Heart transplantation is a surgical procedure that involves replacing a diseased, failing heart with a healthy donor heart. It is considered the gold standard for individuals with end-stage heart failure or severe coronary artery disease (CAD) when other treatment options like medications, lifestyle changes, or surgical interventions (e.g., coronary artery bypass grafting) are no longer effective. The goal of a heart transplant is to restore heart function, enhance quality of life, and significantly improve survival rates for those suffering from terminal heart disease.
Heart transplantation is a complex, high-risk procedure that requires a highly skilled surgical team, including cardiothoracic surgeons, anesthesiologists, transplant coordinators, and nurses. The donor heart is usually obtained from a deceased individual who has been declared brain-dead but whose heart remains healthy. In some cases, the transplant may involve living-related heart transplantation, but this is rare.
The transplanted heart must be a good match for the recipient’s body to reduce the risk of rejection. Immunosuppressive medications are used to prevent the body from rejecting the new heart. However, these medications carry their own risks, including infection and organ dysfunction. Post-transplant monitoring and lifelong care are essential to ensure the health of the transplanted heart.
Although heart transplantation offers a life-saving solution for patients with end-stage heart failure, the procedure carries risks, and the waiting list for a donor heart can be long, with many patients requiring medical management and possibly the use of devices such as ventricular assist devices (VADs) to support heart function until a suitable donor is found.
The need for heart transplantation is generally due to the failure of the heart to pump blood effectively, often caused by various underlying conditions. Here are the most common causes and risk factors that can lead to heart failure and ultimately require a heart transplant:
1. Coronary Artery Disease (CAD)
Coronary artery disease is the most prevalent cause of heart failure and heart transplant needs. It occurs when atherosclerosis (plaque buildup) narrows the coronary arteries, reducing blood flow to the heart muscle. Over time, this can lead to heart damage and failure. If the condition becomes severe and the heart can no longer function properly, a transplant may be required.
2. Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle that impair its ability to pump blood. There are several types of cardiomyopathy:
-
Dilated cardiomyopathy: The heart's chambers become enlarged, and the muscle weakens, making it difficult for the heart to pump effectively.
-
Hypertrophic cardiomyopathy: The heart muscle thickens, leading to a reduced ability to relax and fill with blood.
-
Restrictive cardiomyopathy: The heart becomes stiff and less able to expand, leading to heart failure.
-
Arrhythmogenic right ventricular cardiomyopathy: A rare form of cardiomyopathy where fatty or fibrous tissue replaces normal heart muscle, leading to arrhythmias and heart failure.
3. Valvular Heart Disease
Valvular heart disease is characterized by the damage or malfunctioning of the heart valves. This can lead to heart failure if untreated. Aortic stenosis, mitral regurgitation, and rheumatic heart disease can all contribute to the need for heart transplantation, particularly if heart function deteriorates due to valvular dysfunction.
4. Congenital Heart Defects
Congenital heart defects are structural heart problems present from birth. These defects can range from simple abnormalities, such as small holes in the heart, to more complex issues that prevent the heart from pumping efficiently. In severe cases, where the defect leads to heart failure, a heart transplant may be required.
5. Heart Failure Due to Uncontrolled Hypertension
Chronic high blood pressure (hypertension) is a major risk factor for heart failure. Over time, the increased pressure can cause the heart to become weakened and unable to pump blood effectively. If the condition progresses and the heart fails, a transplant may be necessary.
6. Genetic Disorders
Genetic conditions, such as familial dilated cardiomyopathy and hereditary arrhythmias, can lead to progressive heart damage and dysfunction. When the heart fails despite medical treatment, a transplant may be considered.
7. Alcohol or Drug-Induced Cardiomyopathy
Chronic alcohol abuse and the use of certain drugs (such as cocaine or chemo drugs) can contribute to cardiomyopathy, weakening the heart muscle. This can ultimately lead to heart failure, requiring heart transplantation in advanced stages.
8. End-Stage Heart Failure
In some cases, heart failure may develop as a result of a combination of factors. When the heart is no longer able to meet the body's demands and other treatment options have failed, end-stage heart failure may lead to the need for heart transplantation.
9. Inflammatory Heart Diseases
Myocarditis (inflammation of the heart muscle) caused by viral infections or autoimmune diseases can cause irreversible damage to the heart muscle, leading to heart failure. Systemic lupus erythematosus (SLE) or rheumatic fever are examples of autoimmune diseases that can cause myocarditis and eventually lead to the need for a transplant.
Heart failure is characterized by a progressive weakening of the heart's ability to pump blood, leading to various symptoms that become more severe as the condition advances. The following are common symptoms and signs that indicate the need for heart transplantation:
1. Severe Shortness of Breath
As heart failure progresses, the heart becomes unable to pump blood effectively. This causes fluid to accumulate in the lungs, leading to shortness of breath. Initially, this may occur only during exertion, but over time, it may happen even at rest, leading to significant discomfort.
2. Fatigue and Weakness
Fatigue is a hallmark symptom of heart failure. The body becomes deprived of oxygen-rich blood, leading to chronic tiredness and weakness, even after rest. Patients may feel too weak to perform daily activities and may experience a decline in quality of life.
3. Swelling in the Legs, Ankles, and Abdomen
Fluid retention occurs when the heart is unable to pump blood properly, leading to swelling (edema) in the legs, ankles, and abdomen. This swelling can be noticeable, particularly in the lower extremities, and may worsen as heart failure becomes more severe.
4. Irregular Heartbeats
Arrhythmias (irregular heartbeats) are common in heart failure and can make the heart's pumping function less efficient. These irregular rhythms can cause palpitations, dizziness, and fainting, and may require medical intervention.
5. Sudden Weight Gain
Sudden weight gain due to fluid retention is a common sign of worsening heart failure. When fluid accumulates in the body, it can lead to noticeable weight gain within a short period of time, often accompanied by increased swelling.
6. Chest Pain
Chest pain, especially in the context of coronary artery disease or previous heart attacks, can be a sign of heart failure. While chest pain is not always present, some individuals may experience it as a result of poor blood flow or ischemic heart disease.
7. Decreased Exercise Capacity
As the heart becomes weaker, individuals may experience difficulty with physical activity. Exercise intolerance is common in heart failure patients, and even mild physical exertion can lead to increased shortness of breath, fatigue, or swelling.
8. Dizziness or Fainting
Severe heart failure can lead to hypotension (low blood pressure), which may cause dizziness, lightheadedness, or fainting spells. This occurs when the heart is unable to provide adequate blood flow to the brain.
The decision to pursue heart transplantation involves several diagnostic tests and evaluations to determine the severity of heart failure and assess the patient's overall health. Common diagnostic procedures include:
1. Physical Examination
A thorough physical examination is the first step in evaluating heart failure. The doctor will assess symptoms like swelling, shortness of breath, and fatigue, and check for signs of fluid retention or irregular heart rhythms.
2. Echocardiogram
An echocardiogram is a non-invasive imaging test that uses sound waves to produce detailed images of the heart's structure and function. This test evaluates ejection fraction (the percentage of blood pumped out of the heart with each beat), valve function, and overall heart health.
3. Electrocardiogram (ECG)
An ECG records the electrical activity of the heart and helps detect arrhythmias, heart attack damage, and other electrical disturbances that may contribute to heart failure.
4. Cardiac Catheterization
Cardiac catheterization involves inserting a thin tube (catheter) into the coronary arteries to assess blood flow and detect blockages or coronary artery disease. This test helps determine whether heart disease is contributing to heart failure and the need for transplant surgery.
5. Blood Tests
Blood tests are used to assess various factors that influence heart function, such as kidney function, electrolyte balance, and inflammatory markers. Elevated levels of certain substances in the blood may indicate heart failure or other underlying conditions.
6. Stress Test
A stress test involves monitoring the heart's function during physical exertion, typically on a treadmill. This test evaluates the heart’s ability to cope with increased demand and helps assess whether heart failure is impairing the ability to perform daily activities.
7. Heart MRI and CT Scans
Imaging studies like cardiac MRI and CT scans provide detailed pictures of the heart’s structure and function. These scans are useful in evaluating heart size, valve function, and arterial health.
Heart transplantation is typically reserved for individuals with end-stage heart failure when other medical and surgical interventions are no longer effective. Several treatment options may be explored, depending on the patient’s condition and suitability for transplant:
1. Medical Management
Before a transplant, patients may be treated with medications aimed at managing heart failure symptoms. These may include:
-
ACE inhibitors, ARBs, and beta-blockers to reduce blood pressure and improve heart function.
-
Diuretics to reduce fluid buildup and alleviate swelling.
-
Anticoagulants to prevent blood clots.
-
Anti-arrhythmic drugs to stabilize abnormal heart rhythms.
2. Ventricular Assist Devices (VADs)
For patients who are not immediately eligible for a heart transplant or those waiting for a donor heart, a ventricular assist device (VAD) may be used. VADs are mechanical pumps that help the heart pump blood and act as a temporary bridge to transplant or, in some cases, long-term therapy.
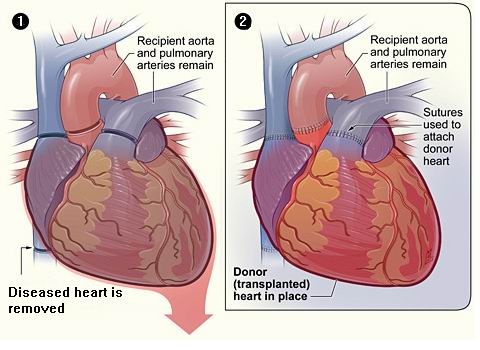
3. Heart Transplant Surgery
Heart transplant surgery involves removing the failing heart and replacing it with a healthy donor heart. The surgery requires a team of highly skilled surgeons and a careful match between the donor and recipient to minimize the risk of graft rejection.
While heart failure itself is often preventable through lifestyle modifications and early treatment, managing the progression of heart disease is crucial in preventing the need for a transplant:
-
Control Blood Pressure: Maintaining a healthy blood pressure (less than 130/80 mmHg) can significantly reduce the risk of developing heart failure.
-
Manage Cholesterol Levels: Keeping cholesterol levels in check with a healthy diet and medication can prevent coronary artery disease, which is a leading cause of heart failure.
-
Avoid Smoking and Limit Alcohol: Smoking and excessive alcohol intake both contribute to heart disease and heart failure. Quitting smoking and drinking in moderation can significantly reduce risks.
-
Regular Exercise and Healthy Diet: A balanced diet low in sodium, fat, and sugar, combined with regular physical activity, can help prevent heart disease and manage existing heart conditions.
-
Timely Treatment of Heart Disease: Early treatment of conditions like coronary artery disease, heart valve disease, and cardiomyopathy can help prevent the progression to heart failure.
While heart transplantation offers a chance at a longer life, it is not without risks and complications. These include:
-
Rejection of the Donor Heart: The body’s immune system may try to attack the transplanted heart, requiring the patient to take immunosuppressive drugs to prevent rejection.
-
Infections: Immunosuppressive therapy increases the risk of infections, including bacterial, viral, and fungal infections.
-
Coronary Artery Disease: Transplant recipients can develop coronary artery disease in the transplanted heart, known as cardiac allograft vasculopathy, which can limit the function of the new heart.
-
Organ Dysfunction: Other organs, such as the kidneys or liver, may be affected due to the long-term use of immunosuppressive medications.
-
Graft Failure: In some cases, the transplanted heart may fail to function properly, necessitating a second transplant or other interventions.
Living with a heart transplant requires long-term care and lifestyle adjustments. Patients must adhere to a strict medication regimen, undergo regular check-ups, and make adjustments to their daily habits to ensure a successful recovery.
1. Post-Transplant Care:
-
After the transplant, patients must take immunosuppressive drugs to prevent rejection, undergo regular cardiac check-ups, and follow a strict post-operative care plan.
2. Physical Rehabilitation:
-
Physical rehabilitation is essential after heart transplantation to regain strength and improve overall cardiovascular health.
3. Emotional Support:
-
The transplant journey can be emotionally challenging. Patients may require psychological support to cope with the changes in lifestyle and the stress of the transplant process.
1. What is heart transplantation?
Heart transplantation is a surgical procedure in which a patient with end-stage heart failure or severe coronary artery disease receives a healthy heart from a deceased donor. This surgery is typically performed when all other treatment options, such as medications and lifestyle changes, have failed to improve the heart’s function. The goal is to replace the diseased heart with a functional one, restoring the patient’s health and improving their quality of life.
2. Why is heart transplantation needed?
Heart transplantation is required for patients with advanced heart failure, where the heart is unable to pump enough blood to meet the body’s needs. Conditions that may lead to heart failure and require a transplant include:
-
Coronary artery disease: Narrowing of the heart arteries due to plaque buildup.
-
Dilated cardiomyopathy: Weakening and enlargement of the heart muscle.
-
Valvular heart disease: Disease of the heart valves that impairs blood flow.
-
Congenital heart defects: Severe heart defects present from birth.
-
Refractory arrhythmias: Heart rhythm problems that cannot be controlled by other treatments.
3. How is heart transplantation performed?
Heart transplantation is a complex procedure that involves:
-
Anesthesia: The patient is placed under general anesthesia to ensure they are unconscious and pain-free during the surgery.
-
Incision: A large incision is made in the chest, and the breastbone is divided to access the heart.
-
Removal of the diseased heart: The patient’s diseased heart is removed while preserving the surrounding blood vessels.
-
Implantation of the donor heart: The healthy donor heart is placed and connected to the patient’s blood vessels.
-
Closure: The chest is closed, and the patient is monitored closely in the ICU for recovery.
The surgery typically lasts 4 to 6 hours, and the patient remains in the hospital for several days to weeks, depending on their recovery.
4. How long does it take to recover from heart transplantation?
Recovery from heart transplantation varies by patient but generally involves:
-
Immediate recovery: The patient stays in the hospital for about 1 to 2 weeks for monitoring and initial recovery.
-
Post-surgical care: After discharge, recovery continues at home with follow-up visits to check heart function, manage medications, and address any complications.
-
Full recovery: It can take several months for the patient to fully recover, regain strength, and return to normal activities. Cardiac rehabilitation is often recommended to improve physical fitness and heart health.
5. What are the risks and complications of heart transplantation?
Heart transplantation carries risks and potential complications, including:
-
Rejection: The immune system may recognize the new heart as foreign and attempt to reject it, leading to inflammation. Immunosuppressive medications are prescribed to prevent rejection.
-
Infection: After surgery, the immune system is weakened, and patients are at higher risk of infections.
-
Graft coronary artery disease (GCAD): A condition where the coronary arteries of the transplanted heart become narrowed, leading to reduced blood flow.
-
Organ failure: Other organs, such as kidneys or lungs, may fail due to the strain of surgery or medication side effects.
-
Cancer: Long-term use of immunosuppressive drugs can increase the risk of developing certain types of cancer, especially skin cancer.
6. How long does a heart transplant last?
The average lifespan of a transplanted heart is about 10 to 15 years. However, some patients live much longer with a transplanted heart, especially if the heart is well-matched, the patient adheres to their post-transplant care, and the immune system doesn’t reject the heart. Advances in immunosuppressive drugs and transplant techniques have improved long-term outcomes.
7. What is the role of immunosuppressive drugs after heart transplantation?
After heart transplantation, immunosuppressive drugs are used to suppress the patient’s immune system to prevent rejection of the transplanted heart. These medications are crucial to allow the new heart to function properly and integrate with the patient’s body. However, immunosuppressive drugs increase the risk of infections, certain cancers, and other complications, so careful monitoring and adjustment of medications are necessary.
8. Can heart transplant patients resume normal activities?
Yes, most heart transplant recipients can eventually resume normal activities, including work, exercise, and leisure activities. However, the timeline varies depending on the individual’s recovery progress. It typically takes several months to regain strength and stamina. Patients are advised to follow a structured cardiac rehabilitation program to gradually rebuild physical endurance and strength. Long-term adherence to a healthy lifestyle, including proper nutrition, regular exercise, and medication management, is essential for the success of the transplant.
9. How is a suitable donor heart found?
A suitable donor heart is typically found through a matching process based on several factors:
-
Blood type: The donor and recipient must have compatible blood types.
-
Size of the heart: The donor’s heart must be an appropriate size for the recipient’s body.
-
Geographical proximity: The donor heart must be within a certain distance of the recipient to ensure it remains viable during transport.
-
Other factors: Age, medical history, and tissue matching may also be considered when matching a donor heart with a recipient.
Patients are placed on a waiting list, and when a compatible donor is available, the patient is contacted for the transplant procedure.
10. How long can a person wait for a heart transplant?
The waiting time for a heart transplant varies depending on several factors, including:
-
Availability of suitable donor hearts: There is a shortage of donor hearts, and patients are placed on a waiting list based on urgency and compatibility.
-
Patient condition: Those in more critical condition may receive priority on the waiting list.
-
Geographical factors: Waiting times can also depend on the proximity to a donor heart, as hearts must be transplanted within a specific time frame after donation.
The other Organ Transplant Procedures are
Few Major Hospitals for Heart Transplantation are
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


