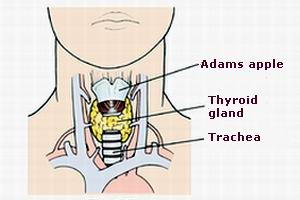
A thyroidectomy is a surgical procedure in which all or part of the thyroid gland is removed. The thyroid is a butterfly-shaped gland located at the base of the neck, and it plays an essential role in regulating metabolism, growth, and energy production by releasing thyroid hormones, such as thyroxine (T4) and triiodothyronine (T3). This gland influences almost every cell in the body, and imbalances in its function can lead to significant health issues.
Thyroidectomy is most commonly performed for conditions such as thyroid cancer, goiters (enlarged thyroid), benign thyroid nodules, and hyperthyroidism that cannot be managed by medication alone. The decision to perform a thyroidectomy depends on factors like the size and type of thyroid disorder, the risk of malignancy, and the impact of the thyroid condition on the patient’s health.
Depending on the nature of the thyroid problem, thyroidectomy can be categorized into different types:
-
Total thyroidectomy: Removal of the entire thyroid gland.
-
Partial thyroidectomy: Removal of only a portion of the thyroid gland.
-
Hemithyroidectomy: Removal of one lobe of the thyroid gland.
The surgery can be performed using traditional open surgery, minimally invasive approaches, or robot-assisted surgery depending on the patient's specific needs.
Thyroidectomy is primarily performed to address various thyroid conditions. The conditions requiring this surgery can be benign or malignant, and understanding the causes and risk factors behind these conditions is crucial for determining the need for the procedure.
Common Causes for Thyroidectomy:
-
Thyroid Cancer:
-
Thyroid cancer is one of the leading causes of thyroidectomy. Cancer can arise in any part of the thyroid and spread to other areas of the body if not treated effectively. Common types of thyroid cancer include:
-
Papillary thyroid cancer: The most common form, typically slow-growing and usually treatable with surgery.
-
Follicular thyroid cancer: A more aggressive form than papillary cancer, sometimes requiring removal of surrounding lymph nodes.
-
Medullary thyroid cancer: This type arises from the C-cells of the thyroid and is often associated with genetic mutations, such as MEN2 syndrome.
-
Anaplastic thyroid cancer: A rare but aggressive form of thyroid cancer that requires rapid surgical intervention.
-
-
-
Benign Thyroid Disorders:
-
Conditions such as benign thyroid nodules, goiters, and multinodular goiters (multiple non-cancerous lumps in the thyroid) may require thyroidectomy, especially if the goiter becomes large enough to cause difficulty swallowing, breathing, or causes cosmetic concerns.
-
-
Hyperthyroidism:
-
Hyperthyroidism is a condition in which the thyroid produces too much thyroid hormone. It can result from Graves’ disease (an autoimmune disorder) or toxic multinodular goiter. If medications or radioactive iodine therapy do not effectively manage hyperthyroidism, a thyroidectomy may be necessary to remove part or all of the thyroid gland.
-
-
Graves' Disease:
-
Graves’ disease is the most common cause of hyperthyroidism. It occurs when the immune system attacks the thyroid, causing it to become overactive. In severe cases, surgery is required if the disease does not respond to anti-thyroid drugs or radioactive iodine treatment.
-
-
Thyroid Nodules:
-
Benign thyroid nodules (solid or cystic lumps in the thyroid) are common and often discovered during routine physical exams or imaging tests. If a nodule grows large or is causing symptoms like discomfort, difficulty swallowing, or changes in voice, surgical removal may be necessary.
-
-
Goiter:
-
A goiter is an enlarged thyroid gland, often caused by iodine deficiency or autoimmune diseases like Hashimoto’s thyroiditis. A large goiter can cause problems like difficulty swallowing, a sensation of a lump in the throat, and in rare cases, obstruction of the trachea. Surgery may be necessary when these symptoms become severe.
-
Risk Factors for Thyroidectomy:
-
Age:
-
Thyroid conditions such as cancer or goiter are more common in adults over the age of 40. Hyperthyroidism and benign thyroid nodules also become more prevalent as people age, leading to a higher likelihood of requiring thyroidectomy.
-
-
Gender:
-
Women are more likely to develop thyroid issues, particularly thyroid cancer and benign thyroid disorders, compared to men. Women in their 30s to 60s are more prone to developing thyroid problems that require surgery.
-
-
Family History:
-
A family history of thyroid cancer or other thyroid disorders increases the risk of developing similar conditions, potentially leading to thyroidectomy. Genetic mutations linked to medullary thyroid cancer or multinodular goiter may also predispose individuals to thyroid-related issues.
-
-
Radiation Exposure:
-
Individuals who have been exposed to radiation, particularly in the head and neck area (e.g., for childhood cancers), are at an increased risk of developing thyroid cancer later in life.
-
-
Autoimmune Conditions:
-
People with autoimmune diseases such as Graves’ disease or Hashimoto’s thyroiditis are more likely to develop thyroid problems that may require surgical intervention.
-
Thyroid surgery is often recommended when the thyroid is diseased, and patients exhibit symptoms that interfere with their daily lives. These symptoms can vary depending on whether the thyroid condition is related to hypothyroidism, hyperthyroidism, thyroid cancer, or benign thyroid disorders.
Common Symptoms that May Lead to Thyroidectomy:
-
Neck Swelling or Lump:
-
A visible lump or swelling in the neck is the most common symptom of thyroid problems. In cases of goiters or thyroid nodules, a noticeable mass may develop in the neck, which may be painless or tender.
-
-
Difficulty Swallowing or Breathing:
-
An enlarged thyroid, or goiter, can exert pressure on the esophagus or trachea, leading to difficulty swallowing (dysphagia) or breathing (dyspnea). This can become more pronounced as the goiter grows in size.
-
-
Hyperthyroid Symptoms:
-
Symptoms of hyperthyroidism, including weight loss, irritability, nervousness, heat intolerance, and rapid heartbeat, may indicate the need for thyroidectomy when other treatments fail to control the condition.
-
-
Hypothyroid Symptoms:
-
Conversely, hypothyroidism (underactive thyroid) can cause symptoms like fatigue, weight gain, cold intolerance, constipation, and depression. If the condition is caused by a structural problem, such as a goiter, surgery may be necessary.
-
-
Hoarseness or Voice Changes:
-
A hoarse voice or changes in speech can be a sign of thyroid cancer or nerve involvement due to enlarged thyroid tissue. Surgery may be required to remove the abnormal tissue causing these symptoms.
-
-
Pain or Tenderness in the Neck:
-
Pain in the neck or tenderness associated with swallowing may indicate an infected thyroid gland (thyroiditis) or an inflamed nodule, potentially requiring surgical treatment.
-
Before proceeding with thyroidectomy, doctors use a variety of diagnostic tools to confirm the diagnosis and determine the extent of the thyroid condition. These diagnostic tests help guide treatment decisions and identify whether surgery is the most appropriate option.
Diagnostic Methods:
-
Physical Examination:
-
The doctor will physically examine the neck to assess the size, shape, and texture of the thyroid. The presence of a lump or enlarged gland can often be felt during this examination.
-
-
Blood Tests:
-
Thyroid function tests measure the levels of thyroid hormones, including T3, T4, and TSH (thyroid-stimulating hormone), to assess whether the thyroid is overactive or underactive. Abnormal levels may suggest hyperthyroidism or hypothyroidism, guiding treatment.
-
-
Ultrasound:
-
Thyroid ultrasound is used to evaluate the size, location, and structure of thyroid nodules or goiters. It helps differentiate between benign and suspicious masses and provides valuable information for surgical planning.
-
-
Fine Needle Aspiration (FNA) Biopsy:
-
If a thyroid nodule is detected, an FNA biopsy is often performed to obtain a sample of tissue from the nodule. This helps determine if the nodule is benign or malignant and whether further surgical intervention is necessary.
-
-
Thyroid Scintigraphy (Radioactive Iodine Scan):
-
This scan uses a small amount of radioactive iodine to evaluate the function of the thyroid gland and identify areas of abnormal growth or activity.
-
-
CT/MRI Scans:
-
In some cases, a CT scan or MRI may be used to assess the extent of disease, especially when thyroid cancer is suspected or if large goiters are affecting surrounding tissues.
-
Treatment for thyroid conditions depends on the diagnosis, and thyroidectomy is often the most effective solution when other methods fail to provide relief. Here are the main treatment options:
Types of Thyroidectomy:
-
Total Thyroidectomy:
-
The complete removal of the thyroid gland is often performed for thyroid cancer or when a goiter or large nodule is causing significant symptoms. After total thyroidectomy, patients will require lifelong thyroid hormone replacement therapy to maintain normal metabolism.
-
-
Partial Thyroidectomy:
-
Only part of the thyroid gland is removed. This may be performed for benign thyroid conditions or when cancer is not a concern. The remaining portion of the thyroid may continue to produce enough hormones, reducing the need for hormone replacement.
-
-
Minimally Invasive Approaches:
-
For smaller thyroid conditions, minimally invasive techniques like robotic-assisted thyroidectomy or endoscopic thyroidectomy are used. These methods involve smaller incisions, less pain, quicker recovery, and fewer complications compared to traditional surgery.
-
-
Radioactive Iodine Therapy:
-
After thyroidectomy, especially in cases of thyroid cancer, radioactive iodine may be used to destroy any remaining thyroid tissue or cancer cells. This therapy is effective for both hyperthyroidism and thyroid cancer.
-
-
Medications:
-
Antithyroid drugs like methimazole are used for hyperthyroidism before surgery, while levothyroxine is used after thyroidectomy to replace the hormones once produced by the thyroid.
-
While some thyroid conditions cannot be prevented, certain measures can reduce the risk or help manage thyroid health effectively.
Prevention:
-
Adequate Iodine Intake:
-
Iodine is essential for proper thyroid function. Ensuring an adequate intake of iodine-rich foods (e.g., seafood, dairy products, iodized salt) can prevent conditions like goiter.
-
-
Avoid Excessive Radiation Exposure:
-
Limiting exposure to radiation, especially in childhood or adolescence, can reduce the risk of thyroid cancer later in life.
-
Post-Surgery Management:
-
Thyroid Hormone Replacement:
-
After total thyroidectomy, patients must take synthetic thyroid hormones, such as levothyroxine, to replace the thyroid hormones that the body can no longer produce.
-
-
Regular Monitoring:
-
Regular blood tests to measure TSH, T3, and T4 levels are essential after thyroidectomy to ensure the correct dosage of hormone replacement.
-
-
Follow-Up Care:
-
Periodic follow-up visits with an endocrinologist or surgeon are crucial to monitor recovery, assess for any recurrence of cancer (if relevant), and manage long-term hormone therapy.
-
While thyroidectomy is a generally safe procedure, it comes with some potential risks and complications that should be considered:
-
Infection:
-
Any surgery carries the risk of infection at the incision site. Following post-operative care instructions and taking antibiotics can help reduce this risk.
-
-
Nerve Damage:
-
The recurrent laryngeal nerve, which controls the vocal cords, can be damaged during surgery, resulting in hoarseness or difficulty speaking.
-
-
Hypoparathyroidism:
-
The parathyroid glands are located near the thyroid and may be inadvertently damaged during surgery. This can lead to low calcium levels in the blood, causing symptoms like muscle cramps and numbness.
-
-
Bleeding:
-
Excessive bleeding can occur, especially if blood vessels in the thyroid region are affected.
-
-
Thyroid Storm:
-
In rare cases, particularly for patients with hyperthyroidism, a thyroid storm can occur after surgery, leading to an extreme increase in thyroid hormones and life-threatening symptoms.
-
After thyroidectomy, most patients lead healthy lives, but ongoing management is crucial for a smooth recovery.
Recovery and Lifestyle Adjustments:
-
Thyroid Hormone Therapy:
-
After surgery, patients must take thyroid hormone replacement medication to prevent hypothyroidism and maintain metabolic balance. It is essential to take this medication consistently.
-
-
Regular Exercise:
-
Physical activity can help improve energy levels and maintain a healthy weight, especially if there are changes in metabolism due to the loss of thyroid function.
-
-
Mental and Emotional Support:
-
Recovery from thyroid surgery can have emotional and psychological effects. It may be helpful to seek support from counseling, therapy, or support groups for people with thyroid disease.
-
-
Diet and Nutrition:
-
A balanced diet rich in essential nutrients helps maintain overall health. Calcium and vitamin D supplements may be necessary if hypoparathyroidism develops.
-
1. What is thyroidectomy?
Thyroidectomy is a surgical procedure in which all or part of the thyroid gland is removed. The thyroid is a butterfly-shaped gland located in the neck that produces hormones that regulate metabolism, heart rate, and body temperature. Thyroidectomy is typically performed to treat thyroid diseases such as thyroid cancer, hyperthyroidism, or benign thyroid nodules.
2. Why would I need a thyroidectomy?
A thyroidectomy may be necessary for several reasons, including:
-
Thyroid cancer: Removal of part or all of the thyroid may be required to treat cancer.
-
Hyperthyroidism: If the thyroid becomes overactive and cannot be controlled by medication.
-
Benign thyroid nodules: If nodules are large or causing symptoms such as difficulty swallowing or breathing.
-
Goiter: An enlarged thyroid that is causing discomfort or difficulty with swallowing.
3. What are the different types of thyroidectomy?
There are different types of thyroidectomy, depending on the extent of thyroid tissue removal:
-
Total thyroidectomy: Removal of the entire thyroid gland.
-
Partial (or hemithyroidectomy): Removal of part of the thyroid gland, usually when a tumor or nodule is localized to one side.
-
Subtotal thyroidectomy: Partial removal of the thyroid gland, leaving some tissue behind.
-
Lobectomy: Removal of one lobe of the thyroid.
4. How is thyroidectomy performed?
Thyroidectomy is generally performed under general anesthesia. The surgeon makes a small incision in the neck, typically along the natural skin folds, to access the thyroid gland. The gland is carefully removed, and if cancer is present, lymph nodes may also be taken for examination. The incision is closed with sutures, and the patient is monitored during recovery.
5. What are the risks and complications of thyroidectomy?
Although thyroidectomy is generally safe, there are some risks and potential complications, including:
-
Damage to the recurrent laryngeal nerve: This nerve controls the vocal cords, and damage can result in voice changes or hoarseness.
-
Hypothyroidism: If the entire thyroid is removed, you may develop hypothyroidism (underactive thyroid) and will need to take thyroid hormone replacement.
-
Infection or bleeding: As with any surgery, there is a risk of infection or bleeding at the surgical site.
-
Calcium imbalances: The parathyroid glands, which regulate calcium levels, are located near the thyroid and may be affected during surgery.
6. What is the recovery time after thyroidectomy?
Recovery time varies depending on the type of thyroidectomy performed and the individual’s overall health. Most patients stay in the hospital for 1 to 2 days after the surgery. Full recovery can take 1 to 2 weeks, with most people returning to light activities within a few days. Patients who have total thyroidectomy may need to take thyroid hormone replacement for life.
7. Will I need to take thyroid hormone after thyroidectomy?
If the entire thyroid gland is removed (total thyroidectomy), you will need to take thyroid hormone replacement for life. This is to maintain normal metabolism and bodily functions. If only part of the thyroid is removed, your remaining thyroid tissue may still produce enough hormones, but your doctor will monitor your levels to determine if medication is necessary.
8. What are the potential side effects of thyroid hormone replacement therapy?
Some patients may experience side effects from thyroid hormone replacement therapy, including:
-
Weight gain or loss
-
Increased heart rate
-
Insomnia
-
Nervousness or anxiety
-
Increased sweating or heat intolerance
Adjusting the dosage can help minimize these side effects, and your doctor will monitor your thyroid hormone levels regularly.
9. How will thyroidectomy affect my voice?
Most patients experience some hoarseness or changes in their voice immediately following thyroidectomy, especially if the recurrent laryngeal nerve was affected during surgery. However, this is usually temporary, and the voice typically returns to normal within a few weeks. In rare cases, permanent voice changes may occur if the nerve is damaged. Your surgeon will take care to avoid damaging the nerve during surgery.
10. Can I resume normal activities after thyroidectomy?
You can usually resume most normal activities within a few weeks after thyroidectomy, depending on your recovery. It is important to avoid strenuous exercise and heavy lifting for at least 1 to 2 weeks. If you are prescribed thyroid hormone replacement, you will need to follow your doctor’s instructions on when to take the medication and when to schedule follow-up visits to monitor your hormone levels.
The other general procedures are:
Few Major Hospitals for Appendicectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



