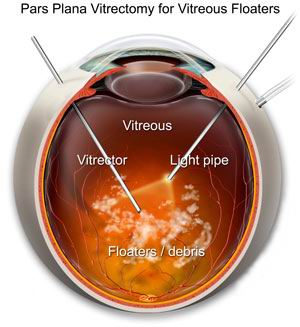
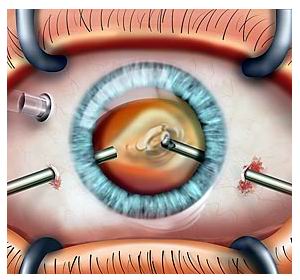
Vitrectomy is a sophisticated surgical procedure designed to treat a variety of serious eye conditions, particularly those affecting the retina and vitreous humor. The vitreous humor is a gel-like substance that fills the eye and helps maintain its shape, but when issues arise such as retinal detachment, diabetic retinopathy, macular holes, retinal bleeding, or complications from previous eye surgeries, vitrectomy can become necessary. During the procedure, a surgeon makes small incisions in the eye to remove the vitreous humor, which allows for direct access to the retina.
Once the vitreous is removed, the surgeon can address any retinal damage or complications, such as reattaching a detached retina, repairing macular holes, or removing scar tissue that may be pulling on the retina. In some cases, the space left by the removed vitreous is filled with a gas bubble, oil, or saline solution to help maintain the shape of the eye and assist in the healing process. The surgery is typically performed under local anesthesia and may take one to two hours depending on the complexity of the case.
Post-surgery recovery involves careful monitoring, eye protection, and a series of follow-up appointments to ensure proper healing and to check for any potential complications, such as infection or increased eye pressure. Although vitrectomy is highly effective in preventing vision loss and treating retinal issues, its success largely depends on the severity of the underlying eye condition and the timeliness of intervention. Many patients experience significant improvement in vision after recovery, though some may still face visual challenges depending on the extent of retinal damage prior to surgery.
Vitrectomy is performed to address various retinal and vitreous conditions that may compromise eye health and vision. Below are some of the common causes and risk factors that lead to the need for vitrectomy:
1. Retinal Detachment
Retinal detachment is one of the most common reasons for vitrectomy. In this condition, the retina becomes separated from the back of the eye, and the vitreous gel may contribute to the detachment. Vitrectomy is often performed to remove the vitreous gel and relieve the traction on the retina, helping to reattach it.
2. Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina. In severe cases, the retina may become damaged due to leakage or bleeding from abnormal blood vessels, leading to vitreous hemorrhage. Vitrectomy is commonly used to remove the blood-filled vitreous gel and treat the underlying retinal damage.
3. Macular Holes
A macular hole is a small break in the macula (the central part of the retina), which can cause significant vision problems. Vitrectomy is often used to remove the vitreous gel and apply a gas bubble to help the macula heal properly.
4. Vitreous Hemorrhage
Vitreous hemorrhage occurs when blood leaks into the vitreous gel, usually as a result of diabetic retinopathy, trauma, or retinal tears. The blood can cloud the vitreous, obstructing vision. Vitrectomy is used to remove the blood-filled vitreous gel and clear the visual pathway.
5. Retinal Tears and Traction
In some cases, retinal tears or abnormal scar tissue may form, causing traction that can pull on the retina. This leads to retinal tears, which can result in retinal detachment. Vitrectomy can address the tears and remove the vitreous gel, helping prevent further complications.
6. Eye Trauma or Infection
Infection or injury to the eye can damage the retina and vitreous. Conditions like endophthalmitis (eye infection) or trauma-induced vitreous hemorrhage may require vitrectomy for effective treatment and preservation of vision.
7. Cataract Surgery Complications
In some cases, cataract surgery can result in complications such as posterior capsule rupture or retinal detachment, leading to the need for vitrectomy to manage these issues.
8. Age and Genetics
Certain eye conditions requiring vitrectomy, such as age-related macular degeneration (AMD) or retinal degeneration, may develop as a person ages. Genetics may also play a role in conditions like macular holes or inherited retinal diseases, increasing the risk of needing vitrectomy.
The symptoms that lead to the need for vitrectomy depend on the underlying condition. However, common signs and symptoms of the conditions treated with vitrectomy include:
1. Sudden Vision Loss
One of the most common symptoms of retinal conditions such as retinal detachment, diabetic retinopathy, or macular holes is sudden vision loss. In some cases, the loss may be partial, affecting only one eye or part of the visual field.
2. Floaters
Floaters are small spots, specks, or threads that appear to float in your field of vision. These are caused by debris in the vitreous gel. In some cases, floaters are a sign of vitreous hemorrhage, which may require vitrectomy to clear the blood-filled vitreous.
3. Flashes of Light
Flashes of light (photopsia) can occur when the retina is being pulled or stretched. This may happen in conditions such as retinal detachment or vitreous traction, both of which are treated with vitrectomy.
4. Blurred or Distorted Vision
In conditions like macular holes or diabetic retinopathy, individuals may experience blurred or distorted vision. Distortion of straight lines into wavy lines is a common symptom, especially in cases of macular edema.
5. Sudden Onset of Shadows or Blind Spots
A sudden onset of a shadow or blind spot in one eye may indicate a retinal tear or detachment, both of which can require vitrectomy. The condition can progressively worsen if not treated promptly.
6. Loss of Peripheral Vision
Loss of peripheral vision, particularly in cases of retinal detachment, can occur as the retina becomes detached and unable to transmit visual information.
The diagnosis of conditions that require vitrectomy is based on a combination of symptoms, eye exams, and imaging tests. A comprehensive evaluation by an ophthalmologist is crucial for identifying the underlying condition and determining the appropriate treatment plan.
1. Comprehensive Eye Exam
A comprehensive eye exam is the first step in diagnosing the condition. The ophthalmologist will check visual acuity, eye alignment, and the health of the retina to look for signs of retinal tears, detachment, hemorrhage, or swelling.
2. Dilated Fundus Examination
A fundus examination involves dilating the pupil using special drops to allow the doctor to fully inspect the retina and vitreous for any abnormalities, including tears, holes, or signs of swelling.
3. Optical Coherence Tomography (OCT)
OCT is an imaging technique that produces cross-sectional images of the retina. It can help diagnose conditions like macular holes, macular edema, and diabetic retinopathy, which may require vitrectomy. OCT provides detailed images of the layers of the retina and helps monitor the extent of damage.
4. Fluorescein Angiography
Fluorescein angiography involves injecting a special dye into the bloodstream and using a camera to take pictures of the retina. This test is useful for detecting leaking blood vessels, particularly in conditions like diabetic retinopathy, and helps assess the need for vitrectomy.
5. B-Scan Ultrasound
If the retina is difficult to examine due to hemorrhage or cataracts, an ocular ultrasound (B-scan) can help visualize the retina and determine the extent of damage or detachment. This imaging test is particularly useful in cases of vitreous hemorrhage or when visual access to the retina is blocked.
Vitrectomy is primarily performed for the following conditions:
1. Retinal Detachment
In retinal detachment, the retina becomes separated from the back of the eye. Vitrectomy helps to remove the vitreous gel, allowing the surgeon to reattach the retina and seal any tears. A gas or silicone oil bubble may be used to help hold the retina in place during healing.
2. Diabetic Retinopathy
In diabetic retinopathy, abnormal blood vessels form in the retina, leading to bleeding or swelling. Vitrectomy can remove the vitreous gel that is filled with blood and treat the underlying retinal damage. Laser therapy may be used in combination with vitrectomy to prevent further complications.
3. Macular Hole
Vitrectomy is used to treat macular holes by removing the vitreous gel and applying a gas bubble to help close the hole. The gas bubble helps push the edges of the hole together for better healing.
4. Vitreous Hemorrhage
When blood leaks into the vitreous gel (from conditions like diabetic retinopathy), the vitreous may become cloudy, obstructing vision. Vitrectomy removes the blood-filled vitreous and clears the visual pathway.
5. Retinal Tears
If retinal tears or holes are found during the diagnosis, vitrectomy can help remove the vitreous gel and prevent further detachment by sealing the tear with a laser or cryotherapy.
Although vitrectomy cannot always prevent the conditions it treats, several steps can reduce the risk of developing retinal problems:
1. Regular Eye Exams
Regular eye exams, particularly for individuals with diabetes, hypertension, or a family history of retinal conditions, are crucial for early detection of issues that may require vitrectomy. Children and adults should have periodic eye exams to catch any potential retinal issues before they require surgical intervention.
2. Control Diabetes and Blood Pressure
Managing blood sugar levels and blood pressure can help reduce the risk of diabetic retinopathy and hypertensive retinopathy, two common causes of vitrectomy. Medications, diet, and lifestyle changes can play a significant role in keeping these conditions under control.
3. Protect Eyes from Trauma
Wearing protective eyewear when engaging in high-risk activities, such as sports or construction work, can help prevent eye injuries that may lead to retinal detachment or other conditions requiring vitrectomy.
4. Healthy Lifestyle Choices
Adopting a healthy lifestyle by eating a balanced diet, exercising regularly, and avoiding smoking can improve overall eye health and reduce the risk of conditions such as age-related macular degeneration.
Complications of Vitrectomy
As with any surgical procedure, vitrectomy carries risks and potential complications:
1. Infection
Infections can occur after any eye surgery, including vitrectomy. Proper post-surgical care, including the use of antibiotic eye drops, is essential to reduce the risk of infection.
2. Retinal Re-detachment
In some cases, retinal detachment may recur after vitrectomy, particularly if the underlying cause (such as diabetic retinopathy) continues to affect the retina. Laser therapy or additional surgery may be required to reattach the retina.
3. Cataract Formation
Vitrectomy can lead to cataract formation, especially in older adults. In some cases, cataract surgery may be required after vitrectomy.
4. Glaucoma
Glaucoma, or increased pressure in the eye, can develop after vitrectomy, particularly if silicone oil is used during the procedure. Regular eye pressure monitoring is essential after surgery.
After vitrectomy surgery, recovery can take several weeks to months, depending on the extent of the procedure and the underlying condition treated. Here are some things to consider when living with vitrectomy:
1. Post-Surgical Care
Following vitrectomy, patients must follow the ophthalmologist's post-operative care instructions, including using prescribed antibiotics and anti-inflammatory medications to prevent infection and reduce inflammation. Patients may also need to position their head in a specific way (such as face-down) to allow gas or silicone to stabilize the retina.
2. Vision Rehabilitation
Some patients may need vision rehabilitation if vision has been compromised due to the underlying condition. This may include the use of low-vision aids or working with a rehabilitation therapist.
3. Emotional and Psychological Support
Vision changes can be emotionally difficult, especially if the surgery doesn’t restore full vision. Emotional support from counselors, family, and support groups can help individuals adjust to these changes.
1. What is vitrectomy?
Vitrectomy is a surgical procedure that involves the removal of the vitreous gel (the clear, jelly-like substance inside the eye) from the interior of the eye. It is typically performed to treat a variety of retinal and vitreous conditions, such as retinal detachment, diabetic retinopathy, macular hole, and vitreous hemorrhage. The procedure allows the surgeon to access the retina for treatment and repair, followed by replacing the vitreous with a saline solution, gas, or silicone oil, depending on the condition being treated.
2. Why is vitrectomy performed?
Vitrectomy is performed to treat conditions that affect the vitreous or retina. Common reasons for undergoing a vitrectomy include:
-
Retinal detachment: When the retina becomes detached from its underlying tissue.
-
Vitreous hemorrhage: Bleeding into the vitreous cavity, often due to diabetic retinopathy or trauma.
-
Macular hole: A small break in the macula, the central part of the retina, leading to vision loss.
-
Diabetic retinopathy: When blood vessels in the retina become damaged or leak, potentially leading to retinal problems.
-
Infections or inflammation in the eye that affect the vitreous or retina.
Vitrectomy may also be used for other conditions that require direct access to the retina for treatment.
3. How does vitrectomy work?
Vitrectomy involves the following steps:
-
Anesthesia: Local or general anesthesia is administered, depending on the patient and the complexity of the surgery.
-
Incision: The surgeon makes tiny incisions in the eye to access the vitreous cavity.
-
Removal of vitreous gel: Specialized instruments are used to remove the vitreous gel from the eye.
-
Retinal repair: Depending on the condition, the surgeon may perform other procedures, such as laser treatment, to repair the retina or remove scar tissue.
-
Replacement of vitreous: After the vitreous is removed, it is replaced with a saline solution, gas bubble, or silicone oil, depending on the condition being treated.
-
Closure: The small incisions are closed, and the eye is bandaged.
4. Is vitrectomy a painful procedure?
Vitrectomy is typically not painful, as it is performed under local anesthesia, and the eye is numbed during the procedure. Patients may feel some pressure or mild discomfort during the surgery, but they should not experience significant pain. After the procedure, some soreness, swelling, and blurred vision may occur as the eye heals, but this is usually temporary and can be managed with prescribed medications and eye drops.
5. What is the recovery time after vitrectomy?
Recovery time varies by patient and the specific procedure performed, but generally:
-
First 24-48 hours: You may experience blurry vision, mild discomfort, or sensitivity to light. You should avoid any strenuous activities.
-
1-2 weeks: Swelling and redness may subside, and you may start to feel more comfortable, though vision may still be blurry.
-
1 month: The eye begins to heal, and vision should gradually improve. You may need to follow specific head positioning instructions if a gas bubble was used.
-
3-6 months: Full recovery can take up to 6 months, depending on the condition treated and the healing process. Regular follow-up visits will be necessary to monitor your progress.
6. Are there any risks or complications associated with vitrectomy?
As with any surgery, vitrectomy carries some risks, though complications are rare:
-
Infection: Any surgical procedure carries a risk of infection, which can be managed with proper post-operative care and antibiotics.
-
Increased intraocular pressure: Some patients may experience increased pressure within the eye, which can be treated.
-
Retinal detachment: In rare cases, retinal detachment can occur after surgery.
-
Cataract formation: Vitrectomy can accelerate cataract formation, especially in older patients.
-
Bleeding or scarring: There is a risk of bleeding inside the eye or scarring of the retina, which could affect vision.
-
Vision changes: Temporary visual disturbances, such as blurred vision or floaters, may occur as the eye heals.
7. How long will the effects of vitrectomy last?
The results of vitrectomy can be long-lasting, particularly if the retinal problem is treated successfully. In many cases, vision improves and stabilizes after surgery. However, some patients may require additional treatments, such as laser therapy, to address any remaining issues or prevent recurrence. If a gas bubble or silicone oil is used during surgery, it will eventually dissipate or be removed during follow-up surgery.
8. Will I need glasses after vitrectomy?
Whether you need glasses after vitrectomy depends on the underlying condition and how much vision is restored after surgery. If the vitrectomy was performed to treat a retinal problem and the eye heals properly, vision may improve significantly, reducing or eliminating the need for corrective eyewear. However, if a cataract develops after surgery, you may need glasses or contact lenses for clear vision. In some cases, patients may require glasses for specific tasks, such as reading or driving.
9. Can vitrectomy be performed on both eyes at the same time?
Vitrectomy is usually performed on one eye at a time to allow for better monitoring of the healing process and to minimize risks. However, if both eyes are affected by similar retinal issues, the surgeon may recommend performing vitrectomy on both eyes, either during separate surgeries or in one sitting, depending on the specific situation and the patient's overall health.
10. Is vitrectomy covered by insurance?
Vitrectomy is often considered medically necessary and is typically covered by insurance, especially when it is performed to treat conditions like retinal detachment, diabetic retinopathy, or vitreous hemorrhage. Insurance coverage varies by provider and plan, so it’s important to verify with your insurance company to confirm coverage details and any out-of-pocket costs that may apply. Many insurance providers will cover vitrectomy if it is deemed necessary to preserve vision and prevent further eye damage.
The other Ophthalmology Procedures are
Few Major Hospitals for Vitrectomy are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



