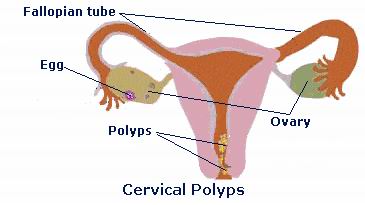
Cervical polyps are small, often benign (non-cancerous) growths that develop on the cervix—the lower part of the uterus that connects to the vagina. These growths are typically red or purple, soft, and usually round or finger-like in shape. Cervical polyps are most commonly found in women between the ages of 40 and 50, but they can occur at any age, even in younger women and postmenopausal women.
Cervical polyps are typically asymptomatic and are often discovered during routine gynecological exams or screenings, such as Pap smears or pelvic exams. While cervical polyps are generally not dangerous, they can sometimes cause problems, such as abnormal bleeding, pelvic pain, or infertility if they are large or cause irritation. In rare cases, cervical polyps can become infected or lead to complications during pregnancy or childbirth.
The exact cause of cervical polyps is not fully understood, but they are believed to be influenced by factors such as hormonal imbalances, infections, or chronic inflammation. While most cervical polyps do not cause serious health issues, they can lead to problems that affect a woman's menstrual cycle, fertility, and reproductive health.
Cervical polyps typically develop due to factors that affect the cervix and its lining. Some women may develop polyps due to hormonal changes, infections, or other conditions that lead to inflammation or abnormal growth of tissue in the cervix.
Causes of Cervical Polyps:
-
Hormonal Imbalance:
-
Estrogen, a hormone primarily produced in the ovaries, plays a role in the growth and maintenance of the endometrial lining (the uterine lining). An imbalance in estrogen levels may stimulate the development of cervical polyps. This is particularly true for women in their reproductive years when hormonal fluctuations are most prevalent. The overproduction of estrogen may cause abnormal cell growth, leading to the formation of polyps on the cervix.
-
-
Chronic Inflammation:
-
Chronic inflammation of the cervix or the surrounding tissues can lead to the development of polyps. Cervicitis, or inflammation of the cervix, can be caused by repeated infections, irritants, or prolonged use of certain contraceptives, leading to the formation of polyps. Inflammatory processes can cause the cervix to become more susceptible to abnormal tissue growth.
-
-
Infections:
-
Pelvic infections, especially bacterial infections or sexually transmitted infections (STIs) like chlamydia and gonorrhea, can increase the likelihood of polyps. These infections cause irritation and inflammation of the cervix, creating an environment that may encourage polyp formation. Additionally, human papillomavirus (HPV), a virus associated with cervical cancer, has been linked to abnormal changes in the cervix, potentially leading to polyps.
-
-
Previous Uterine Procedures:
-
Women who have undergone certain uterine procedures, such as a D&C (dilation and curettage), hysteroscopy, or cervical conization, are at an increased risk for developing cervical polyps. These procedures can cause minor trauma to the cervix, which may promote abnormal cell growth in the area and result in polyps.
-
-
Poor Blood Circulation:
-
Areas with poor blood circulation in the cervix can increase the likelihood of polyps. Poor circulation can lead to an accumulation of blood or fluid in certain areas, resulting in the development of growths like polyps. This may occur due to certain structural abnormalities, pelvic congestion, or other underlying health conditions that affect the vascular system.
-
Risk Factors for Cervical Polyps:
-
Age:
-
Women between the ages of 40 and 50 are at higher risk for developing cervical polyps due to hormonal changes during perimenopause. However, polyps can occur at any age, including in young women, especially those with hormonal imbalances.
-
-
Pregnancy:
-
Pregnancy increases the risk of developing cervical polyps. Hormonal changes during pregnancy, especially elevated levels of estrogen, can promote the growth of polyps in the cervix. Additionally, women who have had multiple pregnancies or childbirths may be more prone to developing polyps.
-
-
Chronic Infections:
-
A history of chronic pelvic infections, including endometritis (infection of the uterine lining), PID (pelvic inflammatory disease), or recurrent cervicitis, increases the risk of cervical polyps. These conditions cause long-term inflammation, which may result in the formation of polyps.
-
-
Use of Birth Control:
-
Some oral contraceptives or IUDs (intrauterine devices) may contribute to the development of cervical polyps. The hormonal effects of these contraceptives, particularly those that involve high levels of estrogen, may increase the likelihood of abnormal tissue growth on the cervix.
-
-
Genetic Predisposition:
-
Although the role of genetics in cervical polyp formation is not fully understood, women with a family history of uterine or cervical polyps may have an increased risk of developing them.
-
Most cervical polyps are painless and asymptomatic, especially if they are small. Many women with cervical polyps may not know they have them unless they are discovered during a routine pelvic exam. However, some larger polyps or those that cause irritation to the cervix can lead to noticeable symptoms.
Common Symptoms of Cervical Polyps:
-
Abnormal Vaginal Bleeding:
-
The most common symptom of cervical polyps is abnormal vaginal bleeding. This may include:
-
Postcoital bleeding (bleeding after intercourse).
-
Irregular periods (spotting between periods).
-
Heavy menstrual bleeding or menorrhagia (prolonged periods).
-
Postmenopausal bleeding, which should always be investigated further as it may signal other underlying conditions.
-
-
-
Pelvic Pain or Discomfort:
-
Larger cervical polyps or those that are irritated may cause mild pelvic discomfort or pain. This pain is usually localized to the cervix and may be more noticeable during intercourse or pelvic exams.
-
-
Increase in Vaginal Discharge:
-
In some cases, cervical polyps may cause an increase in vaginal discharge. The discharge may be yellow, white, or sometimes bloody. The discharge could occur if the polyp becomes irritated or infected.
-
-
Visible Polyps:
-
Large polyps can sometimes be visible during a pelvic exam. These polyps typically appear as red, purple, or brown growths protruding from the cervix. Polyps can be soft, round, or finger-like in shape.
-
-
Painful Menstrual Cycles:
-
Some women with cervical polyps may experience painful menstrual cycles (dysmenorrhea), caused by the pressure the polyp exerts on the uterine walls or cervix.
-
Cervical polyps are often detected during a routine pelvic examination or a Pap smear. If the doctor suspects the presence of polyps, they may perform additional tests to confirm the diagnosis and assess the size and location of the polyps.
Diagnostic Methods:
-
Pelvic Examination:
-
The first step in diagnosing cervical polyps is a routine pelvic exam. During the exam, the doctor may visually inspect the cervix for any growths or abnormal tissue. The polyps may be felt or seen as protrusions on the cervix.
-
-
Colposcopy:
-
If the doctor detects a polyp, they may recommend a colposcopy to examine the cervix in more detail. A colposcope is a specialized microscope used to magnify the cervix, allowing the doctor to closely examine the polyp. If necessary, a cervical biopsy may be taken during the procedure to rule out other conditions, such as cervical cancer.
-
-
Hysteroscopy:
-
A hysteroscopy may be performed to examine the inside of the uterus and the cervix. A hysteroscope, a small tube with a camera, is inserted through the cervix, allowing the doctor to view the polyp and assess its size and location. This is a minimally invasive procedure and can also be used to remove the polyp.
-
-
Ultrasound:
-
In some cases, a transvaginal ultrasound may be used to examine the uterus and cervix. This is particularly useful if the polyps are suspected to be located deeper in the uterine lining or if the doctor needs more detailed images of the reproductive organs.
-
-
Biopsy:
-
If the polyp is large or there are concerns about its nature, a biopsy may be performed during colposcopy or hysteroscopy. The biopsy will help determine if the polyp is benign or cancerous.
-
Treatment for cervical polyps typically depends on their size, symptoms, and whether they are causing complications such as bleeding or infertility. In most cases, polyps can be easily removed through a simple procedure.
Non-Surgical Treatments:
-
Observation:
-
If the polyp is small and not causing any symptoms, a doctor may recommend simply monitoring the condition. Regular pelvic exams or follow-up screenings may be sufficient to ensure that the polyp does not grow or cause further issues.
-
Surgical Treatments:
-
Polypectomy:
-
Polypectomy is the most common treatment for cervical polyps. This procedure involves removing the polyp from the cervix. The procedure is typically done in the office using local anesthesia. For small polyps, the doctor may gently twist or cut the polyp off. Larger polyps may require the use of instruments like forceps or a hysteroscope for removal.
-
-
Cauterization:
-
After removing the polyp, the cervix may be cauterized using heat or chemical solutions to prevent any bleeding and to ensure the polyp does not regrow. This procedure is typically done after polypectomy to reduce the chances of recurrence.
-
-
Hysteroscopic Polypectomy:
-
For larger or more deeply embedded polyps, a hysteroscopic polypectomy may be performed. This involves using a hysteroscope to visualize and remove the polyp. The procedure is done under local or general anesthesia and is minimally invasive.
-
While there is no surefire way to prevent cervical polyps, certain practices can reduce the likelihood of developing them and help manage the condition effectively.
Prevention:
-
Regular Gynecological Exams:
-
Routine pelvic exams and Pap smears are essential for early detection of cervical polyps and other gynecological conditions. Regular screenings can help identify polyps before they cause significant issues.
-
-
Safe Sexual Practices:
-
Practicing safe sex and using barrier contraception such as condoms can reduce the risk of sexually transmitted infections (STIs), which may lead to cervical infections and polyps.
-
-
Prompt Treatment of Infections:
-
Timely treatment of any infections, particularly pelvic or vaginal infections, can prevent inflammation and scarring of the cervix, which may contribute to the formation of polyps.
-
-
Managing Hormonal Imbalances:
-
Women who experience symptoms of hormonal imbalances, such as irregular periods or excessive estrogen levels, should consult their doctor for appropriate evaluation and treatment to reduce the risk of developing cervical polyps.
-
Management:
-
Post-Treatment Follow-Up:
-
After treatment, women should continue to have regular follow-up visits with their gynecologist to ensure that the polyps do not return. The doctor may recommend routine pelvic exams or ultrasounds to monitor the cervix.
-
-
Fertility Considerations:
-
For women with cervical polyps who are trying to conceive, treatment can help improve the chances of pregnancy. Polypectomy improves fertility by eliminating any growths that may interfere with the implantation of an embryo. Women with persistent infertility should seek fertility evaluation to rule out other contributing factors.
-
Although cervical polyps are typically benign and do not cause serious health problems, there are a few potential complications if they are left untreated or become infected.
Potential Complications:
-
Abnormal Bleeding:
-
Uncontrolled or excessive bleeding caused by cervical polyps can lead to anemia or other health issues. Abnormal bleeding may be distressing and require prompt medical attention.
-
-
Infection:
-
Cervical polyps, if left untreated, can become infected, leading to pelvic pain, fever, and abnormal discharge. An infection may also cause inflammation and damage to the cervix.
-
-
Misdiagnosis:
-
In rare cases, polyps may be confused with cervical cancer. A proper diagnosis is crucial to ensure that the growth is benign and not cancerous.
-
Most women with cervical polyps can lead normal, healthy lives once the condition is diagnosed and treated. However, for women who experience symptoms such as abnormal bleeding, pelvic pain, or infertility, managing the condition effectively is key.
Living with Cervical Polyps:
-
Emotional Support:
-
The emotional impact of dealing with abnormal bleeding or fertility challenges due to cervical polyps can be significant. Seeking psychological support or joining support groups for women with gynecological conditions can help alleviate stress and anxiety.
-
-
Fertility and Pregnancy:
-
Women who experience infertility due to cervical polyps should consult a fertility specialist for additional support and treatment. Removal of polyps can increase the chances of successful conception.
-
-
Ongoing Monitoring:
-
Regular follow-up exams are important to ensure the polyps do not recur. Women who have undergone polypectomy should continue to have annual gynecological exams.
-
1. What are cervical polyps?
Cervical polyps are small, benign growths that form on the cervix, the lower part of the uterus that connects to the vagina. These polyps can vary in size and shape and are often pale or red in color. They are typically non-cancerous, although some may occasionally cause symptoms such as bleeding, discharge, or pain during intercourse.
2. What causes cervical polyps?
The exact cause of cervical polyps is not entirely understood, but several factors may contribute to their development:
-
Hormonal imbalances: Changes in estrogen levels may play a role in the formation of polyps, which is why they are more common in women of childbearing age or those on hormone therapy.
-
Chronic inflammation: Long-term inflammation of the cervix due to infections or other conditions can lead to the growth of polyps.
-
Infection: Certain infections, particularly those caused by bacteria or sexually transmitted infections (STIs), can increase the risk of developing cervical polyps.
3. What are the symptoms of cervical polyps?
In many cases, cervical polyps do not cause any symptoms and are discovered during a routine pelvic exam. However, when symptoms do occur, they can include:
-
Abnormal vaginal bleeding: This can include spotting between periods, after intercourse, or after menopause.
-
Increased vaginal discharge, which may be clear or mucousy.
-
Pain during intercourse or pelvic discomfort.
-
Inflammation around the cervix, leading to swelling or tenderness.
Most cervical polyps are harmless, but if you experience unusual bleeding or discomfort, it’s important to see a healthcare provider.
4. How are cervical polyps diagnosed?
Cervical polyps are usually discovered during a routine pelvic exam, where the healthcare provider may notice growths on the cervix. To confirm the diagnosis, further tests may be performed, such as:
-
Colposcopy: A more detailed examination of the cervix using a magnifying instrument to closely examine any abnormalities.
-
Biopsy: If the polyp appears unusual or if there is concern about cancer, a small sample of tissue may be taken for further testing.
-
Pap smear: Although not specifically for polyps, a Pap test may help identify any abnormalities in the cervix.
5. Are cervical polyps dangerous?
Most cervical polyps are benign and do not pose any serious health risks. However, in rare cases, a polyp may be associated with cervical cancer. This is why polyps that cause symptoms such as unusual bleeding or those that appear irregular in shape or size should be evaluated by a healthcare provider. Early detection and treatment of any abnormal growths on the cervix can help prevent potential complications.
6. How are cervical polyps treated?
The treatment for cervical polyps typically involves their removal, especially if they cause symptoms such as abnormal bleeding. Treatment options include:
-
Polypectomy: A simple procedure in which the polyp is removed from the cervix using a small surgical instrument. This can often be done in a doctor’s office with local anesthesia.
-
Electrocautery: In some cases, a polyp may be removed using heat to burn it off.
-
Cryotherapy: Freezing the polyp to destroy it may also be an option.
After removal, the polyp is usually sent for analysis to ensure it is benign.
7. Is the removal of cervical polyps painful?
The removal of cervical polyps is usually a quick and simple procedure. For most women, local anesthesia is used to numb the cervix, and the procedure itself is not painful, though there may be some mild cramping or discomfort afterward. It is common to experience some spotting or light bleeding for a few days after the procedure. Most women can return to their normal activities shortly after the procedure.
8. Can cervical polyps come back after removal?
While cervical polyps can be removed safely, it is possible for new polyps to develop over time, particularly if the underlying causes, such as hormonal imbalances or chronic inflammation, are not addressed. However, the recurrence rate is low, and most women do not experience repeated issues after treatment. Regular follow-up appointments and pelvic exams can help monitor for any future polyps.
9. Can I prevent cervical polyps?
There is no surefire way to prevent cervical polyps, but there are some measures you can take to reduce the risk:
-
Regular gynecological exams: Regular checkups and Pap smears can help detect abnormalities early.
-
Avoid STIs: Practicing safe sex and getting regular screenings for sexually transmitted infections (STIs) can help reduce the risk of infections that may contribute to the development of polyps.
-
Good hygiene: Maintaining good vaginal hygiene can help reduce the risk of infections that might lead to inflammation or the development of polyps.
-
Managing hormonal levels: If you are on hormone therapy, discussing the risks with your healthcare provider may help reduce the chances of developing polyps.
10. Is cervical polyp removal covered by insurance?
Yes, the removal of cervical polyps is typically covered by most health insurance plans if the procedure is deemed medically necessary. If the polyp is causing symptoms, such as abnormal bleeding or pain, insurance typically covers the cost of removal. However, it’s important to check with your insurance provider for specific coverage details, including co-pays, deductibles, and any out-of-pocket costs related to the procedure.
The other Gynecology Procedures are:
Few Major Hospitals for Cervical Polyps are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



