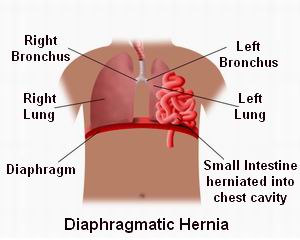
A diaphragmatic hernia is a defect or tear in the diaphragm, allowing the organs of the abdomen to move into the chest cavity. This can lead to various complications, including difficulty breathing, digestive issues, and in severe cases, life-threatening conditions if left untreated. The diaphragm is a critical muscle that aids in breathing and helps to keep the abdominal organs in place.
Laparoscopic diaphragmatic hernia repair is a minimally invasive surgery used to treat this condition. Laparoscopy involves making small incisions in the abdomen through which the surgeon can access the diaphragm, repair the tear, and return the abdominal organs to their proper position, all with the aid of a laparoscope (a small camera).
Why Choose Laparoscopic Surgery?
Laparoscopic repair is preferred over traditional open surgery for several key reasons:
-
Smaller Incisions: Fewer and smaller incisions reduce the risk of infection, minimize scarring, and lead to faster healing.
-
Less Pain: The procedure generally involves less trauma to surrounding tissue, meaning patients experience less pain after surgery.
-
Faster Recovery: Most patients can return to normal activities in a few weeks compared to a longer recovery period with open surgery.
-
Lower Risk of Infection: Due to the reduced exposure of internal organs during surgery, there is a reduced risk of infection.
Laparoscopic diaphragmatic hernia repair is widely regarded as the best treatment option, especially in patients who do not have severe or complicated hernias.
Diaphragmatic hernias can occur due to a variety of causes, including congenital defects, traumatic injuries, or post-surgical complications. Understanding these causes and the associated risk factors can help in early detection and treatment.
Causes of Diaphragmatic Hernia
-
Congenital Diaphragmatic Hernia (CDH):
-
A congenital diaphragmatic hernia occurs when there is a defect in the diaphragm present at birth. The condition allows the abdominal organs to move into the chest cavity during fetal development. CDH is typically diagnosed in infants and is more common in premature babies. In many cases, this defect is discovered soon after birth or during early infancy when respiratory issues arise.
-
-
Traumatic Diaphragmatic Hernia:
-
Traumatic diaphragmatic hernias are caused by blunt or penetrating trauma to the chest or abdomen, such as from motor vehicle accidents, falls, or stab wounds. The trauma can create a tear or rupture in the diaphragm, allowing the abdominal organs to herniate into the chest.
-
-
Post-Surgical Diaphragmatic Hernia:
-
In some cases, a diaphragmatic hernia can develop after abdominal or thoracic surgery. The hernia may result from weaknesses in the diaphragm following surgical incisions, leading to the displacement of abdominal organs.
-
-
Increased Abdominal Pressure:
-
Conditions that increase intra-abdominal pressure, such as obesity, pregnancy, and chronic coughing (common in chronic obstructive pulmonary disease, or COPD), can contribute to the development of diaphragmatic hernias. Over time, this excess pressure can cause the diaphragm to tear.
-
-
Age and Gender:
-
Older individuals may develop diaphragmatic hernias due to the natural weakening of the diaphragm over time. Men are generally more affected by traumatic diaphragmatic hernias than women.
-
Risk Factors for Diaphragmatic Hernia
-
Trauma History:
-
Any prior injury to the chest or abdomen, such as a car accident or fall, significantly increases the risk of a diaphragmatic hernia due to the potential for physical damage to the diaphragm.
-
-
Previous Surgery:
-
Individuals who have had previous abdominal or thoracic surgeries may be at a higher risk due to weakened diaphragmatic tissue or surgical complications.
-
-
Increased Abdominal Pressure:
-
Conditions such as chronic constipation, obesity, and pregnancy can increase intra-abdominal pressure, contributing to the risk of a diaphragmatic hernia. Chronic coughing or heavy lifting may also be risk factors.
-
-
Genetic Factors:
-
Some forms of congenital diaphragmatic hernia may be inherited, with a family history increasing the likelihood of the condition.
-
The symptoms of a diaphragmatic hernia depend on the size of the hernia, the organs involved, and whether the hernia is congenital or acquired. The symptoms may worsen over time if not treated.
Common Symptoms of Diaphragmatic Hernia
-
Chest Pain:
-
Sharp or dull chest pain is a common symptom, especially if the hernia causes pressure on the lungs or other organs in the chest. The pain may worsen with deep breathing or physical exertion.
-
-
Shortness of Breath (Dyspnea):
-
As the hernia causes organs like the stomach or intestines to shift into the chest cavity, it can compress the lungs, leading to difficulty breathing, particularly during physical activity or exertion.
-
-
Abdominal Distension:
-
Bloating or distension in the abdomen may occur, particularly in cases of large hernias. This is caused by the organs displaced into the chest, affecting the digestive process.
-
-
Gastroesophageal Reflux Disease (GERD):
-
Acid reflux or heartburn is a common symptom of diaphragmatic hernia. The hernia can allow the stomach contents to move upward into the esophagus, leading to regurgitation, heartburn, and other symptoms of GERD.
-
-
Nausea and Vomiting:
-
Difficulty swallowing or obstruction caused by the hernia may lead to nausea or vomiting, especially if food or liquid gets stuck in the esophagus.
-
-
Coughing and Wheezing:
-
A persistent cough or wheezing, especially after meals, can occur due to the esophagus being compressed or irritated by the herniated organs.
-
-
Failure to Thrive in Infants:
-
In infants with congenital diaphragmatic hernia, failure to thrive, difficulty feeding, and poor weight gain are common signs.
-
When to Seek Medical Attention
If you experience persistent chest pain, shortness of breath, difficulty swallowing, or nausea and vomiting, seek immediate medical attention. A diaphragmatic hernia can cause severe complications such as strangulation of organs or difficulty breathing, which requires urgent treatment.
Diagnosing a diaphragmatic hernia typically involves a combination of physical examination, imaging tests, and a thorough medical history review. The following diagnostic methods are commonly used:
-
Physical Examination:
-
During a physical exam, the doctor will assess the chest and abdomen for signs of hernia, such as abnormal bowel sounds in the chest or abdominal tenderness.
-
-
Chest X-ray:
-
A chest X-ray is one of the first diagnostic tools used. It can reveal the presence of abdominal organs such as the stomach or intestines in the chest cavity, a key sign of a diaphragmatic hernia.
-
-
CT Scan:
-
A CT scan provides detailed images of the diaphragm and surrounding organs. This is particularly useful for diagnosing the size and complexity of the hernia and determining the best surgical approach.
-
-
Abdominal Ultrasound:
-
Ultrasound can be used to visualize the abdominal organs and identify any abnormalities in the diaphragm or nearby structures.
-
-
Endoscopy:
-
Endoscopy allows the doctor to examine the esophagus and stomach directly, helping to rule out other conditions, such as ulcers or tumors, that could cause similar symptoms.
-
-
MRI:
-
In some cases, MRI may be used to assess the diaphragm and surrounding tissues, particularly if more detailed soft tissue images are required.
-
The primary treatment for a diaphragmatic hernia is surgical intervention. Laparoscopic repair is the preferred method, offering several advantages over traditional open surgery.
Laparoscopic Diaphragmatic Hernia Repair
-
Procedure Overview:
-
Laparoscopic repair involves making small incisions in the abdomen, through which a camera (laparoscope) and surgical instruments are inserted. The surgeon will reposition the herniated organs and close the hole in the diaphragm using sutures or mesh.
-
-
Benefits of Laparoscopic Surgery:
-
Smaller incisions, reduced pain, faster recovery, and fewer complications compared to traditional open surgery.
-
Alternative Treatments
-
Open Surgery:
-
In some cases, especially with large or complex hernias, an open surgical approach may be necessary. This requires a larger incision and may result in a longer recovery time.
-
-
Pneumatic Dilation:
-
For small hernias, a balloon dilation technique may be used to stretch the opening in the diaphragm and reposition the abdominal organs. However, this is less effective for large hernias.
-
Prevention of Diaphragmatic Hernia
-
Congenital hernias cannot be prevented. However, careful prenatal care and screening can help detect diaphragmatic hernias early.
-
Trauma-induced hernias can be minimized by wearing seat belts while driving, taking safety precautions during physical activities, and avoiding abdominal injuries.
Postoperative Management
-
Post-Surgery Care:
-
After laparoscopic repair, patients are typically monitored for any signs of infection or complications. Pain management is important, and most patients will be prescribed pain relievers for the first few days.
-
-
Dietary Changes:
-
Soft foods and liquids may be recommended initially to avoid stressing the repaired diaphragm. Gradual reintroduction of solid foods can occur as healing progresses.
-
-
Regular Follow-up:
-
After surgery, regular follow-up appointments are essential to ensure the patient’s recovery is progressing and that there are no complications, such as recurrence or gastrointestinal issues.
-
While laparoscopic repair is generally safe, there are some risks associated with the surgery:
-
Infection:
-
Infection at the surgical site or within the abdomen is a risk, especially if the hernia was large or complicated.
-
-
Recurrence of the Hernia:
-
In some cases, the hernia may recur if the diaphragm is not adequately repaired or if there is further damage to the diaphragm after surgery.
-
-
Breathing Complications:
-
Some patients may experience shortness of breath or difficulty breathing following surgery, particularly if the diaphragm was significantly weakened or damaged.
-
-
Organ Injury:
-
Although rare, there is a small risk of injury to the organs during surgery, particularly if the herniated organs need to be repositioned or manipulated during repair.
-
After undergoing laparoscopic diaphragmatic hernia repair, patients can typically expect a significant improvement in their symptoms and quality of life. However, ongoing management is important:
-
Dietary Adjustments:
-
Following surgery, a soft-food diet and gradual reintroduction of solid foods are typically recommended. Patients should avoid overeating and large meals to prevent strain on the diaphragm.
-
-
Light Exercise:
-
Light exercise, such as walking, is encouraged post-surgery. Strenuous activities, particularly heavy lifting, should be avoided for a few weeks to allow the diaphragm to heal properly.
-
-
Follow-up Care:
-
Regular visits to the doctor are essential to monitor recovery. During these visits, any concerns or complications can be addressed early.
-
-
Lifestyle Modifications:
-
Maintaining a healthy weight, avoiding smoking, and controlling chronic conditions (e.g., COPD or asthma) can help reduce the risk of recurrence or complications.
-
1. What is a diaphragmatic hernia?
A diaphragmatic hernia is a condition
where
an organ, typically the stomach or intestines, protrudes through an abnormal opening in
the
diaphragm. The diaphragm is the muscle that separates the chest from the abdomen, and a
hernia can occur due to congenital defects or trauma. This hernia can cause symptoms
such as
abdominal pain, breathing difficulty, and digestive problems.
2. What is laparoscopic repair of a diaphragmatic hernia?
Laparoscopic repair of a diaphragmatic hernia is a minimally invasive surgical
procedure
where small incisions are made in the abdomen. A laparoscope (a thin tube with a camera) and small
surgical
tools are used to repair the hernia by closing the opening in the diaphragm and
repositioning any displaced organs back into the abdominal cavity.
3. Why is laparoscopic repair of diaphragmatic hernia preferred?
Laparoscopic surgery offers several advantages over traditional open surgery,
including:
-
Smaller incisions, leading to less pain, faster recovery, and smaller scars.
-
Shorter hospital stay due to the minimally invasive approach.
-
Reduced risk of infection and faster healing.
-
Quicker return to daily activities as compared to open surgery.
4. How is laparoscopic repair of a diaphragmatic hernia performed?
During the laparoscopic procedure, the surgeon makes small incisions in the
abdomen. The
laparoscope is inserted through one incision to visualize the hernia, and
surgical tools are
used through the other incisions to close the hole in the diaphragm. If
necessary, the
displaced organs (such as the stomach or intestines) are gently pushed back
into the
abdomen. In some cases, the diaphragm may be reinforced with mesh to prevent
recurrence of
the hernia.
5. Is laparoscopic repair of diaphragmatic hernia painful?
The surgery is performed under general
anesthesia, so there is no pain during the procedure.
Afterward, patients may
experience some mild
discomfort in the
abdomen or shoulder area due to the carbon dioxide gas used to inflate
the abdomen. This
discomfort typically resolves within a few days and can be managed with
prescribed pain
medications.
6. How long does the surgery take?
The laparoscopic repair of a diaphragmatic hernia typically takes
between 1 to 2
hours, depending on the complexity of
the hernia and the surgeon’s experience. The surgery is less
time-consuming compared to
traditional open surgery due to the minimally invasive approach.
7. What is the recovery time after laparoscopic diaphragmatic hernia repair?
Recovery time is generally shorter than
with open surgery. Most patients can go home 1 to
2 days after the surgery. While patients may
experience some mild discomfort,
they can typically return to normal activities within 1 to 2 weeks.
Avoiding heavy lifting and strenuous activities
for about 4 to 6
weeks is recommended to
ensure proper healing.
8. Are there any risks or complications associated with laparoscopic diaphragmatic hernia repair?
While the risks of laparoscopic surgery are generally low,
potential complications can
include:
-
Infection at the incision sites.
-
Bleeding.
-
Damage to nearby organs, such as the lungs or intestines.
-
Recurrence of the hernia, though this is less common with laparoscopic repair.
However, the risks are minimized when the surgery is performed by an experienced surgeon.
9. How should I prepare for laparoscopic repair of diaphragmatic hernia?
Preparation for surgery typically involves:
-
Preoperative assessments, including blood tests and imaging (such as a CT scan or X-ray) to assess the size and location of the hernia.
-
Fasting for 6 to 8 hours before the surgery to reduce the risk of complications during anesthesia.
-
Stopping certain medications , such as blood thinners, as directed by your surgeon.
-
Arrangements for post-surgery care, as you will need someone to assist you for a few days after the procedure.
10. Is laparoscopic diaphragmatic hernia repair covered by insurance?
Most insurance plans cover laparoscopic repair of a
diaphragmatic hernia when the procedure
is deemed medically necessary. It is important to
verify your insurance coverage beforehand
and check for any out-of-pocket costs or
requirements for pre-authorization.
The other Gastro procedures are:
Few Major Hospitals for Laparoscopy Repair of Diaphragmatic Hernia are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Hospitals For Laparoscopy Repair Of Diaphragmatic Hernia | Doctors For Laparoscopy Repair Of Diaphragmatic Hernia | Surgery Laparoscopy Repair Of Diaphragmatic Hernia | Cost Laparoscopy Repair Of Diaphragmatic Hernia | Treatment Laparoscopy Repair Of Diaphragmatic Hernia | Destinations Laparoscopy Repair Of Diaphragmatic Hernia | Risks Laparoscopy Repair Of Diaphragmatic Hernia | Laparoscopy Repair Of Diaphragmatic Hernia In India | Laparoscopy Repair Of Diaphragmatic Hernia Recovery | Laparoscopy Repair Of Diaphragmatic Hernia Information | Laparoscopy Repair Of Diaphragmatic Hernia Thailand | Laparoscopy Repair Of Diaphragmatic Hernia In Malaysia | Laparoscopy Repair Of Diaphragmatic Hernia Abroad | Laparoscopy Repair Of Diaphragmatic Hernia Donors | Laparoscopy Repair Of Diaphragmatic Hernia Overseas | Laparoscopy Repair Of Diaphragmatic Hernia Low Cost | Laparoscopy Repair Of Diaphragmatic Hernia In Singapore | Laparoscopy Repair Of Diaphragmatic Hernia In Argentina | Diaphragmatic Hernia | Bochdalek Hernia | Morgagni Hernia | Diaphragmatic Hernia | Pneumothorax | Collapsed Lung
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


