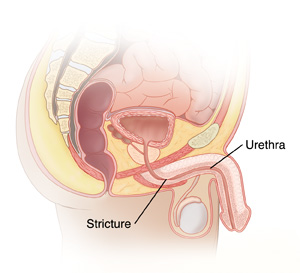
Urethroplasty is a surgical procedure used to repair or reconstruct the urethra, the tube that carries urine from the bladder out of the body. Urethroplasty is typically performed to treat urethral strictures (narrowing of the urethra), which can impede the flow of urine and cause significant complications. This procedure aims to restore normal urethral function, relieve symptoms, and improve the quality of life for patients suffering from this condition.
Urethral strictures can result from various causes, including trauma, infection, or inflammation. The procedure is usually performed under general anesthesia, and the surgeon may choose between different techniques depending on the location and severity of the stricture. These techniques may involve excising the scar tissue and reconnecting the urethra, or using a graft to reconstruct the damaged section of the urethra.
Urethroplasty is considered to be a highly effective and successful surgery, especially for long-term relief of urethral obstruction caused by strictures.
Urethral strictures are the primary reason for performing urethroplasty, and these strictures can result from several causes and risk factors. The most common causes and risk factors associated with urethral strictures are:
1. Trauma or Injury
One of the most common causes of urethral strictures is trauma or injury to the urethra. This can occur during accidents, falls, sports injuries, or pelvic fractures. Injuries that damage the urethra may cause scar tissue to form, leading to narrowing and obstruction of the urethra.
2. Infection
Chronic or untreated urinary tract infections (UTIs), gonorrhea, or chlamydia can lead to urethral scarring. Infections cause inflammation and tissue damage, which can eventually result in strictures.
3. Catheterization
Long-term use of urinary catheters, especially indwelling catheters (catheters that remain in place for extended periods), can cause urethral trauma and scarring, leading to strictures. This is particularly common in patients who require catheterization for other medical conditions.
4. Surgery or Medical Procedures
Previous surgeries involving the urethra or prostate, such as transurethral resection of the prostate (TURP) or bladder surgery, can sometimes lead to scarring and strictures. These surgeries can cause unintentional damage to the urethra, leading to the need for a urethroplasty.
**5. Inflammation and Conditions Like Lichen Sclerosus
Lichen sclerosus is a chronic skin condition that can affect the urethra, causing inflammation, scarring, and narrowing. Other inflammatory conditions may also contribute to urethral strictures.
6. Genetic Factors
Some individuals may have a genetic predisposition to developing urethral strictures. These hereditary conditions can result in an abnormal urethral structure that is more prone to scarring and narrowing.
7. Age and Gender
Older adults are more likely to develop urethral strictures due to age-related changes in the tissues of the urethra. Men are more likely to experience urethral strictures compared to women, partly due to differences in the length and anatomy of the urethra.
Urethral strictures can cause a variety of symptoms depending on the severity and location of the narrowing. The symptoms associated with urethral strictures, which may prompt the need for urethroplasty, include:
1. Difficulty Urinating
One of the most common signs of a urethral stricture is difficulty urinating, which may present as a weak urine stream or the inability to fully empty the bladder.
2. Frequent Urination
Patients may experience an increased need to urinate frequently, particularly at night (known as nocturia). The stricture can cause a partial blockage in the urethra, leading to incomplete bladder emptying.
3. Painful Urination (Dysuria)
Dysuria, or pain during urination, is another common symptom. The narrowing of the urethra can cause irritation and discomfort as urine passes through the restricted area.
4. Urinary Retention
In more severe cases, the stricture may lead to urinary retention, where the patient is unable to urinate at all. This is a medical emergency that requires immediate intervention to prevent bladder damage.
5. Blood in Urine (Hematuria)
The presence of blood in the urine can indicate that the stricture has caused damage to the urethral lining, leading to bleeding. This symptom should be evaluated promptly.
6. Pelvic or Lower Abdominal Pain
In some cases, patients with urethral strictures may experience discomfort or pain in the pelvic or lower abdominal area, particularly when attempting to urinate.
Before performing urethroplasty, a thorough diagnosis is essential to determine the presence and extent of the urethral stricture. Several diagnostic tools and tests are used to evaluate the condition:
1. Medical History and Physical Examination
The doctor will begin by taking a medical history to assess symptoms, previous urinary issues, and any potential risk factors such as prior surgeries or trauma. A physical examination may include a digital rectal exam (DRE) in men to assess prostate size and check for any tenderness.
2. Uroflowmetry
Uroflowmetry measures the rate and volume of urine flow. A decrease in urine flow rate may indicate a urinary obstruction caused by a urethral stricture.
3. Cystoscopy
Cystoscopy is a procedure where a thin, flexible tube with a camera (cystoscope) is inserted through the urethra to examine the inside of the urethra and bladder. This allows the doctor to directly visualize the location and severity of the stricture.
4. Retrograde Urethrogram
A retrograde urethrogram is an imaging test that involves injecting a contrast dye into the urethra to highlight any narrowing or blockages. X-ray images are then taken to evaluate the stricture’s location and size.
5. Urethral Dilatation
In some cases, a urethral dilatation may be performed, which involves inserting a special tool into the urethra to expand and evaluate the narrowing. This procedure helps to determine if a stricture can be treated with urethroplasty.
Urethroplasty is the main treatment for urethral strictures that do not respond to conservative treatments. There are various techniques that may be used during the procedure:
1. Direct Vision Internal Urethrotomy (DVIU)
For smaller, more superficial strictures, DVIU may be performed. This procedure involves using a special tool to cut the stricture open. It is a less invasive option compared to urethroplasty but may not be as effective for long-term results.
2. Urethral Grafting
If a large portion of the urethra is affected, a graft may be used to reconstruct the urethra. This involves taking tissue from another part of the body (such as the cheek, inner forearm, or thigh) and using it to replace the damaged section of the urethra.
3. Flap Urethroplasty
For more complex cases, a flap urethroplasty may be performed, where tissue is taken from nearby areas (like the inner cheek or scrotum) and used to cover or repair the urethral defect.
4. Stent or Catheter Placement
In some cases, a stent or catheter may be temporarily placed in the urethra to allow urine to pass through while the area heals.
5. Open Urethroplasty
In severe cases where other treatments have not been successful, an open urethroplasty may be performed. This involves a larger incision and removal of the damaged portion of the urethra, followed by reconstruction using grafts or flaps.
Preventing urethral strictures is not always possible, but some steps can reduce the risk:
1. Avoid Trauma
Avoiding pelvic injuries and taking precautions during activities that may cause trauma to the urethra can reduce the risk of strictures. Protective gear during sports can also help prevent injuries.
2. Manage Urinary Tract Infections
Timely treatment of urinary tract infections (UTIs) is important to prevent the development of urethral scarring caused by chronic infections.
3. Post-Surgical Care
Following urethroplasty, proper wound care and adherence to post-surgical instructions can prevent infection and complications. It is also important to attend regular follow-up appointments to monitor recovery.
As with any surgical procedure, urethroplasty has potential risks and complications, including:
1. Infection
Infections are a potential complication following surgery. Post-operative care, including antibiotic therapy and proper hygiene, can help minimize this risk.
2. Recurrence of Stricture
In some cases, the stricture may return even after surgery, especially if the underlying cause is not addressed. Regular follow-up and monitoring are important.
3. Urinary Incontinence
Some patients may experience urinary incontinence after surgery, which may require additional treatment, such as pelvic floor exercises or further surgery.
4. Erectile Dysfunction
In rare cases, urethroplasty can affect the nerves that control erections, leading to erectile dysfunction (ED).
After urethroplasty, patients can expect a period of recovery that may involve:
1. Rest and Rehabilitation
Post-operative rehabilitation, including pelvic floor exercises, may help restore normal bladder function and improve the chances of a successful outcome.
2. Regular Follow-Up
Routine follow-up appointments are essential to monitor for any recurrence of the stricture and assess the effectiveness of the surgery.
3. Emotional Support
Patients may benefit from emotional and psychological support to cope with any changes in sexual health or urinary function.
1. What is urethroplasty?
Urethroplasty is a surgical procedure performed to repair or reconstruct the urethra, the tube that carries urine from the bladder to the outside of the body. This procedure is typically done to treat urethral strictures, which occur when scar tissue or narrowing in the urethra obstructs urine flow. Urethroplasty aims to remove or bypass the obstructed section of the urethra, restoring normal urination.
2. Why is urethroplasty performed?
Urethroplasty is performed to treat urethral strictures caused by various factors, including:
-
Trauma or injury: Accidents or injuries to the urethra can cause scarring and narrowing.
-
Previous surgeries: Previous procedures such as catheterization or prostate surgery can lead to urethral damage and scarring.
-
Infections: Chronic urinary tract infections (UTIs) can cause scarring of the urethra.
-
Congenital conditions: Some individuals are born with abnormal urethral development that causes narrowing or blockages.
-
Inflammatory conditions: Diseases such as Lichen sclerosus or urethritis can lead to urethral scarring.
The goal of urethroplasty is to restore normal urine flow by repairing or removing the obstructed part of the urethra.
3. How is urethroplasty performed?
Urethroplasty is typically done under general or spinal anesthesia. The procedure can be performed through various techniques, depending on the location and extent of the stricture:
-
Open urethroplasty: A surgical incision is made to access the urethra, and the obstructed or damaged portion is excised. A graft may be used to reconstruct the urethra if necessary.
-
End-to-end anastomosis: The surgeon removes the narrowed segment and reconnects the two healthy ends of the urethra.
-
Graft urethroplasty: If a large portion of the urethra is affected, a tissue graft (usually taken from the cheek, forearm, or scrotum) is used to reconstruct the urethra.
The choice of technique depends on the severity and location of the stricture.
4. Is urethroplasty painful?
Urethroplasty is performed under anesthesia, so patients do not experience pain during the procedure. After surgery, some discomfort, soreness, or swelling in the genital area may occur, which can typically be managed with pain medications prescribed by the doctor. Mild burning or difficulty urinating may be experienced in the days following the surgery, but these symptoms generally improve over time. Full recovery from pain or discomfort may take a few weeks.
5. What are the risks and complications of urethroplasty?
As with any surgery, urethroplasty carries some risks and potential complications, including:
-
Infection: Infection at the surgical site or within the urinary tract.
-
Bleeding: Some bleeding during or after the procedure is common.
-
Urinary leakage: In some cases, urine may leak from the surgical site, requiring further intervention.
-
Stricture recurrence: In some cases, the urethral stricture may return after surgery.
-
Erectile dysfunction: Rarely, damage to nerves during surgery may result in erectile dysfunction.
-
Scarring: Scar tissue may form in the urethra after surgery, causing additional narrowing or complications.
Your surgeon will take measures to minimize these risks and monitor your recovery.
6. How long does it take to recover from urethroplasty?
The recovery time after urethroplasty varies based on the type of surgery and the individual’s overall health:
-
Hospital stay: Most patients stay in the hospital for 1 to 2 days after the procedure.
-
Initial recovery: Patients can generally resume light activities within 2 to 4 weeks. However, strenuous exercise and heavy lifting should be avoided for about 6 weeks.
-
Follow-up care: Follow-up visits with your urologist will be scheduled to monitor healing, assess urinary function, and check for complications.
The full recovery period can take anywhere from 6 weeks to 3 months, depending on the complexity of the surgery and healing process.
7. What are the benefits of urethroplasty?
Urethroplasty offers several benefits for patients with urethral strictures:
-
Improved urine flow: The procedure restores normal urine flow by eliminating obstructions in the urethra.
-
Increased quality of life: By addressing symptoms like frequent urination, difficulty urinating, or pain, urethroplasty improves overall comfort and health.
-
Long-term solution: Urethroplasty provides a durable, long-lasting solution for many patients, helping avoid recurring strictures or the need for repeated procedures.
-
Preservation of function: For patients with strictures caused by trauma or congenital issues, urethroplasty can restore normal function without the need for more invasive treatments like urinary diversion.
8. How effective is urethroplasty for treating urethral strictures?
Urethroplasty is a highly effective treatment for urethral strictures, particularly those caused by trauma, infection, or surgery. The success rate of the procedure varies depending on factors like the location, length of the stricture, and the patient’s overall health. In general, success rates for urethroplasty are 80% to 95%, with many patients experiencing significant improvement in urinary flow and symptom relief.
However, there is a small chance that the stricture may recur over time, especially if the procedure was more complex or if the stricture was long or located in a challenging area.
9. Are there any alternatives to urethroplasty for treating urethral strictures?
Yes, there are alternative treatments for urethral strictures, depending on the severity and location of the condition:
-
Urethral dilation: A non-surgical method where a doctor uses specialized instruments to stretch the narrowed portion of the urethra. This is typically a temporary solution and may need to be repeated.
-
Urethral stenting: A small tube (stent) is placed inside the urethra to keep it open. However, stents are often not a long-term solution.
-
Laser urethrotomy: Laser treatment can be used to cut or vaporize the stricture in certain cases, providing a minimally invasive alternative to urethroplasty.
-
Catheterization: In some cases, a catheter may be placed in the urethra to help bypass the stricture temporarily.
Urethroplasty is generally the most effective long-term solution for urethral strictures, especially when other treatments have failed.
10. How much does urethroplasty cost?
The cost of urethroplasty varies depending on factors such as the type of surgery, the healthcare facility, and geographic location. On average, the procedure may cost between $5,000 and $15,000. This includes the surgeon’s fees, anesthesia, hospital stay, and follow-up visits. Additional costs may arise if complications occur or if further treatments are required. Many insurance plans cover urethroplasty if it is deemed medically necessary, so it’s important to verify your insurance coverage beforehand.
The other Urology Procedures are:
Few Major Hospitals for Uretheroplasty are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


