Vagina posterior repair, also known as posterior colporrhaphy, is a specialized surgical procedure aimed at correcting defects in the posterior vaginal wall, most commonly rectocele. This condition arises when the rectovaginal septum—the connective tissue between the rectum and the vagina—weakens or tears, causing the rectum to bulge into the vaginal canal. This bulging can cause a variety of physical and functional symptoms that affect a woman’s quality of life.
Posterior vaginal wall defects are a frequent manifestation of pelvic organ prolapse and are often related to childbirth trauma, aging, chronic pressure, or connective tissue disorders.
Women experiencing symptoms related to rectocele or posterior prolapse often benefit significantly from vaginal posterior repair, which restores anatomy, improves function, and alleviates discomfort.
Modern surgical techniques focus not only on anatomical restoration but also on minimizing complications, preserving sexual function, and promoting long-term pelvic floor health.
Primary Causes
-
Vaginal Childbirth Injury: The most common cause is trauma or overstretching of the pelvic floor muscles and connective tissues during labor and delivery, especially with prolonged or assisted vaginal delivery.
-
Aging and Menopause: Declining estrogen levels lead to atrophic changes and decreased collagen production in pelvic tissues.
-
Chronic Intra-abdominal Pressure: Factors like chronic coughing, obesity, constipation, and heavy lifting can strain and weaken pelvic support.
-
Previous Pelvic or Abdominal Surgeries: Surgical trauma and scarring may compromise support structures.
-
Connective Tissue Disorders: Genetic conditions like Ehlers-Danlos syndrome affect tissue strength.
Risk Factors
-
Multiple vaginal births.
-
Large fetal birth weight.
-
Instrumental delivery (forceps or vacuum).
-
Prolonged second stage of labor.
-
Obesity and sedentary lifestyle.
-
Chronic constipation or straining.
-
Smoking and poor nutritional status.
-
Vaginal Bulge: Sensation or visible protrusion of tissue into the vaginal canal, often worsening with standing or straining.
-
Pelvic Pressure or Heaviness: Discomfort or fullness in the perineal or vaginal area.
-
Difficulty with Defecation: Sensation of incomplete evacuation, constipation, or needing manual support (splinting) to pass stools.
-
Pain During Sexual Intercourse: Due to anatomical distortion or associated nerve irritation.
-
Urinary Symptoms: Occasionally, associated bladder prolapse can cause urinary urgency or retention.
-
Recurrent Infections or Irritation: From trapped vaginal secretions or stool.
Clinical Examination
-
A comprehensive pelvic exam assessing vaginal wall integrity and prolapse degree.
-
Inspection and palpation while patient performs Valsalva maneuver to visualize bulging.
-
Evaluation of anal sphincter tone and perineal body.
Ancillary Tests
-
Defecography: Dynamic imaging during defecation to evaluate rectocele size and rectal emptying.
-
Pelvic MRI or Ultrasound: For soft tissue evaluation and complex cases.
-
Urodynamic Studies: When urinary symptoms coexist.
-
Colonoscopy: If bowel symptoms warrant exclusion of other pathologies.
Conservative Approaches
-
Pelvic Floor Physical Therapy: Strengthening pelvic muscles can improve symptoms.
-
Pessary Use: Mechanical support to reduce prolapse.
-
Dietary Modifications: To prevent constipation and reduce straining.
-
Biofeedback and Behavioral Therapies: To optimize defecatory dynamics.
Surgical Interventions
-
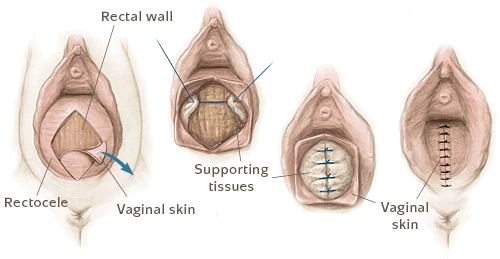
Posterior Colporrhaphy: Suturing and reinforcing the rectovaginal fascia and vaginal wall.
-
Perineorrhaphy: Repair of the perineal body to support the pelvic floor.
-
Use of Mesh: In select cases to provide additional reinforcement, though risks are carefully weighed.
-
Sphincteroplasty: When associated anal sphincter defects are present.
-
Transanal or Transvaginal Approaches: Based on surgeon preference and defect location.
Surgical Technique Overview
-
Usually performed under regional or general anesthesia.
-
Vaginal incision made to access posterior wall and fascia.
-
Redundant tissue excised; underlying support repaired.
-
Careful hemostasis and layered closure to minimize scarring.
-
Drains placed if necessary; postoperative monitoring.
Preventive Measures
-
Maintain healthy weight.
-
Avoid chronic straining with stool softeners and hydration.
-
Pelvic floor exercises especially during and after pregnancy.
-
Smoking cessation.
-
Manage chronic cough or respiratory conditions.
Postoperative Management
-
Pain control and antibiotics as needed.
-
Instructions on hygiene and wound care.
-
Avoid heavy lifting and straining for 6-8 weeks.
-
Gradual return to normal activities.
-
Pelvic floor rehabilitation as indicated.
-
Regular follow-up to monitor for recurrence.
Common Side Effects
-
Swelling, bruising, mild discomfort.
-
Temporary urinary retention.
-
Vaginal discharge and minor bleeding.
Potential Serious Complications
-
Infection requiring antibiotics or drainage.
-
Recurrence of prolapse.
-
Dyspareunia (painful intercourse).
-
Bladder or rectal injury during surgery.
-
Mesh erosion or rejection if mesh used.
-
Anal sphincter dysfunction if involved.
-
Need for revision surgery.
Strategies to Reduce Risks
-
Preoperative optimization.
-
Experienced pelvic reconstructive surgeon.
-
Meticulous surgical technique.
-
Patient adherence to postoperative guidelines.
Recovery Expectations
-
Initial soreness and swelling subside in weeks.
-
Return to non-strenuous activities in 2-4 weeks.
-
Full healing and tissue remodeling take 3-6 months.
-
Improvement in bowel function and pelvic symptoms expected.
Long-Term Care
-
Regular pelvic floor strengthening exercises.
-
Healthy bowel habits.
-
Routine gynecologic and colorectal follow-up.
-
Lifestyle modifications to maintain pelvic health.
Psychological and Social Impact
-
Relief from discomfort and embarrassment.
-
Improved sexual function and intimate relationships.
-
Enhanced quality of life and self-esteem.
1. What is vagina posterior repair?
Vagina posterior repair, also known as posterior colporrhaphy, is a surgical procedure to repair and strengthen the back wall of the vagina, often to correct a rectocele or vaginal laxity.
2. Why is posterior vaginal repair needed?
It is typically recommended for women who experience bulging or pressure in the vaginal area, difficulty with bowel movements, or discomfort caused by a rectocele (prolapse of the rectum into the vagina).
3. What causes the need for posterior repair?
Common causes include childbirth trauma, aging, menopause, chronic constipation, or pelvic floor weakness leading to vaginal wall weakness or prolapse.
4. How is the procedure performed?
The surgeon makes an incision in the vaginal wall to access and tighten the weakened tissues and muscles, restoring normal anatomy and function.
5. What are the benefits of vagina posterior repair?
The procedure improves vaginal support, relieves discomfort, reduces bulging, and helps restore normal bowel function and sexual activity.
6. What is the recovery time after posterior repair?
Most patients recover within 4 to 6 weeks, during which they should avoid heavy lifting, straining, and sexual intercourse to ensure proper healing.
7. Are there risks or complications associated with this surgery?
Risks include infection, bleeding, pain, urinary or bowel dysfunction, and recurrence of prolapse. Choosing an experienced surgeon minimizes these risks.
8. Is posterior vaginal repair painful?
Post-operative discomfort is common but manageable with prescribed pain medication. Sensation usually returns to normal as healing progresses.
9. Will this surgery affect sexual function?
The goal is to improve function and reduce symptoms. Most patients report improved comfort and sexual satisfaction after full recovery.
10. How can I prepare for vagina posterior repair surgery?
Preparation includes a medical evaluation, managing any infections, stopping smoking, avoiding certain medications, and arranging for post-op care and support.
The other Cosmetic Procedures are:
Few Popular Hospitals for Vagina Posterior Repair are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



