Laparoscopic cardiomyotomy is a procedure used to treat achalasia, a condition that affects the esophagus. Achalasia is characterized by the failure of the lower esophageal sphincter (LES) to relax properly, which prevents food from passing into the stomach. This condition often results in chest pain, difficulty swallowing (dysphagia), regurgitation of food, and other digestive issues.
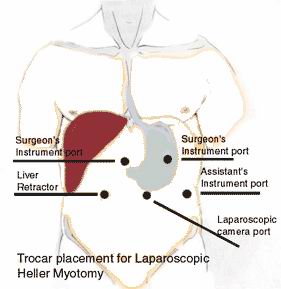
In laparoscopic cardiomyotomy, the surgeon cuts through the muscle of the LES to alleviate the obstruction and restore normal swallowing. The procedure is performed using minimally invasive techniques, meaning smaller incisions are made, and a camera (laparoscope) is used to guide the surgeon. This results in less pain, fewer complications, and a faster recovery compared to traditional open surgery.
How Laparoscopic Cardiomyotomy Works
-
Preparation: Before the surgery, the patient is given general anesthesia to ensure they are unconscious and pain-free.
-
Small Incisions: The surgeon makes several small incisions in the abdomen. Through these incisions, the laparoscope and surgical instruments are inserted.
-
Insertion of Laparoscope: The laparoscope, which is a thin tube with a camera and light, is inserted through one of the incisions. The camera provides a clear view of the esophagus on a monitor, allowing the surgeon to operate with precision.
-
Cardiomyotomy: The surgeon carefully cuts the muscle fibers of the LES to allow the esophagus to relax and food to pass more easily into the stomach.
-
Post-Surgical Care: After the procedure, the incisions are closed with sutures, and the patient is monitored during recovery. Most patients experience a significant improvement in symptoms after surgery.
Advantages of Laparoscopic Cardiomyotomy
-
Minimally Invasive: Smaller incisions reduce the risk of infection and scarring.
-
Quicker Recovery: Patients typically recover faster compared to open surgery and can return to daily activities sooner.
-
Less Pain: The procedure is associated with less postoperative pain.
-
Shorter Hospital Stay: Most patients can go home within 1-2 days after surgery.
Laparoscopic cardiomyotomy is used to treat achalasia, a condition that results from dysfunction in the lower esophageal sphincter. Understanding the causes and risk factors that contribute to achalasia is important for recognizing the condition and seeking timely treatment.
Causes of Achalasia
The exact cause of achalasia is still not fully understood, but several factors contribute to its development:
-
Immune System Dysfunction:
-
One of the most widely accepted theories is that achalasia is caused by an autoimmune response, in which the body’s immune system attacks the nerves in the esophagus. This immune attack damages the nerve cells responsible for controlling the LES and peristalsis (muscle contractions of the esophagus), leading to its dysfunction.
-
-
Neurological Defects:
-
Achalasia is associated with abnormalities in the nervous system of the esophagus. Specifically, the vagus nerve, which controls the relaxation of the LES, is either damaged or fails to function properly in individuals with achalasia.
-
-
Chagas Disease:
-
In parts of the world where Chagas disease (caused by the Trypanosoma cruzi parasite) is endemic, achalasia can develop as a complication. The parasite can damage the nervous system, leading to esophageal motility issues and contributing to the development of achalasia.
-
-
Genetics:
-
There may be a genetic component to achalasia. Although the disease is not directly inherited, a family history of achalasia may increase the likelihood of developing the condition. Several studies have found a slightly higher prevalence of achalasia among people with a family history of the disorder.
-
-
Infections:
-
While infections are not a direct cause, certain viral or bacterial infections can trigger autoimmune responses in genetically susceptible individuals, leading to achalasia.
-
Risk Factors for Achalasia
-
Age:
-
Achalasia can develop at any age but is most commonly diagnosed in adults between 25 and 60 years of age. It is a condition that affects both men and women equally.
-
-
Family History:
-
A family history of achalasia or related neurological disorders may increase the risk of developing the condition. This suggests that there may be an inherited susceptibility to the disorder.
-
-
Autoimmune Diseases:
-
Individuals with autoimmune diseases, such as rheumatoid arthritis or scleroderma, may be at a higher risk for developing achalasia due to immune system dysfunction.
-
-
Environmental Factors:
-
While not well understood, certain environmental factors or infections could potentially trigger achalasia in genetically predisposed individuals.
-
The symptoms of achalasia are related to the dysfunction of the LES and the inability of the esophagus to effectively move food into the stomach. The symptoms usually develop gradually and can worsen over time if left untreated. Common symptoms include:
-
Difficulty Swallowing (Dysphagia):
-
Difficulty swallowing, particularly with solid foods, is the hallmark symptom of achalasia. As the condition progresses, patients may experience difficulty swallowing liquids as well. This is due to the failure of the LES to relax properly, which prevents food from passing into the stomach.
-
-
Regurgitation of Food:
-
Food and liquid that fail to pass into the stomach may remain in the esophagus and be regurgitated. This can occur hours after eating and may happen while sleeping. Regurgitation is a classic symptom of achalasia.
-
-
Chest Pain:
-
Some individuals with achalasia experience sharp or dull chest pain that may mimic the pain associated with a heart attack. This pain is typically caused by food becoming stuck in the esophagus or by the stretching of the esophagus due to swallowed food.
-
-
Heartburn or Acid Reflux:
-
Even though the LES does not relax properly, some individuals may still experience heartburn-like symptoms due to food or liquid staying in the esophagus for extended periods, causing discomfort.
-
-
Weight Loss:
-
Difficulty swallowing and the inability to eat large amounts of food can lead to weight loss in individuals with achalasia. Poor nutrition and a reduced intake of food can result in significant weight loss over time.
-
-
Coughing or Choking:
-
Some patients may experience coughing or choking episodes, particularly when eating, as food or liquid can get stuck in the esophagus or may be inhaled into the windpipe.
-
-
Feeling of Fullness:
-
The sensation of a lump or food getting stuck in the chest is common in people with achalasia, especially after eating.
-
When to Seek Medical Attention
If you experience any of the symptoms of achalasia, such as difficulty swallowing, chest pain, regurgitation, or unexplained weight loss, it is important to consult a healthcare provider. Early diagnosis and treatment can significantly improve outcomes and quality of life.
Diagnosing achalasia and determining whether laparoscopic cardiomyotomy is the best treatment involves several tests and evaluations. The following diagnostic procedures are commonly used to confirm the diagnosis of achalasia:
-
Esophageal Manometry:
-
This is the most definitive test for diagnosing achalasia. Esophageal manometry measures the pressure and muscle contractions in the esophagus. In patients with achalasia, the test will reveal a failure of the LES to relax and reduced peristalsis (muscle contractions) in the esophagus.
-
-
Barium Swallow X-ray:
-
A barium swallow involves drinking a barium-based liquid that shows up on X-rays. This test can reveal the characteristic "bird’s beak" appearance of the esophagus, which is indicative of achalasia. This occurs due to the narrowing of the LES and the esophagus being dilated above it.
-
-
Endoscopy:
-
An upper endoscopy involves using a flexible tube with a camera to examine the inside of the esophagus. The test can help rule out other conditions, such as cancer or strictures, and confirm the presence of achalasia.
-
-
CT or MRI:
-
In rare cases, a CT scan or MRI may be used to assess the structure of the esophagus and surrounding organs.
-
-
High-Resolution Manometry:
-
This advanced version of manometry provides detailed images and measurements of esophageal pressure and function, offering a clearer diagnosis of achalasia.
-
The primary treatment for achalasia is the relaxation of the LES to allow food to pass into the stomach more easily. Laparoscopic cardiomyotomy is considered the most effective and permanent solution for achalasia. However, several other treatment options may be available depending on the severity of the condition.
Laparoscopic Cardiomyotomy
-
This is the most common and effective treatment for achalasia. The procedure involves cutting the muscle fibers of the LES to allow food to pass freely into the stomach. After the procedure, patients usually experience significant relief from their symptoms.
Alternative Treatments
-
Pneumatic Dilation:
-
A balloon dilation is inserted into the LES and inflated to stretch the muscles. This method can provide temporary relief, but it does not have the long-term effectiveness of cardiomyotomy.
-
-
Botulinum Toxin (Botox) Injection:
-
Botox injections can temporarily paralyze the LES muscles, causing relaxation. This is most effective in individuals with mild achalasia, though the effects may wear off after several months.
-
-
Medications:
-
Calcium channel blockers or nitrates may be prescribed to relax the LES, but these are generally less effective and provide only temporary relief.
-
-
Esophagectomy:
-
In rare and severe cases where other treatments have failed, a total esophagectomy (removal of part or all of the esophagus) may be considered, though this is a more invasive and risky option.
-
Prevention of Achalasia
Since the exact cause of achalasia is not fully understood, there is no known prevention. However, early diagnosis and treatment can prevent complications and improve quality of life.
Post-Surgery Management
-
Dietary Changes:
-
After laparoscopic cardiomyotomy, patients are advised to eat soft foods and liquids initially to avoid discomfort or injury to
-
the esophagus.
-
Lifestyle Modifications:
-
Small, frequent meals and chewing food thoroughly can help ease the digestive process.
-
-
Regular Follow-up Appointments:
-
After surgery, it is important for patients to attend regular follow-up visits to monitor recovery, assess symptom resolution, and check for potential complications.
-
While laparoscopic cardiomyotomy is generally safe, there are some potential risks and complications, including:
-
Esophageal Perforation:
-
A rare but serious complication where a hole develops in the esophagus during the procedure, which can lead to infection and leakage of food contents.
-
-
Acid Reflux:
-
Some patients may develop acid reflux after surgery, as the LES may no longer function to prevent stomach acid from flowing back into the esophagus.
-
-
Infection:
-
As with any surgery, there is a risk of infection at the incision sites or in the abdominal cavity.
-
-
Recurrence of Symptoms:
-
In some cases, the symptoms of achalasia may return after surgery, requiring additional treatments.
-
After undergoing laparoscopic cardiomyotomy, most patients experience significant improvement in their symptoms, and many are able to resume normal activities. However, there are a few things to consider for ongoing management:
-
Dietary Adjustments:
-
Patients are encouraged to follow a soft-food diet initially, and then gradually reintroduce solid foods as they heal. Eating smaller, more frequent meals can also reduce the chances of discomfort.
-
-
Ongoing Care:
-
Regular check-ups with a healthcare provider are essential to monitor for any complications, such as acid reflux or recurrence of symptoms.
-
-
Mental Health:
-
As with any chronic condition, dealing with achalasia can have emotional and psychological impacts. Support groups, therapy, or counseling can help patients cope with the changes in lifestyle post-surgery.
-
-
Quality of Life:
-
Most patients experience a significant improvement in swallowing, digestion, and quality of life after laparoscopic cardiomyotomy.
-
1. What is laparoscopic cardiomyotomy?
Laparoscopic cardiomyotomy is a minimally invasive surgical procedure used to treat achalasia, a condition in which the lower
esophageal sphincter (LES) fails to relax properly, causing difficulty swallowing. The
procedure involves cutting the muscle at the lower end of the esophagus (cardiac sphincter)
to allow food and liquids to pass more easily into the stomach. It is performed using small
incisions and a laparoscope, which is a thin, flexible tube with a camera.
2. Why is laparoscopic cardiomyotomy performed?
Laparoscopic cardiomyotomy is primarily performed to treat achalasia, which causes symptoms like difficulty swallowing,
regurgitation of food, chest pain, and weight loss. The condition occurs when the nerves
controlling the esophageal muscles become damaged, leading to the inability of the esophagus
to properly propel food into the stomach. This procedure helps improve esophageal function
and provides relief from symptoms.
3. How is laparoscopic cardiomyotomy performed?
The surgery is done under general
anesthesia. A small incision is made in the abdomen to insert a laparoscope (a long tube with a camera), and
other small incisions are made for the surgical instruments. The surgeon then carefully cuts
the muscle fibers of the lower esophageal sphincter (LES) to allow for better passage of
food and liquids into the stomach. In some cases, the surgeon may also perform a fundoplication (wrapping the top of the
stomach around the lower esophagus) to prevent acid reflux after surgery.
4. Is laparoscopic cardiomyotomy painful?
The procedure itself is performed under general anesthesia, so there is no pain during
surgery. Post-operatively, patients may experience some discomfort in the chest or abdomen
due to the small incisions and the manipulation of tissues during surgery. This discomfort
is usually well-controlled with pain medication and generally resolves within a few days to
weeks.
5. How long does the surgery take?
Laparoscopic cardiomyotomy typically takes between 1 to 2 hours to complete, depending on the complexity of the
case and the patient’s anatomy. The surgery is minimally invasive, which generally allows
for a quicker procedure compared to traditional open surgery.
6. What is the recovery time after laparoscopic cardiomyotomy?
Recovery time after laparoscopic cardiomyotomy is generally shorter than traditional open surgery. Most patients are able
to go home the day after surgery or within 1 to 2 days. Full recovery can take 2 to 4 weeks, during which time patients may
experience mild discomfort and should avoid strenuous activities. A follow-up visit will be
scheduled to monitor progress and healing.
7. Are there any risks or complications associated with laparoscopic cardiomyotomy?
As with any surgery, there are some risks associated with laparoscopic cardiomyotomy, though
they are rare. Possible risks include:
-
Infection at the incision sites.
-
Bleeding.
-
Esophageal perforation (tear in the esophagus).
-
Acid reflux (though this can be mitigated with fundoplication).
-
Difficulty swallowing or narrowing of the esophagus (stricture).
However, when performed by an experienced surgeon, the risks are minimized.
8. How should I prepare for laparoscopic cardiomyotomy?
Preparation for laparoscopic cardiomyotomy typically involves:
-
Pre-operative assessments, including blood tests and imaging (e.g., barium swallow, esophageal manometry).
-
Fasting for 6 to 8 hours before surgery to reduce the risk of complications during anesthesia.
-
Stopping certain medications (such as blood thinners) if instructed by your doctor.
-
Arranging for post-surgery transportation and help at home as you may need assistance for a few days.
9. Will laparoscopic cardiomyotomy cure achalasia?
Laparoscopic cardiomyotomy is highly
effective in treating achalasia. Most patients experience significant
improvement in symptoms, such as easier swallowing and reduced chest pain. However, the
procedure may not completely cure the condition, and a small number of patients may
experience a recurrence of symptoms over time. In some cases, additional treatments like
balloon dilation or repeated surgery may be necessary.
10. Is laparoscopic cardiomyotomy covered by insurance?
Yes, laparoscopic cardiomyotomy is typically covered by most insurance plans when it is
deemed medically necessary. Achalasia is a recognized medical condition, and the surgery is
commonly approved as part of the treatment. It is important to verify your insurance
coverage and understand any out-of-pocket costs before undergoing the procedure.
The other Gastro procedures are:
Few Major Hospitals for Laparoscopic Heller Myotomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Laparoscopic Heller Myotomy | Doctors For Laparoscopic Heller Myotomy | Surgery Laparoscopic Heller Myotomy | Cost Laparoscopic Heller Myotomy | Treatment Laparoscopic Heller Myotomy | Destinations Laparoscopic Heller Myotomy | Risks Laparoscopic Heller Myotomy | Laparoscopic Heller Myotomy In India | Laparoscopic Heller Myotomy Recovery | Laparoscopic Heller Myotomy Information | Laparoscopic Heller Myotomy Thailand | Laparoscopic Heller Myotomy In Malaysia | Laparoscopic Heller Myotomy Abroad | Laparoscopic Heller Myotomy Donors | Laparoscopic Heller Myotomy Overseas | Laparoscopic Heller Myotomy Low Cost | Laparoscopic Heller Myotomy In Singapore | Laparoscopic Heller Myotomy In Argentina | Laparoscopic Heller Myotomy | Oesophageal Achalasia | Achalasia | Dysphagia | Thoracotomy | Myentric Plexus | Lymphocytes | Barret’s Esophagus
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


