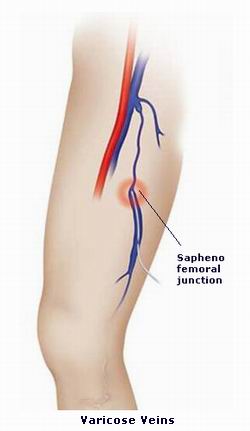
Varicose veins are swollen, twisted blood vessels that often appear on the surface of the skin. They are commonly found in the legs and feet, but can occur anywhere in the body. These veins develop when the valves in the veins, which help blood flow in one direction, become weakened or damaged. As a result, blood starts to pool in the veins, causing them to enlarge and become visible.
Varicose veins are a common issue affecting millions of people worldwide, particularly adults, especially women. Although they are often considered a cosmetic concern, varicose veins can also lead to more serious health complications such as pain, swelling, and leg ulcers. Fortunately, several effective treatments are available for managing and removing varicose veins.
Treatment for varicose veins aims to relieve symptoms, improve blood circulation, and prevent further complications. The choice of treatment depends on the severity of the condition, the patient's symptoms, and their overall health. Treatments range from non-invasive options like lifestyle changes and compression stockings to more advanced procedures like sclerotherapy, laser therapy, and surgical interventions.
Understanding the causes and risk factors for varicose veins is essential to managing the condition effectively. Several factors contribute to the development of varicose veins:
1. Age
As people age, the veins lose some of their elasticity, and the valves that prevent blood from flowing backward may weaken. This leads to blood pooling in the veins, causing them to become enlarged. Older adults are at higher risk of developing varicose veins.
2. Gender
Women are more likely to develop varicose veins than men, especially during pregnancy or due to hormonal changes related to menstruation or menopause. Estrogen, the primary female sex hormone, can weaken the vein walls and valves, making them more susceptible to varicosities.
3. Family History
If your parents or siblings had varicose veins, you may be more likely to develop them. Genetics play a significant role in the development of the condition, and inherited weaknesses in vein structure can make you more prone to varicosities.
4. Pregnancy
Pregnancy is a major risk factor for developing varicose veins. During pregnancy, the body undergoes significant hormonal changes that relax the vein walls, and the growing uterus can exert pressure on the veins in the pelvis and legs. This can cause blood to pool in the veins and lead to varicose veins, particularly in the second and third trimesters.
5. Standing or Sitting for Long Periods
People who have jobs that require them to stand or sit for long periods, such as teachers, nurses, and hairdressers, are at a higher risk of developing varicose veins. Prolonged standing or sitting reduces blood flow in the veins and increases pressure on the valves, leading to vein enlargement.
6. Obesity
Being overweight or obese places added pressure on the veins, especially in the legs, which can lead to the development of varicose veins. This excess pressure can weaken the veins over time, making them more likely to become varicose.
7. Lack of Exercise
A sedentary lifestyle and lack of physical activity can contribute to poor circulation and weakened veins. Exercise helps maintain healthy blood flow and strengthens the veins, preventing varicosities from forming.
Varicose veins may be visible on the skin as blue or purple veins, and they are often accompanied by a range of uncomfortable symptoms. While some people may have varicose veins without experiencing significant symptoms, many individuals suffer from discomfort that requires treatment.
1. Visible Swollen Veins
The most obvious sign of varicose veins is the appearance of twisted, bulging veins just beneath the surface of the skin. These veins often appear blue, purple, or flesh-colored and can be quite noticeable on the legs.
2. Aching or Heaviness in the Legs
People with varicose veins often experience a sensation of aching, heaviness, or fullness in their legs, particularly after standing or sitting for extended periods. This discomfort can be persistent and may worsen as the day goes on.
3. Swelling in the Legs or Ankles
Swelling in the legs or ankles is a common symptom of varicose veins. This swelling, also known as edema, is caused by the pooling of blood in the veins. The legs may feel tight or stiff due to the build-up of fluid.
4. Itching or Burning Sensation
In some cases, varicose veins may cause an itchy or burning sensation on or around the affected area. This is due to irritation of the skin from the swollen veins.
5. Skin Discoloration or Ulcers
In advanced cases of varicose veins, the skin around the veins may develop brownish discoloration. Venous ulcers, which are open sores on the skin, can also form in areas where blood has pooled for a prolonged period.
6. Cramps or Restlessness in the Legs
Nighttime leg cramps or an uneasy feeling in the legs, often referred to as restless legs syndrome, are common complaints in people with varicose veins. This condition can cause discomfort during sleep, making it difficult to relax or rest.
Diagnosing varicose veins typically involves a physical examination and, in some cases, additional tests to assess the extent of the condition and determine the most appropriate treatment plan.
1. Physical Examination
A doctor or vascular specialist will visually inspect the legs and other affected areas to check for visible varicose veins. The healthcare provider may also ask about the patient’s medical history, symptoms, and any contributing risk factors.
2. Duplex Ultrasound
A duplex ultrasound is a non-invasive imaging test that uses sound waves to create a detailed image of the veins. This test allows the doctor to assess blood flow in the veins, check for venous reflux (when blood flows backward due to damaged valves), and evaluate the extent of the varicose veins.
3. Venography (Rare)
In some cases, a venogram may be performed. This is an X-ray procedure where a special dye is injected into the veins to highlight the blood vessels. However, venography is rarely used today as ultrasound is more effective and non-invasive.
Several treatment options are available for varicose veins, ranging from conservative management to minimally invasive procedures and surgical interventions.
1. Conservative Treatments
-
Compression Stockings: These specialized stockings apply pressure to the legs and help improve blood circulation. They are particularly effective for mild cases of varicose veins and can reduce swelling, pain, and discomfort.
-
Lifestyle Modifications: Regular exercise, maintaining a healthy weight, and elevating the legs can help improve circulation and reduce symptoms. Avoiding prolonged standing or sitting is also recommended.
2. Sclerotherapy
Sclerotherapy is a non-surgical procedure in which a solution is injected directly into the varicose vein. The solution causes the vein to collapse and fade away over time. Sclerotherapy is effective for smaller veins and can be performed in an outpatient setting.
3. Endovenous Laser Treatment (EVLT)
Endovenous laser treatment uses a laser fiber inserted into the affected vein to heat and seal it shut. This method is effective for larger varicose veins and can be done with local anesthesia. EVLT has a high success rate and minimal recovery time.
4. Radiofrequency Ablation (RFA)
Similar to EVLT, radiofrequency ablation uses heat to close off the varicose veins. This procedure is also minimally invasive, performed under local anesthesia, and involves the insertion of a catheter into the vein.
5. Stripping and Ligation (Surgical Option)
In cases of severe varicose veins, vein stripping and ligation may be performed. This procedure involves surgically removing the affected vein through small incisions. While it is effective for large veins, it requires more recovery time compared to minimally invasive options.
Although it may not be possible to fully prevent varicose veins, there are several strategies to help reduce the risk and manage the condition.
1. Regular Exercise
Engaging in regular physical activity, such as walking, swimming, or cycling, can improve circulation and help prevent the development or worsening of varicose veins.
2. Maintain a Healthy Weight
Being overweight increases pressure on the veins in the legs. Maintaining a healthy weight can help reduce the likelihood of developing varicose veins.
3. Elevate Your Legs
Elevating your legs for 15 to 30 minutes several times a day can help reduce swelling and improve blood flow.
4. Wear Compression Stockings
Wearing compression stockings can help improve blood circulation and relieve symptoms of varicose veins, especially during long periods of standing or sitting.
While laser treatments for varicose veins are generally safe, there are potential complications to be aware of:
1. Blood Clots
In rare cases, a blood clot can form in the treated vein. This may require further treatment, such as anticoagulants, to prevent complications.
2. Skin Burns
Laser treatments and radiofrequency ablation can cause skin burns or discoloration if not performed properly.
3. Infection
As with any medical procedure, there is a slight risk of infection at the site of the treatment. Following proper aftercare instructions can minimize this risk.
4. Recurrence of Varicose Veins
In some cases, varicose veins may return after treatment, especially if lifestyle changes are not implemented to improve circulation and reduce risk factors.
Living with varicose veins can be challenging, particularly when symptoms like pain, swelling, and itching interfere with daily activities. However, with appropriate treatment and lifestyle modifications, many people can manage the condition effectively.
1. Managing Symptoms
Managing symptoms through compression stockings, exercise, and elevating the legs is essential for maintaining comfort and improving quality of life.
2. Long-Term Care
In some cases, ongoing treatments may be required to keep varicose veins under control. Regular follow-ups with your doctor will ensure that any changes in your condition are addressed promptly.
3. Emotional Well-being
For many individuals, varicose veins can impact self-esteem and body image. Consulting with a healthcare provider, joining support groups, or seeking therapy can help you cope with the emotional challenges of living with the condition.
1. What are varicose veins?
Varicose veins are enlarged, twisted veins that typically appear on the legs and feet. They occur when the valves in the veins become weakened or damaged, causing blood to pool and the veins to stretch or bulge. This condition is often characterized by visible, dark blue or purple veins, swelling, and aching in the affected area. Varicose veins can be a cosmetic concern but, in severe cases, may cause pain, discomfort, or lead to other health problems.
2. What causes varicose veins?
Varicose veins are primarily caused by weakened or damaged valves in the veins. When these valves fail, blood flow is impaired, and blood pools in the veins, causing them to enlarge and twist. Common factors contributing to varicose veins include:
-
Genetics: A family history of varicose veins increases the likelihood of developing them.
-
Aging: The risk increases as we age because the veins lose elasticity and the valves weaken.
-
Pregnancy: Hormonal changes during pregnancy can lead to increased blood flow and pressure in the veins.
-
Obesity: Extra weight puts additional pressure on the veins in the legs.
-
Prolonged standing or sitting: Jobs or activities that require standing or sitting for long periods increase the risk of varicose veins.
3. How are varicose veins treated?
Varicose veins can be treated using several methods, depending on the severity of the condition:
-
Lifestyle changes: Wearing compression stockings, elevating the legs, and regular exercise can help alleviate symptoms.
-
Sclerotherapy: A solution is injected into the varicose veins, causing them to collapse and fade over time.
-
Laser therapy: Uses laser energy to heat and close off the affected veins.
-
Endovenous laser treatment (EVLT): A minimally invasive procedure in which a laser fiber is inserted into the vein to seal it shut.
-
Vein stripping and ligation: A surgical procedure to remove large varicose veins.
-
Ambulatory phlebectomy: A procedure that removes small to medium-sized varicose veins through tiny incisions.
The treatment choice depends on the size, location, and severity of the varicose veins, as well as the patient's overall health.
4. What is the best treatment for varicose veins?
The best treatment for varicose veins depends on various factors such as the size and location of the veins, the severity of symptoms, and individual health conditions. In many cases:
-
Laser therapy or sclerotherapy is highly effective for smaller varicose veins or when the condition is more cosmetic.
-
Endovenous laser therapy (EVLT) or radiofrequency ablation is often used for larger veins, as it’s minimally invasive and has a shorter recovery time compared to traditional surgery.
-
Surgical options like vein stripping are reserved for more severe cases where other treatments have not worked.
Your doctor will recommend the most suitable treatment after a thorough evaluation of your condition.
5. Is laser treatment effective for varicose veins?
Yes, laser treatment is highly effective for treating varicose veins, especially smaller to medium-sized veins. Laser therapy uses focused light energy to heat and close the veins, causing them to collapse and be absorbed by the body. It is minimally invasive, requires no incisions, and typically involves a shorter recovery time compared to traditional surgery. Laser treatment is particularly useful for people who want a non-surgical option with fewer risks and complications.
6. Are there any risks or side effects associated with varicose vein treatments?
Like any medical procedure, varicose vein treatments come with some risks, though serious complications are rare. Possible side effects include:
-
Bruising or swelling at the treatment site.
-
Skin irritation or discoloration after sclerotherapy or laser therapy.
-
Infection: Though rare, any invasive treatment can result in infection if the area is not properly cared for.
-
Blood clots: There is a small risk of developing a blood clot in the treated vein, but this risk is minimized with proper care.
-
Nerve injury: In rare cases, nerve injury can occur, leading to temporary numbness or tingling.
Your doctor will discuss these risks with you and help you understand the potential side effects before proceeding with treatment.
7. How long does it take to recover from varicose vein treatment?
Recovery time depends on the type of treatment:
-
Laser therapy: Most patients can return to normal activities within 24 to 48 hours after treatment.
-
Sclerotherapy: After sclerotherapy, patients may experience mild swelling and bruising, but they can generally resume normal activities within 1 to 2 days.
-
Endovenous laser treatment (EVLT): Recovery time is typically 1 to 2 weeks, with most people returning to work within a few days.
-
Surgical treatments (stripping or ligation): These treatments may require a longer recovery period, with patients needing 1 to 2 weeks for initial recovery and up to 4 to 6 weeks for full healing.
Compression stockings are often recommended to help reduce swelling and improve circulation during recovery.
8. Can varicose veins come back after treatment?
While treatments like laser therapy and sclerotherapy are highly effective at eliminating the treated varicose veins, new veins can develop over time due to factors like aging, genetics, or lifestyle choices. To prevent recurrence, it is important to maintain a healthy lifestyle by:
-
Exercising regularly to improve circulation.
-
Maintaining a healthy weight to reduce pressure on the veins.
-
Avoiding prolonged sitting or standing to prevent blood from pooling in the legs.
Compression stockings can also help prevent new veins from forming.
Regular follow-up with your doctor will help monitor your condition.
9. How much does varicose vein treatment cost?
The cost of varicose vein treatments varies depending on the type of procedure, the number of veins treated, and the clinic's location. On average, the costs are as follows:
-
Laser therapy: $200 to $500 per session.
-
Sclerotherapy: $300 to $500 per session.
-
Endovenous laser treatment (EVLT): $1,500 to $3,000 per leg.
-
Vein stripping surgery: $2,000 to $4,000 per leg.
Many clinics offer package deals for multiple sessions, and some insurance plans may cover treatment if the veins cause medical symptoms or complications.
10. Are varicose vein treatments covered by insurance?
In most cases, insurance will cover varicose vein treatments if the veins are causing significant medical issues, such as pain, swelling, skin ulcers, or blood clots. However, treatments that are considered cosmetic (e.g., for appearance purposes only) may not be covered. It’s important to check with your insurance provider to determine your coverage and discuss with your doctor whether your condition qualifies for coverage.
The other Skin Procedures are:
Few Major Hospitals for Varicose Vein Treatments are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


