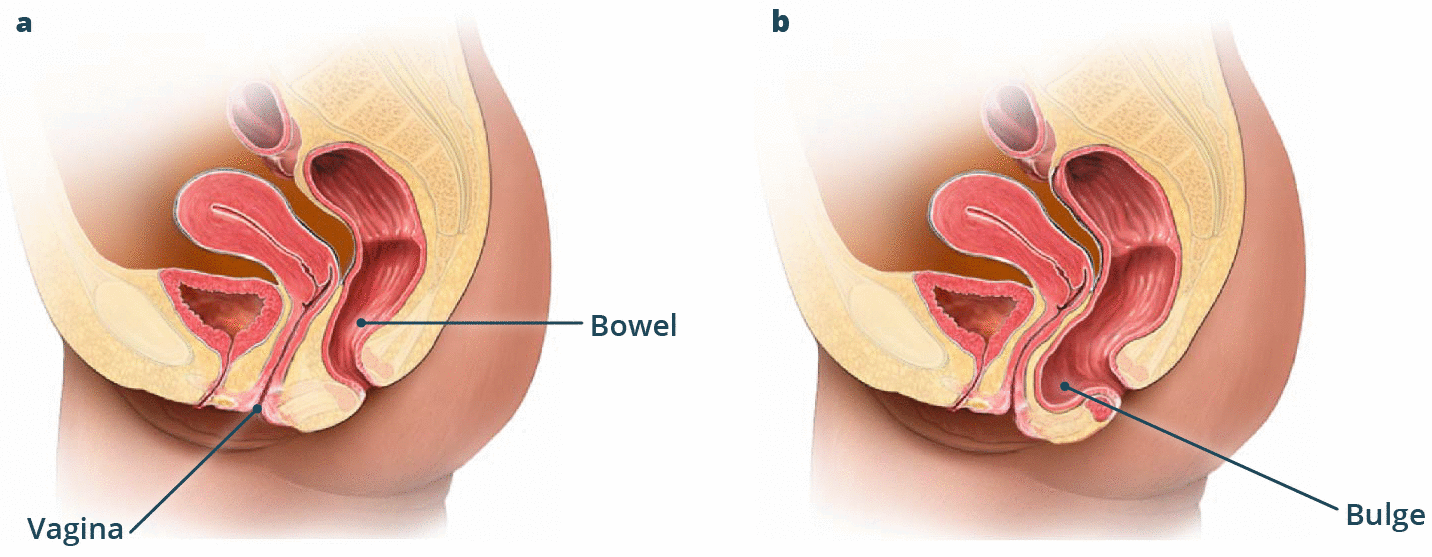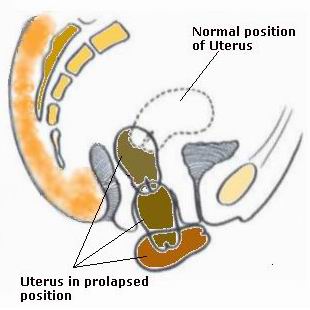
Posterior repair for prolapse operation is a surgical procedure designed to treat posterior vaginal wall prolapse, a condition that affects the pelvic floor in women. This condition occurs when the muscles and tissues of the posterior vaginal wall weaken or stretch, causing the vaginal wall to bulge or prolapse. This can lead to symptoms such as pelvic pressure, urinary issues, and difficulties with bowel movements.
The posterior repair surgery aims to restore the normal anatomy of the pelvic floor by repairing the weakened tissues and muscles, thus providing relief from the symptoms associated with prolapse. The procedure is commonly performed when conservative treatments, such as pelvic floor exercises or the use of a pessary (a device placed in the vagina to support the pelvic organs), have not been successful.
Posterior repair is usually carried out under general anesthesia and involves a small incision at the back of the vaginal wall. The surgeon tightens and supports the weakened muscles and tissues, improving the pelvic structure and restoring proper function.
This surgery has been proven to be effective in improving a woman’s quality of life by resolving the discomfort caused by prolapse and helping to prevent further complications, such as incontinence or rectal problems.
The causes and risk factors for posterior vaginal wall prolapse (which leads to posterior repair surgery) are largely related to factors that place pressure on the pelvic floor or weaken the supportive tissues. Some of the primary causes and risk factors include:
a. Childbirth
The most significant risk factor for posterior vaginal wall prolapse is childbirth, especially vaginal deliveries. The process of labor and delivery, particularly with a large baby, forceful delivery, or prolonged labor, can stretch and weaken the pelvic floor muscles. Multiple pregnancies or difficult childbirth also increase the risk of developing prolapse.
b. Aging
As women age, especially after menopause, the pelvic floor muscles naturally weaken due to the loss of estrogen, a hormone that helps maintain the elasticity of the pelvic tissues. Post-menopausal women are at higher risk for developing prolapse due to hormonal changes and the weakening of supportive tissues.
c. Chronic Straining
Chronic conditions that cause straining, such as constipation, chronic cough, or obesity, increase intra-abdominal pressure. This pressure weakens the pelvic floor muscles over time, contributing to prolapse. Women who experience frequent straining may be more likely to develop prolapse.
d. Genetic Factors
Some women may have a genetic predisposition to pelvic organ prolapse. A family history of prolapse may increase a woman’s likelihood of experiencing similar issues.
e. Pelvic Surgery
Previous pelvic surgeries, such as hysterectomy (removal of the uterus), can also increase the risk of developing prolapse, as the surgery may weaken the pelvic floor or cause damage to the supporting tissues.
f. Increased Age and Gender
Prolapse is most commonly found in older women, particularly after the age of 50. Menopause can accelerate pelvic floor weakening, making the condition more prevalent in older women.
Posterior vaginal wall prolapse, which leads to the need for posterior repair, can manifest in various ways. The severity of symptoms can range from mild discomfort to more severe issues that affect daily life. Some common symptoms and signs of posterior prolapse include:
a. Pelvic Pressure and Heaviness
Women with posterior prolapse often experience a feeling of pressure or fullness in the pelvic region. This can feel like the pelvic organs are “weighing down” or “falling out,” which can cause discomfort, especially when standing or engaging in physical activity.
b. Vaginal Bulge
A noticeable bulge or lump in the vaginal wall, especially when straining or during physical activity, is a common symptom. The bulge may become more pronounced when a woman is sitting, standing, or lifting heavy objects.
c. Bowel Dysfunction
Prolapse can affect the rectum and cause difficulty with bowel movements, such as constipation, incomplete emptying, or the sensation that the rectum is not fully empty after a bowel movement. Some women may also experience fecal incontinence or leakage.
d. Urinary Problems
Although posterior prolapse primarily affects the rectum, it may also lead to urinary issues such as urinary incontinence or frequency (the need to urinate frequently). The bladder may become displaced due to pressure from the prolapse, causing discomfort or issues with urination.
e. Low Back Pain
Some women with posterior prolapse experience low back pain due to the strain on the pelvic muscles and ligaments. The discomfort may worsen with prolonged standing, walking, or physical exertion.
f. Pain During Sexual Activity
A prolapsed vaginal wall can cause pain or discomfort during sexual intercourse. The pressure from the prolapse may make penetration difficult or uncomfortable.
Accurate diagnosis is essential for determining the need for posterior repair surgery. A comprehensive evaluation, including a pelvic exam and medical history, will be conducted to assess the extent of the prolapse and confirm the diagnosis. The following diagnostic steps may be involved:
a. Medical History Review
A detailed medical history will be taken, including information about childbirth, any previous surgeries (especially pelvic or abdominal), and symptoms such as urinary or bowel dysfunction. This helps the doctor understand the likely causes of prolapse.
b. Pelvic Examination
During the pelvic exam, the doctor will assess the vaginal wall, rectum, and other pelvic organs. The doctor will ask the patient to bear down (similar to straining during a bowel movement) to see if the posterior vaginal wall bulges and assess the degree of prolapse. The doctor may also assess the strength of the pelvic floor muscles.
c. Imaging Tests
In some cases, imaging tests such as an ultrasound or MRI may be used to assess the position and condition of the pelvic organs. These tests help the doctor determine the severity of the prolapse and plan the surgery accordingly.
d. Urodynamics and Defecography
For women experiencing urinary or bowel issues, additional tests like urodynamics (to assess bladder function) or defecography (to evaluate the rectum and anus) may be performed to rule out other conditions.
When conservative treatments (such as pelvic floor exercises or pessaries) fail, surgery is often recommended. Posterior repair surgery involves repairing the vaginal wall and strengthening the pelvic floor to restore normal function. The options available for posterior prolapse surgery include:
a. Traditional Posterior Vaginal Repair
This is the most common surgical approach to treat posterior prolapse. The surgeon makes an incision at the back of the vaginal wall and removes or repositions any excess tissue. The vaginal wall is then repaired, and the pelvic organs are supported by tightening the tissues and muscles.
b. Mesh or Graft Repairs
In some cases, synthetic mesh or biologic grafts may be used to reinforce the posterior vaginal wall. This is typically done for more severe prolapse cases or when previous repairs have failed.
c. Laparoscopic or Robotic-Assisted Surgery
For some patients, minimally invasive approaches such as laparoscopy or robotic-assisted surgery may be used to perform the posterior repair. These techniques involve smaller incisions and the use of cameras and robotic tools for greater precision, leading to shorter recovery times and less scarring.
d. Colpocleisis (Vaginal Closure)
In rare cases, particularly for elderly women or those who do not plan to engage in sexual activity, colpocleisis (a procedure in which the vaginal canal is closed off) may be an option. This is a more drastic approach to treating prolapse.
While posterior prolapse may not always be preventable, there are certain steps women can take to manage the condition and reduce the risk of recurrence after surgery:
a. Pelvic Floor Exercises
Regular pelvic floor exercises (also known as Kegel exercises) can help strengthen the muscles and tissues supporting the pelvic organs. These exercises are particularly beneficial after surgery to maintain pelvic floor health.
b. Weight Management
Maintaining a healthy weight reduces the pressure on the pelvic floor and can lower the risk of prolapse. Obesity is a significant risk factor for pelvic organ prolapse, so weight management should be a priority.
c. Avoiding Chronic Straining
Women who suffer from chronic constipation, coughing, or other conditions that require excessive straining should take steps to manage these issues. A high-fiber diet, staying hydrated, and using appropriate treatments for respiratory issues can help reduce the strain on the pelvic floor.
While posterior repair surgery is generally safe and effective, there are potential complications that patients should be aware of:
a. Infection
Like any surgery, infection at the incision site or in the pelvic region is a possibility. Proper wound care and following the doctor’s post-operative instructions can minimize this risk.
b. Bleeding
Some bleeding is normal after surgery, but excessive bleeding may occur in rare cases. If bleeding is persistent or heavy, medical attention should be sought immediately.
c. Recurrence of Prolapse
In some cases, prolapse may recur after surgery. Factors such as age, obesity, and the degree of the prolapse may influence the likelihood of recurrence.
d. Injury to Nearby Organs
Though rare, injury to surrounding organs, such as the bladder or rectum, can occur during the surgery. The risk of injury is minimized when the surgery is performed by an experienced surgeon.
After posterior repair surgery, patients can expect to experience significant improvements in their symptoms and quality of life. However, there are some long-term considerations:
a. Post-Surgical Recovery
The recovery time for posterior repair surgery varies, but most women can return to normal activities within 4 to 6 weeks. During the first few weeks, patients should avoid heavy lifting, sexual activity, and strenuous physical activities.
b. Long-Term Health Monitoring
Ongoing care and regular follow-ups with the healthcare provider are important to monitor the success of the surgery and ensure no complications arise. Pelvic floor exercises and healthy lifestyle choices should be continued to maintain pelvic health.
1. What is Posterior Repair Surgery for Prolapse?
Posterior repair surgery is a procedure designed to treat posterior vaginal prolapse (rectocele), a condition where the rectum bulges into the vaginal wall. This surgery involves repairing the weakened vaginal wall between the rectum and the vagina to restore normal pelvic function and eliminate symptoms such as pelvic pressure, vaginal bulging, and difficulty with bowel movements.
2. Who is a good candidate for Posterior Repair Surgery?
Candidates for posterior repair surgery are typically women suffering from symptoms of vaginal prolapse, such as a bulging sensation in the vagina, bowel issues like constipation, or pelvic pressure. Women who have not responded to conservative treatments, such as pelvic floor exercises or a pessary, may also be considered for surgery. An evaluation by a pelvic floor specialist is required to determine candidacy.
3. How is Posterior Repair Surgery performed?
Posterior repair is usually performed through the vaginal wall. The surgeon makes small incisions in the vaginal tissue to access the prolapsed rectum. The prolapsed tissue is then repositioned, and the vaginal wall is reinforced to provide support. The procedure can be done under general or regional anesthesia, and it is often minimally invasive, requiring only a short hospital stay.
4. What are the benefits of Posterior Repair Surgery?
The main benefit of posterior repair surgery is the relief of prolapse symptoms, such as pelvic pressure, difficulty with bowel movements, and the sensation of vaginal bulging. The surgery restores normal anatomy to the pelvic floor, improves bowel and urinary function, and can enhance the quality of life by preventing the recurrence of prolapse.
5. Are there risks associated with Posterior Repair Surgery?
Like any surgery, posterior repair carries some risks, including infection, bleeding, injury to surrounding organs (like the bladder or bowel), and anesthesia complications. There is also a small risk of recurrence of prolapse or problems with vaginal scarring. It’s important to discuss these risks with your surgeon before undergoing the procedure.
6. How long does it take to recover after Posterior Repair Surgery?
Recovery from posterior repair surgery typically takes a few weeks. Most patients can resume light activities after 2 to 4 weeks, but they are advised to avoid heavy lifting and strenuous exercise for about 6 weeks. Full recovery can take several months, during which time you may experience some vaginal discomfort, swelling, or bruising.
7. Will I need to stay in the hospital after Posterior Repair Surgery?
In most cases, posterior repair surgery is performed as an outpatient procedure, meaning you can go home the same day. However, if there are complications or if you have additional medical concerns, you may need to stay in the hospital for a short period, usually one or two nights.
8. Can Posterior Repair Surgery be done alongside other procedures?
Yes, posterior repair can often be combined with other pelvic floor surgeries, such as anterior vaginal repair for cystocele (bladder prolapse) or a hysterectomy if necessary. Combining procedures can be more efficient and reduce the need for multiple surgeries, but this will depend on the patient's specific condition and overall health.
9. Will Posterior Repair Surgery affect my sexual function?
Posterior repair surgery generally aims to improve pelvic function and may enhance sexual health by relieving the symptoms of prolapse, such as vaginal bulging. Most women report improved sexual function after recovery, although some may experience temporary vaginal dryness or discomfort. It’s important to communicate with your doctor about any concerns related to sexual function before and after surgery.
10. How effective is Posterior Repair Surgery?
Posterior repair surgery is highly effective in treating posterior prolapse. Studies show that most women experience significant relief from symptoms, with low recurrence rates. However, results vary based on factors like age, the severity of the prolapse, and whether the patient has other pelvic floor issues. It’s essential to follow post-surgery instructions to maximize the chances of a successful outcome.
The other Gynecology Procedures are:
Few Major Hospitals for Posterior Repair - Prolapse Operation are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.