Laparoscopy-Assisted Hemicolectomy (LAH) is a minimally invasive surgical procedure used to remove part of the colon, typically when a disease or condition is localized in one section of the colon. This procedure is commonly performed to treat conditions such as colon cancer, inflammatory bowel disease (IBD) (like Crohn’s disease or ulcerative colitis), and diverticulitis.
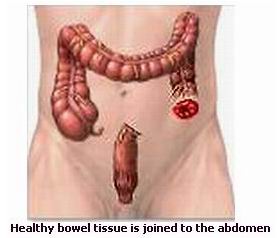
During a laparoscopic-assisted hemicolectomy, the surgeon uses a laparoscope, a long, flexible tube with a camera and light, inserted through small incisions in the abdomen. The laparoscope allows the surgeon to view the colon and the affected area on a monitor. Once the diseased part of the colon is identified, the surgeon removes it, and the remaining sections of the colon are reconnected.
This procedure offers several advantages over traditional open surgery, including reduced pain, smaller incisions, faster recovery, and a lower risk of infection. Laparoscopy-assisted hemicolectomy is a preferred method for many patients due to its minimally invasive nature.
The main reason for performing a laparoscopy-assisted hemicolectomy is the presence of conditions that affect the colon, either due to disease, infection, or structural abnormalities. Here are the primary causes and risk factors associated with this surgery:
Causes of Laparoscopy-Assisted Hemicolectomy
-
Colon Cancer:
-
Colon cancer is one of the leading causes of laparoscopic-assisted hemicolectomy. Tumors located in the colon can obstruct the passage of stool, cause bleeding, and disrupt normal bowel function. Removal of the affected portion of the colon is often necessary to treat localized cancer.
-
-
Diverticulitis:
-
Diverticulitis occurs when pouches (diverticula) in the colon become inflamed or infected. Severe cases that don’t respond to antibiotics may require surgery to remove the affected section of the colon.
-
-
Inflammatory Bowel Disease (IBD):
-
Ulcerative colitis and Crohn’s disease are chronic conditions that cause inflammation in the digestive tract. If these conditions cause significant damage to a portion of the colon, a hemicolectomy may be needed to remove the damaged part.
-
-
Bowel Obstruction:
-
A blockage in the colon, often due to scar tissue or tumors, may necessitate a hemicolectomy to relieve symptoms and prevent further complications.
-
-
Benign Tumors or Polyps:
-
Large or symptomatic polyps or benign tumors in the colon may require removal to prevent progression to cancer or to alleviate symptoms like bleeding or obstruction.
-
Risk Factors for Conditions Leading to Hemicolectomy
Several factors can increase the likelihood of needing laparoscopic-assisted hemicolectomy:
-
Age:
-
The risk of colon cancer and inflammatory bowel disease increases with age, particularly in individuals over 50. Regular screening is important to detect issues early.
-
-
Family History:
-
A family history of colon cancer, polyps, or IBD increases the likelihood of developing these conditions. Genetic conditions like familial adenomatous polyposis (FAP) and Lynch syndrome also increase the risk.
-
-
Poor Diet and Lifestyle:
-
Diets high in red meat and processed foods while low in fiber, combined with a sedentary lifestyle, can increase the risk of colorectal cancer and polyps.
-
-
Chronic Conditions:
-
Chronic inflammatory bowel disease or diverticular disease can cause long-term damage to the colon, necessitating surgical intervention.
-
Patients who require a laparoscopic-assisted hemicolectomy often experience symptoms related to the underlying condition affecting the colon. Common symptoms and signs include:
-
Abdominal Pain or Discomfort:
-
Pain in the lower abdomen, which can vary from mild to severe, often accompanies conditions such as diverticulitis or inflammatory bowel disease.
-
-
Bloating and Fullness:
-
Patients may feel bloating or fullness in the abdomen due to intestinal blockages, gas accumulation, or inflammation in the colon.
-
-
Chronic Diarrhea or Constipation:
-
Conditions like IBD or diverticulitis can cause either chronic diarrhea or severe constipation, leading to discomfort and digestive distress.
-
-
Rectal Bleeding:
-
Blood in the stool or rectal bleeding may indicate the presence of tumors, polyps, or inflammatory conditions affecting the colon.
-
-
Unexplained Weight Loss:
-
Weight loss that is unexplained, especially in the presence of abdominal pain or digestive symptoms, may indicate the progression of a condition like colon cancer.
-
-
Fatigue:
-
Ongoing fatigue may result from anemia caused by chronic blood loss due to conditions like diverticulitis or colon cancer.
-
-
Nausea and Vomiting:
-
Obstructions or complications in the colon may lead to nausea, vomiting, or a feeling of fullness, particularly after eating.
-
A thorough diagnostic evaluation is crucial before determining whether a laparoscopic-assisted hemicolectomy is the appropriate treatment. Here are the steps involved in diagnosing conditions that may require this procedure:
1. Medical History and Physical Examination:
-
The doctor will start by reviewing the patient’s medical history and conducting a physical examination. This may include checking for signs of bloating, abdominal tenderness, or abnormal bowel sounds.
2. Colonoscopy:
-
Colonoscopy is the primary diagnostic tool for identifying issues in the colon. It allows the doctor to visually inspect the entire colon for signs of polyps, tumors, or inflammation and take biopsies if necessary.
3. CT or MRI Imaging:
-
CT scans or MRI can help assess the size and extent of the disease, particularly in cases of colon cancer or diverticulitis, and identify any complications that may require surgery.
4. Blood Tests:
-
Blood tests, including a complete blood count (CBC), can detect signs of anemia, infection, or inflammation, which may indicate the presence of a disease requiring surgery.
5. Barium Enema:
-
A barium enema is sometimes used to get detailed images of the colon and rectum. It is especially helpful in detecting blockages or narrowing of the colon.
Laparoscopy-Assisted Hemicolectomy is the surgical procedure typically used to treat conditions like colon cancer, diverticulitis, or inflammatory bowel disease. The procedure involves several key steps:
1. Laparoscopic Surgery:
-
Laparoscopy-assisted hemicolectomy is a minimally invasive surgery where the surgeon removes part of the colon using small incisions and a camera. The remaining parts of the colon are then reconnected to restore bowel function.
-
This surgery is performed under general anesthesia and typically requires only a few small incisions, reducing recovery time compared to traditional open surgery.
2. Chemotherapy or Radiation Therapy:
-
For patients with colon cancer, chemotherapy or radiation therapy may be recommended before or after surgery to shrink tumors or destroy any remaining cancer cells.
3. Post-Operative Care:
-
After surgery, patients are monitored for complications such as infection, bleeding, or leaks at the anastomosis (connection point between colon sections).
-
Pain management and early mobilization (getting the patient moving post-surgery) are key aspects of post-operative care.
Preventive Measures for Colon and Stomach Health:
-
Diet and Lifestyle:
-
A high-fiber diet, rich in fruits, vegetables, and whole grains, can help reduce the risk of colon cancer and promote healthy bowel movements.
-
Regular exercise and maintaining a healthy weight are essential for reducing the risk of conditions that can lead to surgery.
-
-
Regular Screenings:
-
Routine colorectal cancer screenings (such as colonoscopies) are recommended for individuals over the age of 50 or for those with a family history of colon cancer.
-
Early detection of polyps or cancer can lead to less invasive treatment options and prevent the need for surgery.
-
-
Management of Underlying Conditions:
-
Proper management of inflammatory bowel disease and conditions like diverticulitis through medication and diet can prevent the progression of these diseases and reduce the need for surgery.
-
While laparoscopic-assisted hemicolectomy is generally safe, as with any surgery, complications can occur:
-
Infection:
-
Any surgical procedure carries the risk of infection, including wound infection or abdominal abscesses after surgery.
-
-
Bleeding:
-
There may be some post-operative bleeding, which can usually be controlled. However, excessive bleeding may require further intervention.
-
-
Leakage:
-
There is a risk of leakage at the site where the colon was reconnected, which can lead to severe infection and may require additional surgery.
-
-
Bowel Obstruction:
-
Scar tissue or adhesions may form in the abdominal cavity after surgery, leading to a potential bowel obstruction.
-
After laparoscopic-assisted hemicolectomy, patients will need to adjust to new lifestyle habits:
-
Post-Surgery Diet:
-
Following surgery, a soft diet is often recommended initially, progressing to a regular diet as the digestive system heals. It is important to avoid heavy meals and increase fiber intake gradually.
-
-
Colorectal Surveillance:
-
For patients with colon cancer or a family history of colorectal cancer, regular follow-up colonoscopies are recommended to monitor for new polyps or cancer.
-
-
Physical Activity:
-
Patients are encouraged to engage in light exercise and increase activity gradually to improve overall health and prevent complications such as blood clots.
-
-
Emotional Support:
-
Coping with the emotional and psychological impact of surgery is essential. Support from family, counselors, or support groups can help patients adjust to life after surgery.
-
1. What is laparoscopy-assisted hemicolectomy?
Laparoscopy-assisted hemicolectomy is a minimally invasive surgical procedure to remove a portion of the colon (usually the right or left side) for conditions like colon cancer, diverticulitis, or inflammatory bowel disease. The surgery is performed using a laparoscope, which is a small camera inserted through tiny incisions in the abdomen, allowing the surgeon to guide the procedure with high precision.
2. Why is laparoscopy-assisted hemicolectomy performed?
This surgery is typically performed to treat diseases or conditions that affect the colon, including:
-
Colon cancer: To remove tumors or cancerous sections of the colon.
-
Diverticulitis: In cases where diverticula in the colon become inflamed or infected.
-
Inflammatory bowel disease (IBD): Such as Crohn’s disease or ulcerative colitis, when parts of the colon become severely affected.
-
Benign polyps: To remove large or problematic polyps that may lead to cancer.
3. How is laparoscopy-assisted hemicolectomy performed?
The procedure is done under general anesthesia. A small incision is made in the abdomen, and a laparoscope (a tube with a camera and light) is inserted to visualize the colon. Through additional small incisions, the surgeon uses special instruments to remove the diseased portion of the colon and then reattach the healthy parts of the colon. The operation is guided by the laparoscope’s camera, which provides real-time imaging.
4. Is laparoscopy-assisted hemicolectomy painful?
The surgery itself is painless as the patient is under general anesthesia. After the procedure, patients may experience mild to moderate abdominal pain, bloating, and discomfort due to the small incisions and air used during the surgery. Pain is typically managed with medications, and discomfort usually subsides in a few days to weeks.
5. How long does the surgery take?
Laparoscopy-assisted hemicolectomy usually takes about 2 to 3 hours, depending on the complexity of the surgery and the patient's overall health.
6. What is the recovery time after laparoscopy-assisted hemicolectomy?
Recovery time varies, but most patients can leave the hospital in 2 to 4 days. Full recovery may take 4 to 6 weeks. Most people can return to normal activities, including work, after about 2 weeks, but they may need to avoid strenuous activities and lifting for a longer period.
7. Are there any risks or complications associated with laparoscopy-assisted hemicolectomy?
As with any surgery, risks include infection, bleeding, injury to surrounding organs, blood clots, and bowel obstruction. However, laparoscopy-assisted surgery has fewer complications compared to traditional open surgery due to smaller incisions and less trauma to surrounding tissue.
8. How should I prepare for laparoscopy-assisted hemicolectomy?
Preparation includes:
-
A thorough evaluation by your surgeon, including blood tests, imaging studies (like CT scans or colonoscopy), and possibly bowel preparation with a special diet or laxatives.
-
You may need to stop taking certain medications (like blood thinners) before the surgery.
-
You will be asked to fast for several hours before the procedure.
9. What should I expect after laparoscopy-assisted hemicolectomy?
After the procedure, you will be monitored in the recovery room, and your diet will be gradually reintroduced. You may experience some pain, bloating, and fatigue in the first few days. The recovery period will involve rest, managing the surgical site, and following a controlled diet initially. Regular follow-up visits are essential to ensure proper healing.
10. Will I need a colostomy after laparoscopy-assisted hemicolectomy?
In most cases, a colostomy is not necessary, as the surgeon typically reattaches the remaining sections of the colon. However, in cases where the colon cannot be safely reconnected, a temporary or permanent colostomy may be required. Your surgeon will discuss this with you prior to the surgery.
The other Gastro procedures are:
Few Major Hospitals for Laparoscopy Assisted Hemicolectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Laparoscopy Assisted Hemicolectomy | Doctors For Laparoscopy Assisted Hemicolectomy | Surgery Laparoscopy Assisted Hemicolectomy | Cost Laparoscopy Assisted Hemicolectomy | Treatment Laparoscopy Assisted Hemicolectomy | Destinations Laparoscopy Assisted Hemicolectomy | Risks Laparoscopy Assisted Hemicolectomy | Laparoscopy Assisted Hemicolectomy In India | Laparoscopy Assisted Hemicolectomy Recovery | Laparoscopy Assisted Hemicolectomy Information | Laparoscopy Assisted Hemicolectomy Thailand | Laparoscopy Assisted Hemicolectomy In Malaysia | Laparoscopy Assisted Hemicolectomy Abroad | Laparoscopy Assisted Hemicolectomy Donors | Laparoscopy Assisted Hemicolectomy Overseas | Laparoscopy Assisted Hemicolectomy Low Cost | Laparoscopy Assisted Hemicolectomy In Singapore | Laparoscopy Assisted Hemicolectomy In Argentina | Laparoscopy Assisted Hemicolectomy | Colectomy | Stoma | Colon | Anastomosis | Left Radical Hemicolectomy | Splenic Flexure | Transverse Colon | Right Radical Hemicolectomy | Sigmoid Resection | Rectosigmoid Resection | Abdominoperineal Resection | APR
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


