar that prevents fluid from leaking underneath the retina. Cryopexy is typically used in combination with other surgical methods, such as scleral buckling or pneumatic retinopexy.
While retinal detachment cannot always be prevented, there are steps individuals can take to reduce their risk:
1. Regular Eye Exams
Routine eye exams are critical for early detection of retinal tears or signs of detachment. People with risk factors such as high myopia, a family history of retinal detachment, or diabetes should have regular eye exams.
2. Protecting the Eyes from Trauma
Wearing protective eyewear during sports, work activities, or when engaging in high-risk activities can help prevent eye injuries that could lead to retinal detachment.
3. Controlling Underlying Health Conditions
Managing health conditions such as diabetes, hypertension, and high cholesterol can reduce the risk of retinal damage. Properly controlling blood sugar levels and blood pressure can help prevent complications like diabetic retinopathy or hypertensive retinopathy.
Although scleral buckling surgery has a high success rate, there are potential complications, including:
1. Infection
Infection is a risk after any surgery. Proper post-operative care, including the use of antibiotic eye drops, is essential to minimize the risk of infection.
2. Retinal Re-detachment
In some cases, retinal detachment may recur after surgery. This is more likely if there is residual traction on the retina or if the underlying cause of the detachment is not fully addressed.
3. Cataract Formation
Cataract formation is a common complication after vitrectomy or other retinal surgeries. Cataract surgery may be required later to restore clear vision.
4. Vision Changes
Following surgery, some individuals may experience visual changes, such as reduced contrast sensitivity, distorted vision, or peripheral vision loss, depending on the extent of the detachment and the surgical procedure used.
After undergoing scleral buckling surgery, individuals can typically expect to recover with regular follow-up care and adherence to the surgeon's instructions. Key considerations for living with the condition include:
1. Post-Surgical Care
Following surgery, it is important to follow all post-operative instructions, including using prescribed eye drops, attending follow-up appointments, and avoiding heavy physical activities. Some patients may need to maintain specific head positions for a few days to ensure the retina stays in place while healing.
2. Vision Rehabilitation
In some cases, patients may need vision rehabilitation to help adjust to any permanent vision changes. This may include the use of low vision aids and adaptive techniques to assist with daily activities.
3. Emotional Support
Vision impairment can be emotionally challenging. Support groups, counseling, and vision therapy can help individuals cope with the emotional impact of retinal detachment and recovery.
1. What is scleral buckling surgery?
Scleral buckling surgery is a procedure used to treat retinal detachment, a condition where the retina becomes separated from its underlying tissue. During the surgery, a silicone band (the scleral buckle) is placed around the eye to gently press the wall of the eye inward, helping the retina reattach. The procedure may also involve freezing or using a laser to seal retinal tears. Scleral buckling is a common and effective way to restore retinal attachment and prevent further damage.
2. How does scleral buckling surgery work?
Scleral buckling surgery works by relieving the traction or pressure on the retina caused by retinal tears or detachment. The procedure involves:
-
Anesthesia: The eye is numbed with local anesthesia, and the patient may receive sedatives to relax.
-
Band placement: A silicone band (scleral buckle) is placed around the eye’s sclera (the white part of the eye). This band creates external pressure that pushes the eye wall inward, helping the retina to reattach.
-
Additional treatments: If necessary, cryotherapy (freezing) or laser treatment is applied to seal retinal tears and prevent fluid from getting underneath the retina.
-
Fluid drainage: In some cases, the surgeon may also remove the vitreous gel from the eye to reduce traction on the retina.
3. Why is scleral buckling surgery performed?
Scleral buckling surgery is primarily performed to treat rhegmatogenous retinal detachment, which occurs due to a tear or hole in the retina. The procedure is aimed at reattaching the retina to the back of the eye and preventing permanent vision loss. It is often considered for patients with retinal tears or detachments that are localized and manageable with the banding technique.
4. Is scleral buckling surgery painful?
Scleral buckling surgery is not painful, as it is performed under local anesthesia to numb the eye. Additionally, sedatives may be administered to keep the patient relaxed during the procedure. After the surgery, patients may experience mild discomfort, a feeling of pressure, or some redness in the eye, but these symptoms typically subside within a few days. Pain can generally be managed with prescribed medications.
5. How long does scleral buckling surgery take?
Scleral buckling surgery typically takes about 1 to 2 hours, depending on the complexity of the retinal detachment and whether additional treatments (such as cryotherapy or laser) are needed. The surgery is usually performed on an outpatient basis, meaning the patient can go home the same day.
6. What is the recovery process like after scleral buckling surgery?
Recovery after scleral buckling surgery generally involves:
-
First few days: Some swelling, redness, and mild discomfort may occur. Patients are usually advised to rest and avoid strenuous activities.
-
Head positioning: In some cases, the patient may be instructed to maintain a specific head position for several days to help the retina heal properly.
-
Eye protection: Patients may need to wear an eye shield to protect the eye, particularly while sleeping.
-
Follow-up visits: Multiple follow-up appointments will be scheduled to monitor healing and check for any complications.
-
Return to normal activities: Most patients can return to normal activities within 2 to 4 weeks, although heavy lifting or strenuous physical activities should be avoided for several weeks.
7. Are there any risks or complications with scleral buckling surgery?
While scleral buckling surgery is generally safe, there are potential risks and complications, including:
-
Infection: As with any surgery, there is a risk of infection, though this is rare.
-
Elevated eye pressure: Some patients may experience increased intraocular pressure after surgery, which could require additional treatment.
-
Retinal re-detachment: In some cases, the retina may detach again after surgery, necessitating further intervention.
-
Double vision: Some patients may experience temporary double vision due to the placement of the scleral buckle.
-
Bleeding or scarring: These complications are less common but can occur.
8. How effective is scleral buckling surgery?
Scleral buckling surgery is highly effective, with a success rate of approximately 80-90% in reattaching the retina and preserving vision. The procedure is particularly effective for retinal detachments caused by single tears or breaks. However, the outcome depends on factors such as the severity of the detachment, the timing of the surgery, and the overall health of the retina.
9. Will I need further treatment after scleral buckling surgery?
In many cases, no further treatment is required after scleral buckling surgery if the retina successfully reattaches. However, follow-up visits are crucial to ensure that the retina remains attached and to detect any potential complications early. In some cases, additional procedures such as vitrectomy (removal of the vitreous gel) or laser treatment may be necessary if there are any persistent problems, like recurrent retinal tears or fluid buildup.
10. Can scleral buckling surgery be performed on both eyes?
Scleral buckling surgery is usually performed on one eye at a time, especially if both eyes are affected by retinal detachment. This approach allows for proper monitoring of each eye during the recovery process. However, if necessary, both eyes can be treated in separate surgeries. Your ophthalmologist will evaluate the situation and decide the best course of action for your case.
The other Ophthalmology Procedures are
Few Major Hospitals for Scleral buckling surgery are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.