A hysterectomy is a major surgical procedure in which the uterus is removed. In some cases, other organs such as the cervix, ovaries, and fallopian tubes may also be removed. The procedure is most commonly performed to treat a variety of conditions affecting the uterus, such as fibroids, cancer, chronic pelvic pain, endometriosis, and abnormal bleeding.
Although a hysterectomy is a highly effective treatment for these conditions, it is also a life-altering procedure with long-term effects on a woman's health, fertility, and overall well-being. Women undergoing a hysterectomy often experience changes in their hormonal balance, fertility status, and physical health. For some, the decision to undergo a hysterectomy is life-saving, while for others, it may be part of an effort to improve quality of life by treating persistent, painful, or distressing symptoms.
A hysterectomy can be performed in a variety of ways, depending on the medical condition being treated, the patient's health, and whether the uterus needs to be removed entirely. This detailed guide will help you understand the reasons for the procedure, the risks and benefits, and how to manage the recovery process.
The decision to undergo a hysterectomy is usually based on the severity of a woman's condition and how it affects her health. Many conditions can contribute to the need for this surgery, and it is often considered when other treatment options have not worked.
Common Causes for Hysterectomy:
-
Uterine Cancer:
-
Endometrial cancer, cervical cancer, and ovarian cancer are some of the leading causes of hysterectomy. For patients with uterine cancer, the procedure is often necessary to remove the affected organ and prevent the spread of cancer to other parts of the body.
-
-
Fibroids:
-
Uterine fibroids are non-cancerous growths that develop in the uterine muscle. In some women, fibroids can cause heavy bleeding, pelvic pain, frequent urination, and other symptoms. If fibroids become large or cause significant discomfort, a hysterectomy may be recommended.
-
-
Endometriosis:
-
Endometriosis is a painful condition where tissue similar to the uterine lining grows outside the uterus. This can cause chronic pelvic pain, infertility, and other symptoms. If conservative treatments fail, a hysterectomy may be considered to remove the affected tissue and relieve symptoms.
-
-
Chronic Pelvic Pain:
-
Women who suffer from chronic pelvic pain not responsive to other treatments may undergo a hysterectomy to address the underlying cause, such as adenomyosis (a condition where the uterine lining grows into the uterine muscle), fibroids, or endometriosis.
-
-
Abnormal Uterine Bleeding:
-
Heavy or irregular menstrual bleeding is one of the most common reasons for hysterectomy. Conditions such as dysfunctional uterine bleeding, adenomyosis, or endometrial hyperplasia (thickening of the uterine lining) may require this procedure to manage abnormal bleeding.
-
-
Prolapsed Uterus:
-
A prolapsed uterus occurs when the uterus drops into the vaginal canal due to weakened pelvic floor muscles. This condition can cause discomfort and urinary or bowel problems. A hysterectomy may be recommended in severe cases where other treatments, such as pelvic floor exercises or pessaries, have been ineffective.
-
-
Infections and Inflammatory Diseases:
-
Chronic infections, such as pelvic inflammatory disease (PID), or recurrent uterine infections that cause irreversible damage to the uterus can result in the need for a hysterectomy to prevent further complications.
-
-
Molar Pregnancy:
-
A molar pregnancy occurs when an abnormal growth develops inside the uterus, often resulting in a miscarriage. In rare cases, a hysterectomy is performed to remove the molar tissue and prevent further complications.
-
Risk Factors for Requiring a Hysterectomy:
-
Age:
-
Women over 40 years of age, particularly those in perimenopause and menopause, are at higher risk of requiring a hysterectomy due to the increased incidence of conditions such as fibroids, endometrial cancer, or uterine prolapse.
-
-
Chronic Gynecological Conditions:
-
Women with a history of chronic pelvic conditions, such as endometriosis, fibroids, or adenomyosis, may be at higher risk of requiring a hysterectomy if these conditions become severe or unmanageable with non-surgical treatments.
-
-
Multiple Pregnancies or Childbirth:
-
Women who have had multiple pregnancies, especially those involving difficult deliveries, are at higher risk for conditions such as uterine prolapse or trauma that may require a hysterectomy.
-
-
Obesity:
-
Obesity has been linked to an increased risk of developing fibroids, endometrial cancer, and other conditions that may require a hysterectomy.
-
-
Family History:
-
A family history of gynecological cancers (such as endometrial or ovarian cancer) or conditions like fibroids and endometriosis may increase the likelihood of needing a hysterectomy.
-
The need for a hysterectomy typically arises from persistent or severe symptoms related to gynecological conditions. These symptoms can range from physical discomfort to more severe health issues affecting the quality of life.
Symptoms Indicating the Need for a Hysterectomy:
-
Heavy Menstrual Bleeding:
-
One of the most common symptoms that may lead to a hysterectomy is heavy or irregular bleeding. This can occur due to conditions such as fibroids, endometrial hyperplasia, or adenomyosis.
-
-
Pelvic Pain:
-
Chronic pelvic pain from conditions like endometriosis or fibroids can be debilitating. If other treatments fail to alleviate the pain, a hysterectomy may be recommended.
-
-
Abnormal Vaginal Discharge:
-
Women experiencing unusual vaginal discharge that may be a sign of an infection or abnormal growth (such as fibroids or cancer) may require further investigation and potentially a hysterectomy.
-
-
Abnormal Uterine Growths:
-
Growths like fibroids or polyps may cause abnormal symptoms, including bloating, pelvic pressure, or urinary problems. A hysterectomy may be needed to remove these growths and improve symptoms.
-
-
Infertility or Miscarriage:
-
In women with conditions like endometriosis or fibroids, a hysterectomy may be considered if these conditions lead to infertility or recurrent miscarriage that cannot be addressed through less invasive treatments.
-
-
Prolapsed Uterus:
-
Women with a prolapsed uterus may experience symptoms such as a bulging sensation in the vagina, pelvic pressure, urinary or bowel difficulties, and discomfort during sexual intercourse. A hysterectomy may be recommended if conservative treatments do not provide relief.
-
Before performing a hysterectomy, doctors typically carry out a series of diagnostic tests to understand the underlying condition and determine whether surgery is necessary.
Diagnostic Methods:
-
Pelvic Examination:
-
The doctor will perform a pelvic exam to evaluate the size and shape of the uterus, check for abnormal growths, and assess the overall health of the pelvic organs.
-
-
Ultrasound:
-
A transvaginal ultrasound is commonly used to visualize the uterus and any abnormal growths, such as fibroids or polyps. It can also be used to evaluate the endometrial lining for signs of cancer or abnormal tissue growth.
-
-
Hysteroscopy:
-
A hysteroscope (a thin tube with a camera) may be used to examine the inside of the uterus. This allows the doctor to assess conditions like endometrial hyperplasia, fibroids, and polyps. A biopsy may also be performed during this procedure if cancer is suspected.
-
-
Biopsy:
-
A biopsy of the uterine lining may be performed to check for signs of endometrial cancer or precancerous cells. A sample of the uterine tissue is taken for examination.
-
-
MRI or CT Scan:
-
In complex cases, MRI or CT scans may be used to get detailed images of the uterus and surrounding tissues. These imaging techniques help assess large fibroids, endometriosis, or any other abnormal growths.
-
A hysterectomy is typically performed when other treatment options have been exhausted or are not effective. It is important to consider all treatment options before choosing surgery.
Types of Hysterectomy:
-
Total Hysterectomy:
-
The entire uterus and cervix are removed. This is the most common form of hysterectomy.
-
-
Subtotal or Partial Hysterectomy:
-
Only the uterus is removed, while the cervix is left intact. This procedure is sometimes used when cervical issues are not a concern.
-
-
Radical Hysterectomy:
-
A radical hysterectomy involves the removal of the uterus, cervix, part of the vagina, and surrounding tissues, including the lymph nodes. This type of hysterectomy is often performed for cervical cancer or advanced uterine cancer.
-
-
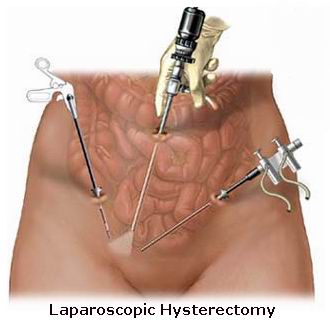
Laparoscopic (Minimally Invasive) Hysterectomy:
-
A laparoscopic hysterectomy uses small incisions and a camera to guide the surgeon in removing the uterus. This minimally invasive technique offers faster recovery times and less postoperative pain.
-
-
Vaginal Hysterectomy:
-
A vaginal hysterectomy involves the removal of the uterus through the vaginal canal. It is often performed for uterine prolapse or when a minimally invasive approach is preferred.
-
Non-Surgical Treatment Options:
-
Medications:
-
For conditions like fibroids or endometriosis, medications such as hormonal therapies, birth control pills, or GnRH agonists can help reduce symptoms and possibly avoid the need for surgery.
-
-
Uterine Artery Embolization:
-
This procedure is used to treat fibroids by blocking the blood supply to the fibroids, causing them to shrink and die.
-
-
Endometrial Ablation:
-
Endometrial ablation is a procedure that destroys the uterine lining to treat heavy bleeding. It is typically recommended for women who do not wish to have children in the future.
-
As with any major surgery, there are risks and potential complications associated with a hysterectomy. These complications can vary based on the type of hysterectomy, the reason for the procedure, and the patient’s overall health.
Potential Complications:
-
Infection:
-
Infection is a risk after any surgery. Women who undergo hysterectomy are at risk of developing infections in the incision sites or within the pelvic cavity. Antibiotics are often prescribed to prevent infections.
-
-
Heavy Bleeding:
-
Though bleeding is normal during and after the surgery, some women may experience excessive bleeding. In rare cases, a blood transfusion may be necessary.
-
-
Injury to Surrounding Organs:
-
During the surgery, there is a risk of damage to nearby organs, such as the bladder, urethra, or bowel. Though rare, injuries may require further surgical repair.
-
-
Early Menopause:
-
If the ovaries are removed along with the uterus, early menopause can occur, leading to symptoms like hot flashes, night sweats, and mood swings. Hormone replacement therapy (HRT) may be recommended to manage these symptoms.
-
-
Pelvic Floor Dysfunction:
-
Some women experience pelvic floor dysfunction or weakened pelvic muscles following a hysterectomy. This can lead to issues with bladder control or vaginal prolapse.
-
-
Blood Clots:
-
As with any surgery, there is a risk of blood clots forming in the legs or lungs. Preventative measures, such as walking soon after surgery and wearing compression stockings, can reduce this risk.
-
Recovering from a hysterectomy involves both physical and emotional adjustments. While the surgery provides relief from certain medical conditions, it may come with challenges, particularly for women who are dealing with changes related to menopause or the loss of fertility.
Post-Surgery Recovery:
-
Physical Recovery:
-
After a hysterectomy, it is important to rest and take care of the body. Women are generally advised to avoid heavy lifting, strenuous activity, and sexual intercourse for at least 6 weeks to allow proper healing.
-
-
Emotional Recovery:
-
The emotional impact of having a hysterectomy, particularly for women who were hoping to have children, should not be underestimated. Counseling and support groups can help women process the emotional changes that follow the procedure.
-
-
Hormonal Therapy:
-
For women who have had their ovaries removed, hormone replacement therapy (HRT) may be recommended to help manage menopausal symptoms and protect against bone loss.
-
-
Long-Term Care:
-
Regular check-ups and follow-up appointments with a healthcare provider are essential to monitor the healing process and manage any long-term effects, such as pelvic floor health or bone density.
-
1. What is a hysterectomy?
A hysterectomy is a surgical procedure in which a woman’s uterus is removed. This procedure may also involve the removal of other reproductive organs, such as the ovaries, fallopian tubes, or cervix, depending on the reason for the surgery. It is typically performed to treat conditions such as uterine fibroids, endometriosis, cancer, or chronic pelvic pain.
2. Why would I need a hysterectomy?
A hysterectomy may be recommended for several reasons, including:
-
Uterine fibroids: Noncancerous growths in the uterus that cause heavy bleeding or pain.
-
Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus.
-
Cancer: Uterine, cervical, or ovarian cancer may necessitate removal of the uterus.
-
Chronic pelvic pain: Unresolved pain that doesn't respond to other treatments.
-
Abnormal bleeding: Heavy, irregular, or prolonged menstrual bleeding.
-
Prolapsed uterus: When the uterus descends into the vaginal canal due to weakened pelvic muscles.
3. What are the different types of hysterectomy?
There are several types of hysterectomy, depending on the extent of the surgery:
-
Total hysterectomy: Removal of the uterus and cervix.
-
Subtotal (or partial) hysterectomy: Removal of the uterus, but leaving the cervix intact.
-
Radical hysterectomy: Removal of the uterus, cervix, parts of the vagina, and surrounding tissues. This is usually performed for cancer treatment.
-
Laparoscopic (minimally invasive) hysterectomy: Performed through small incisions with the help of a camera, offering faster recovery.
-
Abdominal hysterectomy: Involves a larger incision in the abdomen to remove the uterus.
4. How is a hysterectomy performed?
A hysterectomy can be performed in several ways, depending on the type of surgery and the patient’s condition. The procedure may be done through:
-
Abdominal incision: A large incision made in the abdomen to remove the uterus.
-
Vaginal incision: The uterus is removed through the vagina.
-
Laparoscopic surgery: Minimally invasive surgery with small incisions using a camera and specialized instruments to remove the uterus.
The choice of method depends on factors like the size of the uterus, the reason for the surgery, and the patient’s overall health.
5. Is a hysterectomy painful?
A hysterectomy is performed under anesthesia, so you will not feel pain during the procedure. After the surgery, you may experience some discomfort, cramping, or soreness in the abdominal or pelvic area. Pain can typically be managed with prescribed medication, and most women experience significant relief after a few days. The recovery period will vary depending on the type of surgery performed.
6. What is the recovery time after a hysterectomy?
Recovery time depends on the type of hysterectomy:
-
Laparoscopic hysterectomy: Most women can return to normal activities within 2 to 4 weeks.
-
Abdominal hysterectomy: Recovery may take 6 to 8 weeks, as the procedure involves a larger incision.
During recovery, it’s important to avoid heavy lifting, strenuous activities, and sexual intercourse until your doctor gives the go-ahead. Follow-up appointments will be scheduled to monitor your progress.
7. Will I experience any side effects after a hysterectomy?
Some side effects after a hysterectomy may include:
-
Menopause: If the ovaries are removed (oophorectomy), you will experience menopause immediately after the surgery.
-
Hot flashes, mood changes, and vaginal dryness: These are common menopausal symptoms.
-
Pelvic floor changes: Some women may experience urinary or bowel changes, or pelvic floor weakness.
-
Hormonal imbalances: If the ovaries are removed, hormone replacement therapy (HRT) may be recommended to manage symptoms.
8. Can I still get pregnant after a hysterectomy?
No, after a hysterectomy, you will no longer be able to get pregnant. This is because the uterus, where pregnancy occurs, is removed. If only the uterus is removed and the ovaries and fallopian tubes are preserved, your hormones may still function normally, but you will not be able to carry a pregnancy. For women who are not yet sure about having children, it is important to discuss the possibility of preserving eggs or embryos before undergoing the surgery.
9. Are there any risks associated with a hysterectomy?
As with any surgery, there are risks associated with a hysterectomy, including:
-
Infection: The risk of infection in the surgical area or pelvic organs.
-
Bleeding: Excessive bleeding during or after the surgery.
-
Damage to surrounding organs: In rare cases, nearby organs such as the bladder, bowel, or ureters may be injured.
-
Blood clots: The risk of developing blood clots in the legs or lungs, especially during the recovery phase.
-
Urinary or bowel problems: Some women may experience difficulty with urination or bowel movements after surgery.
10. What is the long-term outlook after a hysterectomy?
After recovery, most women find that their symptoms are significantly improved or completely resolved. A hysterectomy can provide relief from chronic pelvic pain, heavy bleeding, or other underlying conditions. If the ovaries are removed, you will enter menopause, which may require hormone replacement therapy to manage symptoms. Overall, a hysterectomy improves the quality of life for many women by alleviating painful or debilitating symptoms, though it is important to follow up with your doctor for continued care.
The other Gynecology Procedures are:
Few Major Hospitals for Hysterectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



