Sterilization is a permanent form of contraception, offering individuals and couples a reliable, irreversible method to prevent pregnancy. However, some individuals or couples may later experience a change in their life circumstances, such as remarriage or a desire for more children. This shift in perspective may lead them to consider reversal of sterilization.
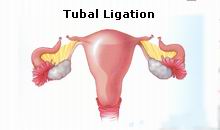
Reversal of sterilization is a medical procedure that allows individuals who previously underwent sterilization—whether through tubal ligation (in women) or vasectomy (in men)—to regain fertility. The goal of the procedure is to reconnect the fallopian tubes in women or the vas deferens in men, thus restoring the pathway for sperm to reach the eggs or for eggs to travel to the uterus, depending on the sex and sterilization method.
While reversal of sterilization is possible, it is not guaranteed to be successful, and the chances of success depend on a range of factors. Understanding the options available for reversing sterilization, the procedures involved, the likelihood of success, and the risks and challenges associated with this decision are crucial for individuals considering this option.
There are several reasons why individuals or couples may choose to pursue reversal of sterilization. However, the procedure is not always straightforward, and understanding the causes, as well as the risk factors, is important before moving forward with the surgery.
Causes for Seeking Reversal of Sterilization
-
Desire for More Children:
The most common reason individuals choose to undergo sterilization reversal is the desire to have more children. Over time, people’s circumstances, relationships, and life goals may change, prompting a reconsideration of previous decisions made regarding family planning. -
Regret Over the Permanent Nature of Sterilization:
Some individuals may have undergone sterilization at a young age and later regretted the decision when they realized they desired children later in life. This is particularly common for women who undergo tubal ligation in their 20s or 30s when they may not have anticipated changes in their family structure. -
Health or Medical Reasons:
In some cases, individuals who originally chose sterilization may have experienced health-related issues that now make pregnancy less risky or medically advisable. For example, women who initially had conditions that made pregnancy dangerous may experience improvements in their health, prompting them to seek reversal. -
Change in Relationship Status:
A change in relationship status, such as remarriage or the end of a partnership, may also influence the decision to reverse sterilization. Individuals who are remarried may want to have children with their new partner, especially if they had previously undergone sterilization when they were in a different relationship. -
Desire for Fertility Preservation:
Some individuals may not wish to pursue a reversal immediately but are considering future fertility options. In these cases, the reversal procedure may help preserve the potential for future pregnancy, even if they do not want to conceive immediately.
Risk Factors Affecting the Success of Reversal of Sterilization
The success of sterilization reversal can vary significantly from one individual to another. Several factors influence the likelihood of a successful procedure:
-
Age: Women over the age of 40 may have a lower chance of achieving pregnancy following a sterilization reversal due to the natural decline in fertility associated with age. The quality of the eggs decreases as a woman ages, and this can affect the chances of conception.
-
Time Since Sterilization: The longer it has been since the sterilization procedure, the lower the chances of a successful reversal. As the fallopian tubes can develop scar tissue over time, it may become more difficult to reconnect the tubes effectively. For men, the success of vasectomy reversal also diminishes over time, especially if a significant period has passed since the vasectomy.
-
Method of Sterilization: Different sterilization techniques affect the reversibility of the procedure. Tubal ligation, for instance, is often easier to reverse compared to Essure (a method where small coils are inserted into the fallopian tubes), which can be more complicated due to the nature of the procedure and the materials used.
-
Scar Tissue and Tubal Damage: Scar tissue can form around the fallopian tubes or vas deferens, which can interfere with the procedure’s success. The extent of damage to the reproductive organs from the original sterilization procedure plays a key role in the reversal’s outcome.
-
Overall Health: A person’s overall reproductive health also impacts the success rate. Conditions such as endometriosis, pelvic inflammatory disease (PID), or fibroids can complicate the procedure and lower the chances of success.
While reversal of sterilization may restore fertility, it is important to understand the possible symptoms and signs following the procedure. The success of the reversal can take time to assess, and recovery may include a range of physical and emotional symptoms.
Post-Operative Symptoms
-
Pain and Discomfort:
After the reversal procedure, mild abdominal pain and discomfort are common. This is typically caused by the healing process and the manipulation of the reproductive organs during surgery. The pain is usually managed with prescribed medication and improves within a few days. -
Swelling or Bruising:
Swelling around the surgical site is typical and should resolve within a few days to a week. Bruising around the incision area is also common and will fade as healing progresses. -
Vaginal Spotting or Bleeding:
Light bleeding or spotting may occur as the body heals. This is generally not a cause for concern unless the bleeding becomes excessive or continues for a prolonged period. -
Fatigue:
Post-surgery fatigue is common and is typically a result of the body recovering from the procedure. Adequate rest is essential during this period.
Signs of Success Post-Surgery
-
Return of Menstrual Cycle:
In women, a regular menstrual cycle after surgery indicates that the fallopian tubes may be open and functioning. This is an encouraging sign for fertility. -
Pregnancy:
The ultimate sign of success for the procedure is pregnancy. However, it may take several months for a woman to conceive following tubal reversal. Men undergoing vasectomy reversal will typically need to have a sperm analysis done to confirm the presence of viable sperm post-surgery.
Signs of Complications
-
Severe Pain:
Persistent, sharp pain or discomfort that doesn’t subside after a few days may be a sign of infection or other complications. Immediate consultation with a doctor is recommended. -
Fever:
A fever post-surgery can indicate an infection, which requires prompt medical attention. -
Excessive Bleeding:
Excessive bleeding from the incision sites or abnormal vaginal bleeding should be evaluated by a healthcare provider to rule out complications.
Before deciding on a sterilization reversal, several diagnostic steps are involved. These steps ensure that both the individual’s health and fertility prospects are evaluated and understood.
Consultation and Evaluation
-
Medical History:
A thorough review of the patient’s medical and fertility history is essential. This includes understanding the original sterilization procedure, any complications experienced, and other health issues that may impact fertility. -
Physical Examination:
A pelvic exam is necessary to assess the condition of the reproductive organs. This helps identify any potential obstacles to the reversal procedure, such as scarring or fibroids. -
Sperm Analysis (For Men):
A sperm analysis is typically done before a vasectomy reversal to assess sperm count, motility, and quality. The presence of viable sperm is necessary for the reversal procedure to be effective.
Pre-Surgery Imaging Tests
-
Hysterosalpingogram (HSG):
An HSG is commonly used for women undergoing tubal reversal. This X-ray procedure evaluates the condition of the fallopian tubes and helps determine whether the tubes are blocked or open. This is a crucial test in deciding whether reversal is feasible. -
Ultrasound:
A pelvic ultrasound may be conducted to check for uterine and ovarian abnormalities. In women, the ultrasound can also help in assessing the quality of the ovarian reserve.
Eligibility Criteria
To be eligible for reversal of sterilization, certain conditions must be met:
-
The person should have no medical contraindications to surgery.
-
The individual’s fertility history should indicate that conception is likely with proper treatment.
-
The individual must be fully informed about the permanent nature of the procedure and the risks involved.
-
A thorough assessment of the reproductive organs should be completed to determine the condition of the fallopian tubes or vas deferens.
There are two primary types of reversal surgery: tubal ligation reversal for women and vasectomy reversal for men. Both procedures require specialized surgical techniques to restore fertility.
Tubal Ligation Reversal
-
Laparoscopic Tubal Reversal:
This is the most commonly used technique and is minimally invasive. Small incisions are made in the abdomen, and a laparoscope (a thin tube with a camera) is used to guide the surgeon in reconnecting the fallopian tubes. This technique has the benefit of quicker recovery times and smaller scars. -
Open Tubal Reversal Surgery:
This method requires a larger incision and is usually done when laparoscopic techniques are not feasible. This option is often considered when there is significant damage or scarring to the fallopian tubes, requiring a more extensive approach.
Vasectomy Reversal
-
Vasovasostomy:
The most common vasectomy reversal technique, vasovasostomy involves reconnecting the vas deferens by removing any blockages and stitching the ends of the tube back together. -
Vasoepididymostomy:
If the vas deferens is damaged or blocked, this more complex procedure may be performed. The surgeon connects the vas deferens directly to the epididymis (the tube that stores sperm), bypassing the blockage.
Assisted Reproductive Technology
In cases where surgical reversal does not lead to successful pregnancy, assisted reproductive technologies (ART), such as In Vitro Fertilization (IVF), may be considered. IVF involves fertilizing the eggs outside the body and implanting the embryos in the uterus.
After undergoing a reversal of sterilization, following proper preventive measures and post-surgery management is crucial to ensure successful recovery and increase the chances of pregnancy.
Pre-Surgery Management
-
Health Optimization:
Individuals should aim to be in optimal health before undergoing reversal. This includes managing chronic conditions, achieving a healthy weight, and avoiding smoking and alcohol, all of which can affect fertility and surgery outcomes. -
Fertility Assessment:
Both partners may undergo fertility testing to evaluate the chances of conception post-reversal.
Post-Surgery Management
-
Rest and Recovery:
Adequate rest and avoiding strenuous activity are important in the weeks following surgery. Following the surgeon’s post-operative instructions is essential to prevent complications and promote healing. -
Follow-Up Appointments:
After surgery, follow-up visits are critical to ensure the healing process is proceeding as expected and to check for any signs of complications.
Emotional Support
Many individuals may experience mixed emotions after reversal surgery, especially if pregnancy does not occur immediately. Emotional support, whether through counseling or support groups, can help individuals cope with the psychological aspects of the reversal process.
While the reversal of sterilization can be an effective way to restore fertility, it is not without risks. Some of the potential complications include:
-
Infection: As with any surgery, there is a risk of infection. Post-operative care is crucial to avoid this complication.
-
Damage to Reproductive Organs: In rare cases, there may be damage to surrounding organs or tissues during surgery, which can affect fertility.
-
Scar Tissue: Scar tissue that forms after the surgery may reduce the chances of pregnancy.
-
Failed Reversal: Even with a successful procedure, pregnancy may not occur if there are other underlying fertility issues.
-
Ectopic Pregnancy: Women who conceive after reversal surgery have an increased risk of ectopic pregnancy, where the fertilized egg implants outside the uterus.
After the procedure, many individuals and couples experience a sense of relief, but it is essential to be prepared for what comes next, including emotional and physical adjustments.
Physical Life After Reversal
-
Return to Fertility: While the surgery can restore fertility, it may take several months to over a year for some women to conceive, depending on various factors like age, the quality of the fallopian tubes, and overall reproductive health.
-
Post-Operative Care: After the surgery, follow-up visits will be necessary to monitor the success of the reversal and to ensure the healing process is progressing smoothly.
Emotional and Psychological Considerations
-
Regret or Disappointment: Some women or men may experience disappointment if they do not achieve pregnancy after the reversal, and emotional support may be required.
-
Relationship Dynamics: For couples, undergoing sterilization reversal can sometimes bring up issues of trust, expectations, and future planning. Couples counseling might help in managing these emotions.
1. What is Sterilization Reversal?
Sterilization reversal is a surgical procedure aimed at reversing a previous sterilization (such as tubal ligation or vasectomy) to restore fertility. The surgery involves reconnecting the fallopian tubes in women or the vas deferens in men, allowing sperm to reach the egg for potential conception. This procedure is an option for individuals who wish to regain their ability to conceive after previously choosing permanent contraception.
2. Who is a good candidate for Sterilization Reversal?
Good candidates for sterilization reversal are individuals who have had a sterilization procedure (tubal ligation or vasectomy) but now desire to have children. Women in good overall health, without significant pelvic damage or scarring, and men without significant damage to the vas deferens may be suitable candidates. The decision depends on factors such as age, the length of time since sterilization, and overall reproductive health.
3. How is the Sterilization Reversal surgery performed?
In women, the procedure typically involves making small incisions in the abdomen to access the fallopian tubes. The blocked or severed sections of the tubes are then reconnected. In men, a vasectomy reversal involves making an incision in the scrotum to reconnect the vas deferens. The surgery is generally performed under general anesthesia, and patients usually go home the same day or after a short hospital stay.
4. What are the success rates of Sterilization Reversal?
Success rates for sterilization reversal depend on several factors, including the type of sterilization procedure performed, the length of time since the procedure, and the patient's age. For women, success rates range from 40% to 80%, with younger women generally experiencing higher success rates. For men, vasectomy reversals have a success rate of about 50% to 70%, depending on how much time has passed since the vasectomy.
5. How long does it take to recover from Sterilization Reversal surgery?
Recovery from sterilization reversal surgery varies from person to person, but most women can return to normal activities within 1 to 2 weeks, while men may need about 1 to 2 weeks to recover from a vasectomy reversal. During the first few days, patients may experience mild discomfort, swelling, or bruising, but these symptoms typically subside with proper care and rest.
6. Is the Sterilization Reversal surgery painful?
While the surgery is performed under general anesthesia, some discomfort may be experienced during the recovery period. For women, there may be abdominal pain, while men might experience scrotal swelling or bruising. Pain management options, such as prescribed medications, are typically provided to help manage any discomfort after the procedure.
7. Can I expect to get pregnant immediately after Sterilization Reversal?
Pregnancy is not guaranteed immediately after sterilization reversal. While the surgery restores the possibility of natural conception, it may take some time to conceive. The success of conception depends on factors such as the condition of the reproductive organs, the quality of sperm, and the timing of ovulation. It’s recommended to try for pregnancy for at least 12 months before seeking further fertility treatments if conception does not occur naturally.
8. Are there any risks or complications associated with Sterilization Reversal?
Like any surgery, sterilization reversal carries risks, such as infection, bleeding, damage to surrounding organs, or scarring of the fallopian tubes or vas deferens. There may also be a risk of ectopic pregnancy if the fallopian tubes do not function correctly after the surgery. It is important to have a thorough consultation with your surgeon to understand the risks and possible complications.
9. Will Sterilization Reversal affect my sexual function?
Sterilization reversal surgery typically does not affect sexual function. The surgery is aimed at restoring fertility, not altering sexual anatomy. However, some patients may experience temporary changes in sexual function due to recovery-related discomfort or emotional stress associated with fertility issues. It is important to discuss any concerns with your doctor before and after the procedure.
10. Are there alternatives to Sterilization Reversal for restoring fertility?
If sterilization reversal is not an option or is unsuccessful, there are other fertility treatments available, such as in vitro fertilization (IVF) or the use of donor sperm or eggs. IVF may be an option for women who have had tubal ligation but still have healthy ovaries, while men who have had a vasectomy may consider sperm retrieval and IVF for conception. Your doctor will help guide you through the most appropriate options based on your unique circumstances.
The other Gynecology Procedures are:
Few Major Hospitals for Reversal of Sterilization are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



