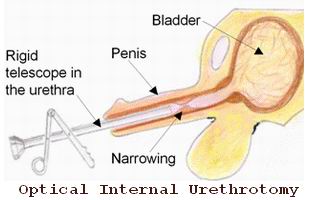
Optical Internal Urethrotomy (OTU), also known as endoscopic urethrotomy, is a minimally invasive surgical procedure used to treat urethral strictures (narrowing of the urethra) by directly visualizing and cutting or dilating the narrowed area of the urethra using a specialized tool. The procedure is performed with the aid of an endoscope, a thin, flexible tube with a camera that allows the surgeon to view the urethra and surrounding tissues.
The primary goal of OTU is to restore normal urinary flow in patients suffering from urethral strictures, which can occur in both men and women. These strictures can be caused by injury, infection, inflammation, or congenital defects, and they can lead to a range of symptoms, including urinary retention, painful urination, or difficulty in passing urine.
Unlike traditional open surgeries, endoscopic urethrotomy is performed through a small incision or natural opening (in this case, the urethra), making it a less invasive option that requires shorter recovery times and carries fewer risks.
The need for Optical Internal Urethrotomy (OTU) is generally due to urethral strictures, which are caused by various factors. Urethral strictures can occur when the tissue in the urethra scars and narrows, leading to an obstruction. Here are the common causes and risk factors that may lead to urethral strictures, and subsequently, the need for OTU:
1. Trauma or Injury
-
Physical trauma to the urethra during accidents, catheterization, or surgical procedures (such as prostate surgery or circumcision) can cause scarring, resulting in a urethral stricture.
2. Infections and Inflammation
-
Urinary tract infections (UTIs), balanitis (inflammation of the head of the penis), and urethritis (inflammation of the urethra) can lead to scarring and narrowing of the urethra.
3. Congenital Urethral Abnormalities
-
Some individuals are born with narrowing of the urethra due to congenital defects. This can result in urinary flow issues that require surgical intervention.
4. Use of Catheters
-
Long-term catheter use or repeated catheter insertions for medical procedures can cause injury or scarring in the urethra, leading to stricture formation.
5. Radiation Therapy
-
Patients who have received radiation therapy for cancers, particularly prostate cancer or pelvic cancers, may develop urethral strictures as a side effect.
6. Previous Surgery
-
Urethral strictures may develop as a complication after surgical procedures, such as prostate surgery or bladder procedures.
7. Scar Tissue Formation
-
Conditions like diabetes, autoimmune diseases, or chronic inflammatory conditions can promote scar tissue formation in the urethra, contributing to strictures.
The primary indication for undergoing OTU is the presence of urethral stricture, and the following symptoms and signs typically lead to the diagnosis:
1. Difficulty Urinating
-
One of the most common symptoms is straining to urinate, which occurs due to a narrowing of the urethra. The bladder has to work harder to push urine through the restricted area.
2. Weak Urine Stream
-
A weak or interrupted urine stream is a common symptom of urethral strictures. The urine flow may be thin or may stop and start during urination.
3. Painful Urination (Dysuria)
-
Painful urination or a burning sensation while passing urine can occur when the urethra is narrowed, causing pressure on the bladder.
4. Urinary Retention
-
In severe cases of urethral stricture, urinary retention may occur, where the patient cannot fully empty the bladder, leading to discomfort, urgency, and potentially an increased risk of urinary infections.
5. Frequent Urination
-
A narrowed urethra can cause the bladder to feel full more quickly, leading to more frequent urination, especially during the night (nocturia).
6. Blood in the Urine (Hematuria)
-
Hematuria, or blood in the urine, may occur if the urethra is inflamed or damaged by the stricture or the instruments used during diagnostic or treatment procedures.
7. Urinary Tract Infections (UTIs)
-
Chronic UTIs can develop as a result of urinary flow obstruction. Frequent UTIs with symptoms such as pain, fever, and discomfort may prompt the need for surgical intervention.
Diagnosing the need for Optical Internal Urethrotomy (OTU) involves a thorough evaluation of the patient’s symptoms, medical history, and a series of diagnostic tests:
1. Medical History and Physical Examination
-
The physician will begin by taking a detailed medical history and performing a physical examination. They will inquire about symptoms such as difficulty urinating, painful urination, or blood in the urine. A history of previous catheterization, surgeries, or trauma to the urinary tract will also be considered.
2. Urinalysis
-
A urinalysis will be performed to check for any signs of infection, blood, or other abnormalities in the urine that might suggest a urethral stricture or other urinary tract issues.
3. Uroflowmetry
-
Uroflowmetry is a non-invasive test that measures the rate and force of urine flow. A weak or interrupted stream can suggest a urethral obstruction, prompting further investigation.
4. Cystoscopy
-
Cystoscopy is a key diagnostic tool in diagnosing urethral strictures. It involves inserting a small camera (cystoscope) through the urethra to visually inspect the urethra and bladder for narrowing, scarring, or other abnormalities.
5. Retrograde Urethrogram (RUG)
-
A retrograde urethrogram is an X-ray test used to assess the length and location of a urethral stricture. It involves injecting a contrast dye into the urethra and taking X-rays to create detailed images of the urinary tract.
6. MRI or CT Scan
-
In some cases, a MRI or CT scan may be used to provide detailed images of the urinary tract, helping to evaluate the extent of the stricture and surrounding structures.
The primary treatment for urethral stricture is Optical Internal Urethrotomy (OTU), which is performed endoscopically to relieve the blockage and restore normal urinary function. Depending on the severity and location of the stricture, the following treatment options are available:
1. Optical Internal Urethrotomy (OTU)
-
In this procedure, a thin tube with a camera (hysteroscope) is inserted into the urethra. The surgeon uses specialized tools to cut the scar tissue or widen the stricture. This procedure is typically performed under local anesthesia in adults and general anesthesia in children.
2. Dilation (Balloon Dilation)
-
Balloon dilation involves the insertion of a small balloon catheter into the narrowed part of the urethra, which is inflated to widen the stricture. This is a less invasive option but may require repeated treatments.
3. Urethroplasty
-
For severe or recurrent urethral strictures, urethroplasty (surgical reconstruction of the urethra) may be necessary. This is often a more involved procedure and may be used if OTU does not provide long-term relief.
4. Stents
-
In some cases, stents (small tubes) may be inserted into the urethra to help keep the passage open while healing occurs. Stents are usually temporary.
5. Antibiotics
-
If a urinary tract infection is present, antibiotics will be prescribed before or after the procedure to prevent complications.
Preventing urethral strictures and their recurrence involves good hygiene practices, regular monitoring, and managing underlying conditions. Patients are advised to:
1. Maintain Proper Hygiene
-
Proper hygiene practices, including careful cleaning after using the restroom and ensuring good genital care, can reduce the risk of urinary infections and scarring.
2. Avoid Unnecessary Trauma
-
Avoiding unnecessary catheterization or trauma to the urethra during medical procedures helps prevent scarring. If catheters are needed, it’s important to follow healthcare provider instructions carefully.
3. Manage Chronic Conditions
-
Proper management of chronic conditions like diabetes, prostate problems, or autoimmune diseases can reduce the risk of developing strictures.
4. Regular Follow-Up
-
Regular follow-up visits with the urologist are essential to monitor healing, detect any recurrence of symptoms, and ensure that the urethra remains clear.
Although OTU is generally safe, as with any surgical procedure, there are potential risks and complications, including:
1. Infection
-
Post-surgical infections, particularly urinary tract infections, can occur. Patients may be prescribed antibiotics to prevent infection.
2. Bleeding
-
Some bleeding is common after OTU, but excessive bleeding may require additional intervention.
3. Recurrence of Stricture
-
Urethral strictures may recur after surgery, especially in cases where the stricture is long or severe. Repeat procedures or dilation may be necessary.
4. Urinary Retention
-
In some cases, temporary difficulty in urinating may occur after the procedure, requiring follow-up treatment.
After undergoing Optical Internal Urethrotomy (OTU), most patients experience a significant improvement in urinary symptoms. However, it is essential to follow post-operative care and make lifestyle adjustments to prevent complications:
1. Follow-Up Care
-
Regular follow-up appointments are crucial to monitor recovery, ensure proper healing, and detect any recurrence of symptoms.
2. Hydration and Diet
-
Staying well-hydrated helps prevent urinary tract infections and aids in the healing process. A healthy diet can promote overall well-being and help reduce the risk of infections.
3. Activity Restrictions
-
After surgery, patients may need to avoid heavy lifting or strenuous activity for a period of time to allow the urethra to heal properly.
1. What is Optical Internal Urethrotomy (OTU)?
Optical Internal Urethrotomy (OTU) is a minimally invasive endoscopic surgery used to treat urethral strictures—narrowing or scarring of the urethra that can obstruct the flow of urine. The procedure involves using an endoscope (a thin, lighted tube) to visually guide surgical instruments into the urethra. The surgeon then makes a small incision in the scar tissue or stricture using a special cutting tool to widen the urethra and improve urine flow.
2. Why is Optical Internal Urethrotomy (OTU) performed?
OTU is typically performed to treat urethral strictures, which can be caused by:
-
Injury or trauma to the urethra, such as from surgery or accidents.
-
Infections that cause scarring in the urethra.
-
Chronic catheter use, which can cause repeated trauma and scarring.
-
Congenital conditions: Some individuals are born with urethral narrowing.
-
Previous surgeries in the pelvic area that result in scarring or stricture formation.
The goal of OTU is to relieve the obstruction, allowing normal urine flow and reducing symptoms like pain, difficulty urinating, or urinary retention.
3. How is Optical Internal Urethrotomy performed?
The OTU procedure typically involves the following steps:
-
Preparation: The patient is given either local anesthesia or general anesthesia, depending on the procedure's complexity and the patient’s comfort.
-
Insertion of the endoscope: A thin, flexible tube (endoscope) is inserted through the urethra to allow the surgeon to visualize the stricture.
-
Cutting the stricture: A specialized cutting tool is passed through the endoscope, and the surgeon carefully cuts the scar tissue or narrowed part of the urethra to open it up.
-
Completion: The endoscope is removed, and the procedure is complete. A catheter may be placed temporarily to help with urine drainage during the healing process.
The procedure usually lasts 15 to 30 minutes, and patients are typically able to go home the same day.
4. Is Optical Internal Urethrotomy painful?
During the procedure, the patient is typically under anesthesia, so there is no pain. After the procedure, mild discomfort, soreness, or a burning sensation while urinating is common. Some swelling, bruising, or bleeding may occur, but these symptoms usually subside within a few days to a week. Pain relief medications can be prescribed to manage any discomfort after the procedure.
5. What are the risks and complications of Optical Internal Urethrotomy (OTU)?
As with any surgical procedure, OTU carries some risks and potential complications, including:
-
Infection: Infection at the incision site or within the urinary tract.
-
Bleeding: Some minor bleeding is common, but excessive bleeding can occur in rare cases.
-
Urinary retention: Difficulty urinating after the procedure due to swelling or incomplete opening of the stricture.
-
Recurrent stricture: The stricture may return over time, requiring additional treatments.
-
Damage to surrounding tissues: Although rare, surrounding tissues, including the bladder or urethral wall, can be inadvertently damaged during the procedure.
-
Urethral perforation: Rarely, the urethra can be perforated during the procedure, leading to more serious complications.
Your surgeon will take steps to minimize these risks and monitor your condition during the procedure and recovery.
6. How long does it take to recover from Optical Internal Urethrotomy (OTU)?
Recovery after OTU is generally quick due to the minimally invasive nature of the procedure:
-
Hospital stay: Most patients can go home the same day after the procedure.
-
Initial recovery: Mild discomfort, such as burning during urination or light bleeding, may persist for a few days.
-
Physical activity: Most patients can return to light activities within 2 to 3 days, but it’s important to avoid heavy lifting or strenuous exercise for about 1 to 2 weeks.
-
Follow-up visits: A follow-up visit is usually scheduled 1 to 2 weeks after the procedure to ensure proper healing and check for any recurrence of the stricture.
Full recovery may take 2 to 4 weeks, depending on individual healing and any complications.
7. How effective is Optical Internal Urethrotomy for treating urethral strictures?
OTU is generally an effective treatment for urethral strictures, with success rates ranging from 60% to 80% in most cases. It is particularly effective for short strictures and those caused by trauma or infection. However, the success of the procedure can vary depending on the severity and location of the stricture. In some cases, the stricture may recur, requiring repeat procedures or alternative treatments like urethral dilation or urethroplasty (surgical reconstruction of the urethra).
8. Are there any alternatives to Optical Internal Urethrotomy?
Yes, several alternatives exist for treating urethral strictures, depending on the severity of the condition:
-
Urethral dilation: A non-surgical method that involves stretching the narrowed area of the urethra using specialized instruments.
-
Urethroplasty: A more invasive procedure in which the urethra is surgically reconstructed, often used for longer or more complex strictures.
-
Stent placement: A small tube can be inserted into the urethra to keep it open, though this is generally a temporary solution.
-
Laser therapy: Lasers can be used to treat urethral strictures, especially in cases where OTU is not possible or effective.
Your urologist will recommend the best treatment option based on the location and severity of the stricture.
9. How soon can I return to normal activities after Optical Internal Urethrotomy?
Most patients can resume normal daily activities within 2 to 3 days after OTU. However, activities like sexual intercourse, heavy lifting, or strenuous exercise should be avoided for 1 to 2 weeks to ensure proper healing. Full recovery and return to all normal activities, including high-impact exercise, may take about 4 weeks. It is important to follow your doctor’s advice for the best outcome and to prevent complications.
10. How much does Optical Internal Urethrotomy cost?
The cost of Optical Internal Urethrotomy can vary depending on factors like location, the healthcare facility, and whether additional treatments or consultations are required. On average, the procedure may cost between $2,000 and $6,000, which includes the surgeon’s fees, anesthesia, hospital stay, and follow-up visits. If additional treatments, such as stent placement or follow-up procedures, are necessary, the total cost may be higher. Insurance may cover the cost if the procedure is medically necessary, so it’s important to check with your provider for specific coverage details.
Complications include:
- Urinary tract infection
- Wound infection
- Wound dehiscence
- Urethrocutaneous fistula
- Recurrence of urethral stricture
All activities are to be carefully handled. Pain would be felt for about 2 weeks for which pain medication would be given. The catheter would need to remain in place for 2 days to 2 weeks.
- Avoid lifting of heavy objects for 2 weeks.
- Ensure adequate level of fluid intake is maintained daily (approx 2 litres).
- Avoid driving for a week.
- Avoid sex for 1 week.
The other Urology Procedures are:
Few Major Hospitals for Optical Internal Urethrotomy (OTU) - (Endoscopic Surgery) are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Vasectomy Reversal | Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


