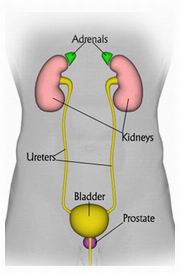
Adrenalectomy is a surgical procedure that involves the partial or complete removal of one or both adrenal glands. The adrenal glands, located above each kidney, are vital endocrine organs responsible for producing hormones such as cortisol, aldosterone, adrenaline, and noradrenaline. These hormones regulate essential bodily functions including metabolism, blood pressure, immune response, and stress adaptation.
Adrenalectomy is performed to treat a range of adrenal gland pathologies. Understanding these causes is fundamental to grasp why adrenalectomy is necessary.
1. Adrenal Tumors
- Benign Adrenal Adenomas: Non-cancerous tumors often discovered incidentally during imaging (“incidentalomas”). When hormonally active, they may cause syndromes like Cushing’s or primary aldosteronism.
- Adrenocortical Carcinoma: A rare but aggressive malignancy of adrenal cortex requiring surgical removal.
- Pheochromocytomas: Catecholamine-producing tumors originating in adrenal medulla that cause episodic hypertension, headaches, and sweating.
2. Primary Hyperaldosteronism (Conn’s Syndrome)
Caused by aldosterone-producing adenomas or bilateral adrenal hyperplasia, leading to uncontrolled hypertension and low potassium.
3. Cushing’s Syndrome
Excess cortisol production due to adrenal adenomas, hyperplasia, or carcinomas, causing characteristic features such as central obesity, skin changes, and metabolic disturbances.
4. Congenital Adrenal Hyperplasia
A genetic disorder leading to enzyme deficiencies affecting cortisol production and adrenal enlargement.
5. Metastatic Disease
Adrenal glands are common metastatic sites for cancers such as lung, breast, melanoma, and renal cell carcinoma. Adrenalectomy may be part of curative or palliative management.
6. Adrenal Hemorrhage or Trauma
Rare indications include removing necrotic or damaged adrenal tissue post-injury.
The clinical presentation varies based on the underlying adrenal pathology:
Hormone Excess Syndromes
- Cushing’s Syndrome: Weight gain (especially trunk and face), hypertension, glucose intolerance, muscle weakness, osteoporosis, skin thinning, bruising, and psychological changes.
- Primary Hyperaldosteronism: Persistent high blood pressure resistant to medication, muscle weakness, fatigue due to hypokalemia.
- Pheochromocytoma: Paroxysmal hypertension, severe headaches, palpitations, sweating episodes, anxiety.
- Androgen/Estrogen Excess: Virilization in females, menstrual irregularities, feminization in males.
Mass Effect Symptoms
- Flank or abdominal pain if the tumor grows large.
- Palpable abdominal mass (rare).
Incidentalomas
Often asymptomatic; discovered incidentally during imaging for unrelated reasons.
Diagnosing adrenal disorders is multi-faceted, combining clinical, biochemical, and imaging data:
1. Clinical Evaluation
Detailed history and physical exam focusing on signs of hormone excess and hypertension.
2. Laboratory and Hormonal Tests
- Serum cortisol levels and dexamethasone suppression test for Cushing’s.
- Plasma aldosterone and renin ratio for primary aldosteronism.
- Plasma-free metanephrines and normetanephrines for pheochromocytoma.
- 24-hour urine collections for catecholamines or cortisol.
- Electrolyte panels detecting hypokalemia.
3. Imaging Studies
- CT Scan: Primary modality to characterize adrenal masses, evaluate size, shape, and density.
- MRI: Useful for pheochromocytoma and differentiating benign from malignant lesions.
- MIBG Scintigraphy: Functional imaging to localize pheochromocytomas.
- PET Scan: For malignancy evaluation and metastatic disease staging.
4. Adrenal Vein Sampling
Gold standard for lateralizing aldosterone secretion in primary aldosteronism to guide unilateral adrenalectomy.
5. Histopathology
Postoperative tissue analysis confirms diagnosis and tumor characteristics.
Medical Management
Before surgery, medical optimization is critical, especially for hormone-producing tumors:
- Alpha-blockers and beta-blockers for pheochromocytoma to control blood pressure.
- Correcting electrolyte imbalances in primary aldosteronism.
- Managing hypercortisolism symptoms.
Surgical Techniques
- Laparoscopic Adrenalectomy: Minimally invasive approach with smaller incisions, faster recovery, and less pain. Preferred for benign and small malignant tumors (6 cm) .
- Robotic Adrenalectomy: An advanced laparoscopic method providing enhanced dexterity and visualization.
- Open Adrenalectomy: Reserved for large tumors, invasive carcinomas, or when malignancy is suspected.
- Partial Adrenalectomy: For bilateral disease to preserve adrenal function.
Postoperative Care
- Monitoring for adrenal insufficiency.
- Hormone replacement therapy if bilateral removal performed.
- Pain management and wound care.
- Early mobilization to prevent thromboembolism.
While many adrenal disorders cannot be fully prevented, timely diagnosis and management reduce morbidity:
- Routine screening in hypertensive patients resistant to treatment.
- Genetic counseling and testing in familial syndromes.
- Avoiding exogenous steroids misuse.
- Regular follow-up imaging for known adrenal incidentalomas.
- Lifestyle modifications addressing cardiovascular risk factors.
Despite advances, adrenalectomy has inherent risks:
- Intraoperative Bleeding: Due to rich vascular supply.
- Injury to Nearby Organs: Kidney, pancreas, spleen, liver.
- Adrenal Insufficiency: Especially after bilateral adrenalectomy.
- Infection and Wound Healing Issues
- Hormonal Imbalance: Temporary or permanent.
- Thromboembolic Events: Deep vein thrombosis or pulmonary embolism.
- Pheochromocytoma Crisis: Sudden catecholamine surge causing hypertensive emergencies.
- Recurrence or Metastasis: In malignant cases.
Quality of Life and Monitoring
Patients generally experience symptom improvement post-adrenalectomy, especially if hormone-secreting tumors were removed.
- Lifelong endocrine follow-up is necessary, particularly after bilateral surgery.
- Hormone replacement therapy adherence is crucial.
- Patients should be educated about adrenal crisis signs and carry emergency steroids if needed.
- Gradual return to physical activity is encouraged.
- Psychological support may be helpful for patients dealing with chronic conditions or cancer.
1. What is an adrenalectomy?
Adrenalectomy is a surgical procedure to remove one or both adrenal glands, which sit above the kidneys and produce important hormones like adrenaline and cortisol.
2. Why would someone need an adrenalectomy?
It is typically performed to remove adrenal tumors, including benign growths, cancerous tumors, or hormone-producing tumors causing conditions like Cushing’s syndrome or pheochromocytoma.
3. What are the different types of adrenalectomy procedures?
There are mainly two approaches:
- Laparoscopic adrenalectomy: Minimally invasive, using small incisions and a camera.
- Open adrenalectomy: Traditional surgery with a larger incision, usually for larger tumors or complicated cases.
4. How long does the surgery take?
Laparoscopic adrenalectomy generally takes 2 to 3 hours, while open surgery can take longer depending on tumor size and complexity.
5. What is the recovery time after adrenalectomy?
Recovery varies by surgery type: laparoscopic patients may return to normal activities within 2 to 4 weeks, while open surgery patients may require 4 to 6 weeks or longer for full recovery.
6. What are the risks and potential complications?
Risks include bleeding, infection, injury to surrounding organs, hormone imbalances, and blood pressure fluctuations. Careful preoperative evaluation and postoperative care help reduce these risks.
7. Will I need hormone replacement therapy after surgery?
If both adrenal glands are removed, lifelong hormone replacement is necessary. If only one gland is removed, the remaining gland usually compensates, and hormone therapy may not be needed.
8. How is adrenalectomy performed laparoscopically?
The surgeon makes small incisions to insert a camera and surgical tools to carefully detach and remove the adrenal gland with minimal trauma and faster recovery.
9. What symptoms should I watch for after adrenalectomy?
Watch for signs of infection, severe pain, dizziness, fatigue, or symptoms of hormone imbalance such as low blood pressure or unusual weakness, and report these promptly to your doctor.
10. How effective is adrenalectomy in treating adrenal tumors?
Adrenalectomy is often very effective, especially for benign tumors and hormone-secreting tumors, providing symptom relief and reducing risks related to tumor growth or hormone excess.
The other Cosmetic Procedures are:
Few Popular Hospitals for Adrenalectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



