Laparoscopic-assisted intestinal resection is a minimally invasive surgical technique used to remove damaged, diseased, or cancerous sections of the intestine. This procedure is commonly performed to treat conditions such as colon cancer, Crohn’s disease, diverticulitis, intestinal obstructions, and trauma to the intestine.
Unlike traditional open surgery, where a large incision is made, laparoscopic surgery uses small incisions and specialized instruments, including a laparoscope, a thin tube with a camera attached, to view the area. Surgeons then manipulate small surgical tools through these incisions to perform the resection. This approach allows for greater precision, reduced pain, and shorter recovery times for patients.
Laparoscopic-assisted intestinal resection is often chosen for its ability to offer minimally invasive benefits while still achieving the same results as traditional open surgery. This method is associated with less tissue damage, smaller scars, and a quicker return to normal activities, making it a preferred choice for many patients.
Indications for Surgery
There are several medical conditions that can require an intestinal resection, particularly when the affected part of the intestine cannot be treated effectively through medication alone. These conditions include:
-
Colon Cancer: Cancerous growths in the colon may necessitate the removal of part of the colon (bowel resection). Laparoscopic-assisted resection is a less invasive alternative to open surgery.
-
Crohn’s Disease: This chronic inflammatory bowel disease often causes scarring and narrowing of the intestines, leading to blockages, ulcers, and fistulas. If medical treatment doesn’t relieve symptoms, surgery may be needed.
-
Diverticulitis: In this condition, small pouches (diverticula) form in the colon and become inflamed or infected. Severe cases may require resection.
-
Bowel Obstructions: Blockages in the intestine, often caused by adhesions from prior surgeries, hernias, or inflammatory diseases, may require a surgical approach to remove the obstruction.
-
Trauma: Intestinal injury from accidents, infections, or other trauma can necessitate the removal of damaged bowel segments.
Risk Factors for Needing Intestinal Resection
Several factors increase the likelihood of needing laparoscopic-assisted intestinal resection:
-
Age: The likelihood of developing certain conditions like cancer or diverticulitis increases with age, making older adults more prone to requiring surgery.
-
Chronic conditions: Conditions like Crohn’s disease or ulcerative colitis put individuals at higher risk for bowel disease and complications that may require surgery.
-
Previous surgeries: People who have had previous abdominal or gastrointestinal surgeries are more likely to develop adhesions, which may contribute to bowel obstruction.
-
Lifestyle factors: Poor dietary habits, including a high-fat, low-fiber diet, can contribute to the development of diverticulitis or other intestinal issues that may require surgery. Smoking also increases the risk of developing complications like Crohn’s disease.
Understanding these causes and risk factors is essential for early diagnosis and appropriate treatment planning.
Symptoms that could signal the need for laparoscopic-assisted intestinal resection vary depending on the underlying condition, but common warning signs include:
-
Chronic Abdominal Pain: Persistent pain in the abdomen that doesn’t improve with medication could indicate an underlying issue like bowel obstruction, Crohn’s disease, or diverticulitis.
-
Unexplained Weight Loss: When parts of the intestine are diseased or obstructed, they may not be able to absorb nutrients properly, leading to unexplained weight loss and malnutrition.
-
Chronic Diarrhea or Constipation: Disruptions in normal bowel function can indicate conditions like Crohn’s disease, colon cancer, or diverticulitis.
-
Rectal Bleeding: Any form of rectal bleeding, whether in the stool or as blood in the toilet bowl, should be taken seriously as it could indicate diverticulosis, colorectal cancer, or other serious conditions.
-
Bowel Obstruction: If a person experiences symptoms of obstruction, such as nausea, vomiting, bloating, and inability to pass gas or stool, this can signal a blockage that may require surgical intervention.
-
Signs of Infection: If a person is running a fever or experiencing increased pain, this could signal an infection in the abdominal cavity, requiring immediate medical attention.
Patients exhibiting any of these signs or symptoms should seek medical evaluation as soon as possible to determine whether surgery is necessary.
Diagnosing the need for laparoscopic-assisted intestinal resection generally involves a combination of medical history review, physical examinations, and diagnostic imaging:
-
Medical History and Physical Examination: The doctor will review the patient's symptoms and medical history, which may include past abdominal surgeries, chronic conditions, or family history of gastrointestinal diseases like colorectal cancer. A thorough physical examination is also crucial in identifying signs of obstruction or inflammation.
-
Imaging Studies: Advanced imaging techniques are used to locate the problem area and determine its extent:
-
CT scans or MRI: These provide detailed images of the abdominal cavity and intestines, helping to detect tumors, blockages, or other abnormalities.
-
X-ray with Barium Contrast: A Barium study allows the doctor to visualize the intestines, detecting issues like narrowing or blockages.
-
-
Endoscopy: Endoscopic techniques like colonoscopy and sigmoidoscopy allow the doctor to directly visualize the colon or rectum and take biopsies if needed for further examination of suspicious tissue.
-
Blood Tests: These tests can reveal signs of infection, inflammation, or anemia, which may be indicative of a more serious condition like cancer or an infection that requires surgery.
The combination of these diagnostic tools helps the surgeon determine if laparoscopic-assisted resection is the best treatment option for the patient.
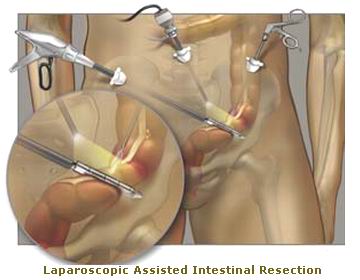
Surgical Procedure: Laparoscopic-Assisted Resection
The laparoscopic-assisted resection typically involves several steps:
-
Preparation: The patient is placed under general anesthesia. The surgeon makes several small incisions in the abdomen (usually 3-5). A laparoscope, equipped with a camera, is inserted through one of the incisions to provide a view of the inside of the abdomen.
-
Resection of the Diseased Bowel Section: The surgeon uses the laparoscopic instruments to carefully remove the damaged or diseased section of the intestine.
-
Reconnection (Anastomosis): The remaining healthy sections of the intestine are reconnected using staples or sutures, and the incision sites are closed.
-
Recovery: A typical hospital stay lasts 2-5 days, depending on the patient’s recovery progress. Most patients experience minimal post-operative pain and can return to daily activities more quickly than those who undergo traditional open surgery.
Other Treatment Options
-
Conventional Open Surgery: In certain cases, open surgery may be preferred if laparoscopic surgery is not possible due to the complexity or extent of the disease, obesity, or significant previous scarring.
-
Endoscopic Stenting: For certain types of obstructions, doctors may place a stent to hold the intestine open temporarily until further treatment can be done.
Although not all cases of intestinal disease can be prevented, certain lifestyle changes and proactive measures can reduce the risk:
Prevention of Bowel Disease
-
Diet: A healthy, fiber-rich diet can help prevent many forms of diverticulosis and can promote overall digestive health.
-
Avoid Smoking: Smoking has been linked to the development of Crohn’s disease and other gastrointestinal disorders.
-
Exercise: Regular physical activity can improve bowel function and reduce the risk of conditions that lead to resection.
Post-Surgical Management
Postoperative management focuses on recovery and reducing the risk of complications:
-
Pain Management: Post-surgical pain is usually well-controlled with medications such as NSAIDs and opiates.
-
Diet: Initially, patients will be on a liquid or soft food diet. Over time, they can gradually reintroduce solid foods.
-
Monitoring for Complications: Surgeons will closely monitor for signs of infection, anastomotic leaks, or bowel obstructions.
-
Regular Follow-ups: Regular check-ups after surgery are important for assessing recovery and addressing any ongoing symptoms or complications.
While laparoscopic-assisted resection is associated with fewer complications compared to open surgery, potential risks still exist. These include:
-
Anastomotic Leak: This occurs when the newly reconnected sections of the bowel leak, leading to infection and other severe complications.
-
Bowel Obstruction: Scar tissue or adhesions from surgery can lead to a blockage in the intestines.
-
Infection: As with any surgery, there is a risk of infection at the incision sites or within the abdominal cavity.
-
Bleeding: Excessive bleeding can occur during surgery or after the procedure.
-
Hernia: Incisions made during the surgery may result in an incisional hernia, where the intestine protrudes through the abdominal wall.
Recovery from laparoscopic-assisted intestinal resection is generally quicker than open surgery, but patients will need to make lifestyle adjustments to ensure a smooth recovery:
-
Dietary Changes: After surgery, patients may be advised to follow a low-fiber or bland diet for a period to allow the intestine to heal. Gradually, they can reintroduce fiber and other foods.
-
Physical Activity: Light physical activity, like walking, can aid in recovery, but patients should avoid heavy lifting or strenuous exercise for several weeks after surgery.
-
Emotional and Psychological Support: Undergoing surgery can be emotionally challenging. Patients should seek support from healthcare professionals or counseling if needed.
In conclusion, laparoscopic-assisted intestinal resection is a highly effective treatment option for many intestinal conditions. By understanding the causes, treatment options, and recovery process, patients can make informed decisions and work with their healthcare team to achieve the best possible outcomes.
1. What is laparoscopic assisted intestinal resection?
Laparoscopic assisted intestinal resection is a minimally invasive surgery used to remove a portion of the intestine that is damaged or diseased, such as due to cancer, Crohn’s disease, diverticulitis, or other conditions. The surgery is performed with small incisions and the help of a camera (laparoscope), making it less traumatic for the body compared to traditional open surgery.
2. Why would I need laparoscopic intestinal resection surgery?
This surgery is needed when a part of your intestine is diseased or damaged, causing symptoms such as severe pain, bleeding, blockages, or infections. Conditions like Crohn’s disease, diverticulitis, or colon cancer may require removal of a section of the intestine to restore normal function and relieve symptoms.
3. How is laparoscopic intestinal resection different from traditional surgery?
Laparoscopic intestinal resection is performed through several small incisions (usually about 1 to 2 cm) rather than one large incision as in traditional open surgery. A laparoscope, which is a thin tube with a camera, helps guide the surgeon during the procedure. This approach usually results in less pain, smaller scars, and quicker recovery compared to open surgery.
4. What are the benefits of laparoscopic assisted intestinal resection?
The benefits of laparoscopic surgery include:
-
Smaller incisions, which result in less pain and a lower risk of infection.
-
Shorter hospital stays and faster recovery times.
-
Less scarring.
-
Reduced blood loss during surgery.
-
Quicker return to normal activities compared to open surgery.
5. How is laparoscopic intestinal resection performed?
The procedure is performed under general anesthesia. The surgeon makes several small incisions in the abdomen and inserts a laparoscope and other surgical instruments. The affected section of the intestine is identified, removed, and the healthy parts are reconnected. In some cases, the procedure may be converted to open surgery if complications arise.
6. What are the risks associated with laparoscopic intestinal resection?
While laparoscopic intestinal resection is generally considered safe, there are risks involved. These include infection, bleeding, injury to surrounding organs (such as the bladder or blood vessels), leakage from the surgical site, blood clots, and complications related to anesthesia. Your surgeon will discuss these risks and help minimize them.
7. What is the recovery time for laparoscopic intestinal resection?
Recovery time for laparoscopic intestinal resection is typically quicker than for open surgery. Most patients can go home within 2 to 3 days after surgery, though it may take 2 to 4 weeks for you to return to normal activities. You will need to follow a special diet and avoid heavy lifting or strenuous activities during recovery.
8. What should I expect during recovery after laparoscopic intestinal resection?
During recovery, you may experience some discomfort, bloating, or gas, but these symptoms should improve over time. You may need to follow a special diet, which may include clear liquids initially and gradually move to soft foods. Your surgeon may also recommend avoiding heavy lifting or strenuous activities for several weeks. Regular follow-up visits are important to monitor your recovery.
9. Are there any lifestyle changes needed after the surgery?
After surgery, it’s important to follow a healthy diet to help your intestines heal. Gradually reintroduce foods to your diet as recommended by your doctor. You may need to avoid high-fat, high-fiber, or spicy foods temporarily. You should also avoid heavy lifting and strenuous activities while recovering, and follow your surgeon’s instructions on when to resume normal activities.
10. What happens if the surgery is not performed?
If laparoscopic intestinal resection is not performed, the condition causing the damaged or diseased section of the intestine may worsen. This can lead to complications such as intestinal blockages, chronic pain, infections, and a decrease in the quality of life. In some cases, untreated conditions may become life-threatening.
The other Gastro procedures are:
Few Major Hospitals for Laparoscopic Assisted Intestinal Resection are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.