Periodontal disease, commonly known as gum disease, represents one of the most prevalent oral health problems globally, affecting millions of individuals across all age groups. It is an inflammatory condition that primarily targets the periodontium—the specialized tissues that surround and support teeth—including the gingiva (gums), periodontal ligament, cementum, and alveolar bone.
If untreated, periodontal disease can progress from mild gingivitis to severe periodontitis, resulting in gum recession, bone loss, tooth mobility, and eventual tooth loss. Periodontic treatment encompasses a spectrum of evidence-based therapies aimed at halting disease progression, restoring periodontal health, and preserving natural dentition.
The complexity of periodontic treatment requires an individualized approach integrating non-surgical and surgical interventions, coupled with patient education and lifestyle modifications. This comprehensive guide explores the etiology, clinical manifestations, diagnostic methodologies, therapeutic options, preventive strategies, complications, and quality of life considerations in managing periodontal disease.
Pathophysiology and Etiology
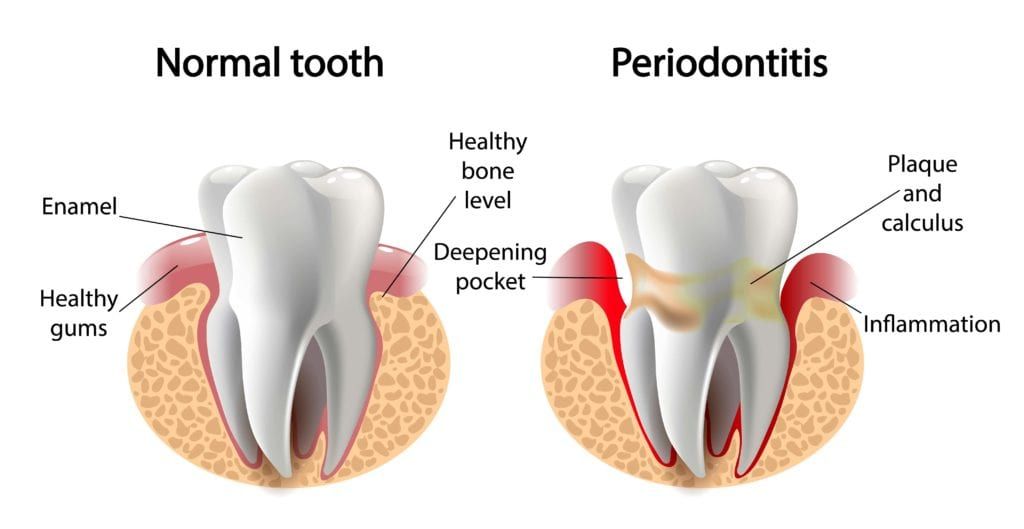
Periodontal disease initiates with the accumulation of microbial dental plaque—a biofilm comprised of pathogenic bacteria—on tooth surfaces. Persistent plaque induces an immune-inflammatory response in the gingival tissues, leading to the destruction of connective tissue and alveolar bone.
Untreated plaque calcifies to form calculus (tartar), which exacerbates bacterial colonization and mechanical irritation. The interplay between microbial virulence factors and host immune response determines disease severity and progression.
Major Causes and Contributors
-
Dental Plaque Accumulation: Primary etiological factor driving inflammation.
-
Subgingival Calculus Deposits: Difficult to remove without professional intervention.
-
Poor Oral Hygiene Practices: Allow unchecked plaque buildup.
-
Smoking: Impairs neutrophil function, decreases gingival blood flow, and exacerbates periodontal destruction.
-
Systemic Conditions: Diabetes mellitus, cardiovascular disease, rheumatoid arthritis, and other immunocompromising conditions increase susceptibility and impair healing.
-
Genetic Predisposition: Polymorphisms in immune-regulatory genes can predispose to aggressive periodontitis.
-
Hormonal Fluctuations: Puberty, pregnancy, and menopause alter gingival tissue responses.
-
Medications: Calcium channel blockers, phenytoin, and cyclosporine cause gingival enlargement.
-
Psychosocial Factors: Chronic stress modulates immune function adversely.
Clinical Presentation
-
Gingival Bleeding: Easily provoked bleeding on brushing, flossing, or spontaneously.
-
Gingival Inflammation: Redness, swelling, tenderness, and changes in texture.
-
Periodontal Pocket Formation: Pathologic deepening of the sulcus exceeding 3 mm measured by periodontal probing.
-
Gingival Recession: Apical migration of the gingival margin exposing root surfaces.
-
Halitosis: Persistent bad breath caused by bacterial endotoxins.
-
Tooth Mobility: Reflecting loss of supporting bone and ligamentous attachment.
-
Suppuration: Presence of pus from periodontal pockets indicating active infection.
-
Pain and Discomfort: May occur in advanced disease or abscess formation.
Clinical Examination
-
Full-mouth periodontal charting including probing depths, bleeding on probing, attachment levels, plaque index, and tooth mobility.
-
Assessment of furcation involvement in molars.
-
Gingival phenotype evaluation (thin vs. thick biotype).
-
Occlusal analysis for trauma from occlusion.
Radiographic Evaluation
-
Periapical and bitewing radiographs to assess alveolar bone loss pattern and severity.
-
Panoramic radiographs for global assessment of jaws and identification of additional pathology.
-
Cone Beam Computed Tomography (CBCT) for three-dimensional imaging in complex cases.
Laboratory Investigations
-
Microbial sampling for pathogen identification in refractory cases.
-
Host-response biomarker analysis (research setting).
Medical and Dental History
-
Review of systemic health, medications, smoking status, and prior dental treatments.
Phase I: Initial/Nonsurgical Therapy
-
Scaling and Root Planing (SRP): Removal of supra- and subgingival plaque and calculus with hand instruments and ultrasonic scalers, followed by meticulous smoothing of root surfaces to remove endotoxins.
-
Adjunctive Antimicrobial Therapy: Topical or systemic antibiotics used selectively in aggressive or refractory cases.
-
Patient Education: Instruction on proper brushing, interdental cleaning, and lifestyle modification.
Phase II: Surgical Therapy
-
Indicated when deep pockets (>5 mm) persist post-SRP or for regenerative procedures.
-
Flap Surgery (Access Surgery): Reflection of gingival tissues to allow direct visualization and cleaning of root surfaces and osseous defects.
-
Osseous Surgery: Reshaping of alveolar bone to eliminate infrabony defects.
-
Guided Tissue Regeneration (GTR): Placement of barrier membranes to promote selective cell repopulation and regeneration of periodontal ligament and bone.
-
Soft Tissue Grafting: Free gingival or connective tissue grafts to augment keratinized tissue and cover root exposures.
-
Bone Grafting: Autografts, allografts, or synthetic materials to rebuild alveolar bone defects.
-
Laser-Assisted Periodontal Therapy: Minimally invasive removal of inflamed tissue and bacterial load with improved healing dynamics.
Phase III: Maintenance Therapy
-
Supportive periodontal therapy every 3-6 months.
-
Reinforcement of oral hygiene and monitoring for disease recurrence.
Preventive Measures
-
Consistent, effective daily oral hygiene practices including twice-daily brushing and interdental cleaning.
-
Smoking cessation programs and lifestyle counseling.
-
Balanced nutrition emphasizing antioxidants and anti-inflammatory foods.
-
Management of systemic diseases with healthcare provider collaboration.
-
Regular professional cleanings and periodontal monitoring.
Patient Engagement and Education
-
Empowering patients with knowledge of periodontal disease etiology and importance of compliance.
-
Motivational interviewing to enhance behavior change.
Possible Complications
-
Postoperative pain, swelling, and transient sensitivity.
-
Gingival recession leading to aesthetic and sensitivity concerns.
-
Incomplete calculus removal causing persistent inflammation.
-
Allergic or adverse reactions to materials used in treatment.
-
Rare infections or delayed healing.
-
Patient non-compliance leading to disease recurrence.
Recovery and Adaptation
-
Initial healing takes 1-2 weeks; complete resolution of inflammation may take several months.
-
Enhanced awareness and control of risk factors improve long-term prognosis.
-
Use of desensitizing agents for exposed root surfaces.
Maintenance and Monitoring
-
Lifelong supportive care is necessary to maintain periodontal stability.
-
Regular recall visits with professional cleaning and examination.
Psychological and Social Impact
-
Improved self-confidence following treatment and restoration of oral health.
-
Addressing anxiety related to dental care through patient support.
1. What is periodontic treatment?
Periodontic treatment refers to the range of dental procedures aimed at preventing, diagnosing, and treating periodontal (gum) disease. It focuses on the health of the gums and supporting structures around the teeth to prevent tooth loss and maintain oral health.
2. What causes periodontal disease?
Periodontal disease is primarily caused by bacterial plaque buildup on teeth and gums. Poor oral hygiene, smoking, genetic factors, certain illnesses like diabetes, and hormonal changes can increase the risk of developing gum disease.
3. What are the signs and symptoms of periodontal disease?
Common signs include red, swollen, or bleeding gums, bad breath, gum recession, loose teeth, and persistent bad taste. In advanced stages, it may cause pain and tooth loss.
4. What types of periodontic treatments are available?
Treatments range from non-surgical procedures like scaling and root planing (deep cleaning) to surgical interventions such as flap surgery, soft tissue grafts, and regenerative procedures to restore lost bone and tissue.
5. How is scaling and root planing performed?
Scaling removes plaque and tartar from tooth surfaces and beneath the gums, while root planing smooths the tooth roots to help gums reattach. This procedure is usually done under local anesthesia over one or more visits.
6. When is surgery needed in periodontic treatment?
Surgery is recommended when deep pockets between gums and teeth don’t respond to non-surgical treatments. Surgical procedures help reduce pocket depth, remove infected tissue, and regenerate damaged bone and gums.
7. Is periodontic treatment painful?
Most treatments are performed under local anesthesia to minimize discomfort. Post-treatment sensitivity and mild soreness are common but manageable with prescribed pain relief and proper care.
8. How long does it take to recover from periodontic treatment?
Recovery time varies depending on the treatment type. Non-surgical treatments typically require a few days to heal, while surgical procedures may take several weeks. Following post-treatment care instructions speeds recovery.
9. Can periodontic treatment reverse gum disease?
Early-stage gum disease (gingivitis) is reversible with proper treatment and oral hygiene. Advanced periodontal disease can be managed and controlled with treatment but may not be fully reversible. The goal is to halt progression and maintain oral health.
10. How can I prevent periodontal disease?
Prevention includes regular dental checkups and cleanings, proper brushing and flossing, quitting smoking, maintaining a healthy diet, and managing systemic conditions like diabetes. Early detection and treatment are key.
The other Dental Procedures are:
Few Popular Hospitals for Tooth Veneers are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



