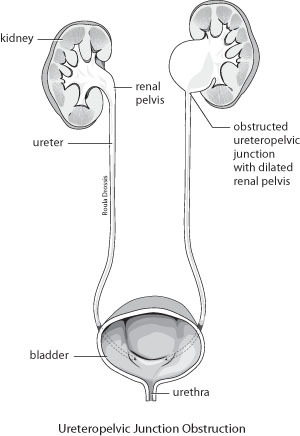
Endopyelotomy is a minimally invasive surgical procedure used to treat hydronephrosis, a condition where the kidney becomes swollen due to a backup of urine. The procedure is typically performed to relieve a blockage in the renal pelvis, the area where the kidney’s collecting system meets the ureter. When this area becomes narrowed or obstructed, urine can’t flow freely from the kidney, leading to pain, kidney damage, or infections.
Endopyelotomy is commonly used for conditions like ureteropelvic junction (UPJ) obstruction, where the connection between the ureter and the renal pelvis becomes constricted, causing a blockage. The goal of endopyelotomy is to enlarge the narrowed region of the renal pelvis or ureter to restore normal urine flow, which helps prevent further kidney damage.
This procedure offers significant advantages over traditional open surgery, including a faster recovery time, smaller incisions, and less postoperative pain. It can be performed through various techniques, including endoscopic, laparoscopic, or robotic-assisted surgery.
Endopyelotomy is used to treat conditions that cause obstructions in the renal pelvis and ureter. Understanding the causes and risk factors behind these obstructions is essential for determining who may benefit from the procedure.
1. Ureteropelvic Junction (UPJ) Obstruction
-
Congenital UPJ Obstruction: This is the most common cause of renal obstruction, particularly in children. It occurs when the junction between the kidney and the ureter doesn’t develop properly, leading to a narrowing of the passage that restricts urine flow.
-
Acquired UPJ Obstruction: In adults, UPJ obstruction can be caused by kidney stones, tumors, or scarring from previous infections or surgeries. This form of obstruction can lead to hydronephrosis and damage to the kidney.
2. Kidney Stones
Kidney stones that get lodged in the renal pelvis or ureter can lead to blockages that prevent urine from flowing properly. The presence of stones in these areas may necessitate endopyelotomy, especially when conservative treatments like stone extraction fail.
3. Scar Tissue from Previous Surgery
Scarring from prior surgical procedures, particularly abdominal or pelvic surgeries, can lead to narrowing of the renal pelvis or ureter. This condition, often called post-surgical stenosis, may require endopyelotomy to correct the blockage.
4. Infections
Chronic or recurrent urinary tract infections (UTIs) can cause scarring or inflammation in the renal pelvis and ureter, leading to obstructive conditions that may require surgical intervention.
5. Abnormalities in Kidney Development
Some individuals are born with structural abnormalities in the kidney or ureter, such as horseshoe kidneys or ectopic kidneys, which can predispose them to develop obstructions that require endopyelotomy to correct.
6. Age and Gender
-
Age: UPJ obstruction is often diagnosed in childhood but can also develop later in life. As people age, they may experience a higher incidence of acquired obstructions due to factors like kidney stones or other health issues.
-
Gender: Males are more likely to develop UPJ obstruction than females, especially in congenital cases.
Endopyelotomy is used to treat blockages and improve kidney function. The symptoms of the underlying conditions treated by this surgery are typically related to urinary retention, pain, and kidney dysfunction. Common symptoms include:
1. Flank Pain
Pain in the side or back, often on one side of the body, is one of the most common symptoms of UPJ obstruction or hydronephrosis. The pain may be intermittent or constant, depending on the severity of the blockage.
2. Swelling in the Abdomen or Flank
In severe cases, urine buildup can cause the kidney to swell, leading to noticeable bulging or discomfort in the abdomen or flank area. This swelling is often a result of hydronephrosis.
3. Nausea and Vomiting
When the kidney becomes severely swollen or infected, it can cause nausea and vomiting. These symptoms often accompany the pain and swelling associated with a urinary tract obstruction.
4. Urinary Frequency or Urgency
In some cases, patients may experience increased frequency of urination or an urgent need to urinate. However, urine flow may still be restricted due to the blockage, leading to difficulty in fully emptying the bladder.
5. Blood in the Urine (Hematuria)
In some cases of kidney obstruction or infection, blood may appear in the urine. This could be a sign of kidney stones, a urinary tract infection, or trauma to the renal structures.
6. Fever and Chills
Infections resulting from untreated urinary obstructions can lead to fever, chills, and discomfort. This is a more serious symptom that requires immediate medical attention.
Before proceeding with endopyelotomy, a healthcare provider will conduct several diagnostic tests to confirm the diagnosis of UPJ obstruction or any other conditions requiring surgery.
1. Medical History and Physical Examination
The first step is a thorough medical history review and physical examination. This includes understanding the patient's symptoms, history of kidney issues or infections, and any prior surgeries or conditions that could contribute to a blockage.
2. Imaging Tests
-
Ultrasound: An ultrasound is commonly used to assess kidney function and detect any swelling or fluid buildup in the kidneys. It can help identify hydronephrosis, the primary indication for endopyelotomy.
-
CT Scan: A CT scan with contrast can provide more detailed images of the urinary system and identify any anatomical issues, such as kidney stones, tumors, or scarring that may be contributing to the obstruction.
-
MRI: Magnetic Resonance Imaging (MRI) can also be used to provide detailed images of the kidneys and urinary tract, especially when there are concerns about soft tissue structures.
-
Intravenous Pyelogram (IVP): This test involves injecting contrast dye into the veins to visualize the kidneys, ureters, and bladder on X-rays. It is used to detect obstructions and assess the severity of the blockage.
-
Voiding Cystourethrogram (VCUG): A VCUG may be done to assess bladder function and identify any abnormalities in the urinary tract.
3. Urodynamic Studies
Urodynamics tests measure how well the bladder, sphincters, and kidneys are functioning together. These tests help determine if there is any impaired function or blockage that needs surgical intervention.
The primary goal of endopyelotomy is to alleviate the obstruction at the ureteropelvic junction and restore normal urine flow. There are several treatment options available for this condition, but endopyelotomy is generally used when less invasive methods have failed.
1. Conservative Treatments
-
Medications: For mild cases of UPJ obstruction, medications such as pain relievers or antibiotics may help manage symptoms and prevent infections.
-
Observation: In some cases, especially in children, the condition may improve over time without surgery. Doctors may recommend monitoring the situation with regular imaging studies.
-
Stent Placement: A ureteral stent is a temporary tube inserted into the ureter to hold it open and allow urine to flow. This may be used as an interim measure before endopyelotomy.
2. Endopyelotomy Procedure
The goal of endopyelotomy is to enlarge the narrowed section of the renal pelvis or ureter to restore proper urine flow. The procedure can be performed through:
-
Endoscopic Surgery: A small camera is inserted into the ureter through the bladder to guide the surgeon. Small incisions are made to allow access to the obstructed area, and a laser or scalpel is used to make the necessary incisions.
-
Laparoscopic Surgery: In some cases, minimally invasive laparoscopic techniques may be used. Small incisions are made in the abdomen, and the surgeon uses a camera and special instruments to perform the procedure.
3. Open Surgery
In rare cases, traditional open surgery may be necessary if other minimally invasive options are not suitable.
While some causes of UPJ obstruction, such as congenital issues or injuries, cannot be prevented, certain strategies can reduce the risk of complications:
1. Managing Underlying Conditions
Managing conditions like kidney stones, diabetes, and high blood pressure can help prevent additional stress on the kidneys and reduce the risk of obstructions.
2. Hydration and Diet
Staying hydrated and eating a balanced diet can help prevent kidney stones, which may contribute to obstructions. Reducing salt intake can also lower the risk of kidney damage.
3. Regular Check-Ups
After endopyelotomy, regular follow-up visits with your healthcare provider are crucial to ensure that the procedure was successful and that the obstruction does not recur.
Like any surgery, endopyelotomy has potential complications, though they are relatively rare. Some of the risks include:
1. Infection
Infections at the surgical site or in the urinary tract can occur after surgery. Proper hygiene, antibiotics, and aftercare can help reduce this risk.
2. Bleeding
There is a risk of bleeding during or after the surgery, particularly if there is damage to surrounding tissues or blood vessels.
3. Ureteral Stricture
In some cases, scar tissue may form after surgery, leading to a recurrence of the obstruction or narrowing of the ureter.
4. Urinary Leakage
Sometimes, there may be leakage of urine from the surgical site or around the stent, which may require additional interventions.
After undergoing endopyelotomy, patients will need to follow a careful post-operative recovery plan to ensure the best outcomes:
1. Post-Surgery Care:
-
Rest is important during the recovery period. Follow-up appointments will be scheduled to monitor the healing process, check for any complications, and ensure that the urinary flow has returned to normal.
2. Managing Pain:
-
Pain management is essential during the recovery period. Patients may be prescribed pain relievers to alleviate discomfort.
3. Diet and
Hydration:
-
Maintaining proper hydration and following a balanced diet are
crucial for kidney health. Low-sodium and low-oxalate diets may be recommended to prevent
the formation of kidney stones.
4.
Psychological Support:
-
The emotional and psychological impact of
recovering from surgery and
adjusting to new lifestyle changes can be significant. Patients may benefit from
support groups or
individual therapy to navigate this adjustment.
Maintaining proper hydration and following a balanced diet are crucial for kidney health. Low-sodium and low-oxalate diets may be recommended to prevent the formation of kidney stones.
The emotional and psychological impact of recovering from surgery and adjusting to new lifestyle changes can be significant. Patients may benefit from support groups or individual therapy to navigate this adjustment.
1. What is endopyelotomy?
Endopyelotomy is a minimally invasive surgical procedure used to treat pelvic-ureteric junction (PUJ) obstruction, a condition where there is a blockage between the kidney and the ureter. This obstruction can lead to pain, kidney damage, and infections. The procedure involves making small incisions and using specialized instruments, often guided by imaging techniques such as a ureteroscope, to remove or cut the blockage in the ureter, restoring proper urine flow from the kidney to the bladder.
2. What causes pelvic-ureteric junction (PUJ) obstruction?
PUJ obstruction can occur due to a variety of reasons, including:
-
Congenital abnormalities: Some individuals are born with a narrow or kinked PUJ that causes a blockage.
-
Kidney stones: Stones can form and block the flow of urine at the junction.
-
Scar tissue: Previous surgeries or infections can lead to scar tissue that causes narrowing or blockage.
-
Abnormal tissue development: In some cases, abnormal tissue growth around the PUJ can obstruct urine flow.
-
Trauma or injury: Injury to the kidney or ureter can lead to scarring or other obstructions.
In many cases, the exact cause of PUJ obstruction is not clear.
3. Who is a candidate for endopyelotomy?
Endopyelotomy is typically recommended for individuals who have:
-
Pelvic-ureteric junction (PUJ) obstruction confirmed by imaging tests, such as an ultrasound, CT scan, or MRI.
-
Symptoms of PUJ obstruction, including recurrent kidney infections, pain, and hydronephrosis (swelling of the kidney due to urine buildup).
-
Failed or unsuccessful conservative treatments (such as medication or drainage tubes) for PUJ obstruction.
-
Good overall health and the ability to tolerate a minimally invasive procedure.
Your urologist will evaluate your specific condition to determine if endopyelotomy is the right treatment option.
4. How is endopyelotomy performed?
Endopyelotomy is a minimally invasive procedure that involves:
-
Anesthesia: The patient is typically given general anesthesia to ensure they are comfortable and pain-free.
-
Access to the ureter: The surgeon inserts a thin, flexible tube called a ureteroscope through the urinary tract to reach the area of the blockage at the pelvic-ureteric junction.
-
Cutting the obstruction: Once the blockage is identified, the surgeon uses specialized instruments to either cut or remove the obstruction, such as a laser or scalpel.
-
Stent placement: In some cases, a temporary stent may be placed in the ureter to help keep the area open and promote healing.
The procedure is typically done with small incisions or sometimes through the natural urinary tract, which minimizes scarring and recovery time.
5. What are the benefits of endopyelotomy?
The main benefits of endopyelotomy include:
-
Minimally invasive: Compared to traditional open surgery, endopyelotomy involves smaller incisions and less trauma to the body.
-
Shorter recovery time: Patients typically recover faster and experience less pain post-surgery than with open surgery.
-
Reduced risk of complications: With less tissue disruption, the risk of infection, scarring, and blood loss is significantly reduced.
-
Improved kidney function: By removing the obstruction, the procedure restores proper urine flow, helping prevent kidney damage and improving overall kidney function.
-
Faster return to daily activities: Most patients can resume normal activities within a few days to a week.
6. What are the risks and complications of endopyelotomy?
While endopyelotomy is generally safe, there are potential risks and complications, including:
-
Infection: Infection can occur at the site of the incision or within the urinary tract.
-
Bleeding: Some bleeding may occur during the procedure or shortly after, but it is typically minimal.
-
Narrowing or scarring: In some cases, scar tissue may form at the site of the incision or the blockage, requiring additional treatment.
-
Injury to surrounding tissues: There is a small risk of damaging nearby structures, such as the kidney, ureter, or blood vessels.
-
Stent-related issues: If a stent is placed, it can cause discomfort, infection, or irritation.
-
Recurrent obstruction: In rare cases, the obstruction may return, requiring repeat procedures.
Your urologist will discuss these risks with you and take steps to minimize potential complications.
7. How long does it take to recover from endopyelotomy?
The recovery time after endopyelotomy is generally quick due to the minimally invasive nature of the procedure:
-
Hospital stay: Most patients are able to go home the same day or after a short hospital stay of 1 to 2 days.
-
Initial recovery: You may experience mild discomfort, swelling, or bruising for a few days to a week after the surgery.
-
Physical activity: Most patients can return to light activities within 1 to 2 weeks, but more strenuous activities should be avoided for 4 to 6 weeks.
-
Full recovery: Full recovery typically takes 1 to 2 months, depending on the extent of the procedure and individual healing.
Follow-up visits with your urologist are necessary to monitor healing and ensure proper urinary function.
8. Are there any alternative treatments to endopyelotomy?
Yes, alternative treatments for PUJ obstruction include:
-
Percutaneous nephrostomy: A tube is inserted into the kidney to drain urine, often used temporarily to relieve symptoms.
-
Stenting: In some cases, a stent is inserted into the ureter to relieve the obstruction without surgery, though this is not a long-term solution.
-
Open surgery: In rare cases, traditional open surgery may be necessary to remove or bypass the blockage.
-
Balloon dilatation: A balloon is inflated at the site of the blockage to open up the ureter, though this technique is not as commonly used as endopyelotomy.
Your urologist will discuss the best treatment options for your specific case, taking into account the severity of the condition and your overall health.
9. How effective is endopyelotomy in treating PUJ obstruction?
Endopyelotomy is highly effective in treating PUJ obstruction, with success rates typically ranging from 80% to 90%. The procedure can significantly improve urine flow, relieve symptoms such as pain and infection, and preserve kidney function. In cases where the obstruction is due to scarring or abnormal tissue, the success rate may be lower, and additional treatments may be necessary.
Follow-up visits and imaging tests after surgery help ensure the obstruction does not return and the kidney function improves.
10. How much does endopyelotomy surgery cost?
The cost of endopyelotomy surgery can vary based on factors like location, healthcare facility, and surgeon’s fees. On average, the cost of the procedure ranges from $8,000 to $15,000. This includes the surgeon’s fees, anesthesia, hospital stay, and follow-up care. Insurance typically covers the cost of the procedure if it is deemed medically necessary. Be sure to verify your insurance coverage and discuss payment options with your healthcare provider.
The other Urology Procedures are:
Few Major Hospitals for Endopyelotomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.