Vaginal and perineal plastic surgery refers to surgical procedures aimed at repairing, reconstructing, or enhancing the appearance and function of the vagina, vulva, and perineum (the area between the vaginal opening and the anus). These surgeries can be performed for a variety of reasons, including medical, functional, aesthetic, or reconstructive needs.
Vaginal plastic surgery includes procedures such as vaginoplasty, which tightens the vaginal walls, and labiaplasty, which reshapes or reduces the size of the labia. Perineal plastic surgery typically involves repairing the perineum, especially after childbirth, when the muscles and tissues may become stretched or torn. In some cases, surgeries such as perineoplasty may be performed to restore the tone and appearance of the perineal area.
Women may seek vaginal and perineal plastic surgery for reasons related to childbirth injuries, aging, congenital conditions, sexual function, or aesthetic preferences. For some, these surgeries are essential for improving quality of life, restoring confidence, and enhancing sexual satisfaction. In other cases, the surgery may be performed for medical reasons, such as to treat pelvic organ prolapse or to correct perineal tears that occurred during childbirth.
This article will explore the causes, symptoms, diagnosis, treatment options, prevention, complications, and management of vaginal and perineal plastic surgery. It will also provide insights into living with the condition following surgery.
Vaginal and perineal plastic surgery can be sought for a variety of medical, functional, and aesthetic reasons. Below are the primary causes and risk factors that may lead to the need for these surgeries.
Causes for Vaginal & Perineal Plastic Surgery:
-
Childbirth-Related Trauma:
The most common cause of vaginal and perineal surgery is trauma that occurs during childbirth. Perineal tears are common during vaginal delivery, and in severe cases, these tears may involve the anal sphincter or deeper tissues. Episiotomy, a surgical incision made to prevent tearing, can also cause scarring, leading to discomfort or sexual dysfunction.Women who have had multiple vaginal births or traumatic deliveries may experience vaginal laxity, stretching, or prolapse, making surgery necessary to restore functionality.
-
Aging and Vaginal Atrophy:
As women age, especially after menopause, the vaginal tissues may lose elasticity, resulting in vaginal dryness, thinning of the vaginal walls, and reduced elasticity. This can cause discomfort during intercourse, vaginal laxity, and a decrease in sexual satisfaction. Vaginal rejuvenation surgeries like vaginoplasty can restore elasticity and improve sexual function. -
Congenital Anomalies:
Some women are born with vaginal or perineal anatomical abnormalities that may cause functional or aesthetic concerns. Congenital conditions, such as an underdeveloped vaginal opening or asymmetrical labia, can be corrected through plastic surgery to improve both appearance and function. -
Pelvic Organ Prolapse:
Pelvic organ prolapse (POP) occurs when the bladder, uterus, or rectum drops into the vaginal canal due to weakened pelvic floor muscles. This condition may require reconstructive vaginal surgery to restore the vaginal walls and perineum. -
Sexual Health and Satisfaction:
Some women seek vaginal and perineal plastic surgery to improve sexual function and satisfaction. For example, a vaginoplasty may help women who feel that their vaginal tone has been compromised due to childbirth or aging. Labiaplasty may be sought by women who are self-conscious about the appearance of their labia and experience discomfort during physical activities or sex. -
Cosmetic and Aesthetic Concerns:
Increasingly, women are opting for cosmetic genital surgery to improve the appearance of their genital area. Labiaplasty, which reduces the size of the labia minora, and vulvoplasty, which reshapes the vulva, are common procedures for aesthetic enhancement.
Risk Factors for Vaginal & Perineal Plastic Surgery:
-
Multiple Childbirths:
Women who have had multiple vaginal deliveries are at an increased risk of vaginal and perineal trauma, including vaginal laxity, perineal tears, and prolapse, which may require surgical intervention. -
Obesity:
Being overweight can increase the risk of vaginal and perineal issues such as prolapse and weakened pelvic floor muscles. Excess weight puts added pressure on the pelvic organs, contributing to the need for surgery. -
Age:
As women age, the elasticity and tone of vaginal and perineal tissues decline. Postmenopausal women, in particular, are more likely to experience vaginal atrophy and perineal issues that may necessitate plastic surgery. -
Sexual Activity:
Certain sexual activities, particularly those that involve rough or traumatic movements, may lead to perineal or vaginal injury, contributing to the need for reconstructive surgery. -
Genetic Factors:
Women with a family history of vaginal or pelvic floor disorders, such as prolapse or congenital anomalies, may be at a higher risk for requiring vaginal and perineal plastic surgery.
The decision to undergo vaginal and perineal plastic surgery is often prompted by various symptoms that affect a woman’s quality of life. These symptoms may vary depending on the underlying cause of the condition. Common symptoms that indicate the need for surgical intervention include:
1. Vaginal Laxity:
One of the most common symptoms prompting vaginoplasty or labiaplasty is vaginal laxity, which can occur after childbirth or as a result of aging. Vaginal laxity can cause feelings of looseness, reduced sexual satisfaction, and discomfort during sexual intercourse.
2. Pelvic Floor Dysfunction:
Women who experience pelvic organ prolapse (where the uterus, bladder, or rectum drops into the vaginal canal) may experience symptoms such as difficulty urinating, urinary incontinence, constipation, and pain during intercourse. This may lead to the need for reconstructive surgery to restore the vaginal and perineal tissues.
3. Pain and Discomfort During Intercourse:
Dyspareunia, or pain during intercourse, can result from vaginal laxity, perineal scarring from childbirth, or congenital abnormalities. Vaginal and perineal plastic surgery can help alleviate this discomfort by tightening the vaginal walls or repairing the perineum.
4. Labial Enlargement or Asymmetry:
Some women experience enlarged, asymmetrical, or protruding labia that may cause self-consciousness or physical discomfort during activities like exercise or sexual intercourse. Labiaplasty can help reduce labial size and improve both aesthetics and comfort.
5. Urinary Incontinence:
Women with weakened pelvic floor muscles may experience urinary incontinence (involuntary leakage of urine) due to weakened tissues that support the bladder. Surgical intervention may be necessary to restore proper pelvic floor function.
6. Scarring from Childbirth:
Severe perineal tears or episiotomy incisions that do not heal properly can lead to scarring or tightness in the vaginal or perineal area. This may cause discomfort, pain, or sexual dysfunction, leading women to seek surgical intervention.
The diagnosis of conditions that require vaginal and perineal plastic surgery typically involves a thorough medical history and physical examination by a gynecologist or pelvic floor specialist. Here’s an overview of the diagnostic process:
1. Medical History and Symptom Review:
The first step in diagnosis involves discussing the patient’s symptoms, such as vaginal laxity, pelvic organ prolapse, sexual dysfunction, and pain. The doctor will inquire about the patient’s obstetric history (e.g., number of children, type of deliveries) and any previous surgeries.
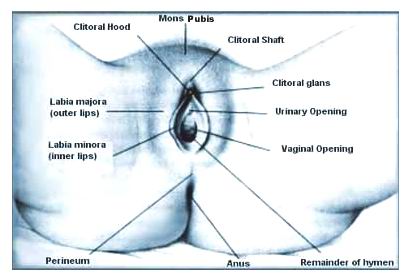
2. Pelvic Examination:
A comprehensive pelvic exam will be conducted to assess the vaginal and perineal areas for signs of damage, laxity, scarring, or prolapse. The doctor will check for the size and shape of the labia and assess the integrity of the vaginal walls and perineum.
3. Imaging Studies:
In some cases, ultrasound or MRI may be used to visualize the pelvic organs and assess any damage to the tissues, especially in cases of pelvic organ prolapse. Imaging may also be used to evaluate the thickness of the vaginal walls or detect any abnormalities.
4. Urodynamic Testing:
If urinary incontinence is present, a urodynamic study may be conducted to assess the function of the bladder and determine whether surgery is required to improve bladder control.
5. Vaginal or Perineal Scoring:
In some cases, a vaginal scoring system or perineal scoring system may be used to assess the degree of vaginal or perineal damage. This is particularly useful in determining the need for reconstructive surgery following childbirth injuries.
Treatment for vaginal and perineal issues may involve surgical procedures aimed at restoring function and improving appearance. The most common surgical treatments include:
1. Vaginal Tightening (Vaginoplasty):
Vaginoplasty is a procedure designed to tighten the vaginal walls by removing excess tissue and repairing the vaginal muscles. This procedure is commonly sought by women experiencing vaginal laxity due to aging or childbirth.
2. Labiaplasty:
Labiaplasty involves reshaping or reducing the size of the labia minora (the inner vaginal lips) or labia majora (the outer lips). This procedure can alleviate discomfort, improve the appearance of the genital area, and enhance sexual satisfaction.
3. Perineoplasty:
Perineoplasty is performed to repair the perineum, particularly after severe perineal tears or episiotomy scars from childbirth. This surgery restores the appearance and function of the perineum and helps reduce discomfort during sexual activity.
4. Pelvic Floor Reconstruction:
In cases of pelvic organ prolapse, pelvic floor reconstruction is performed to lift and support the pelvic organs. This may involve repairing the vaginal walls, repositioning the bladder, uterus, or rectum, and tightening the pelvic floor muscles.
5. Colpocleisis (Vaginal Closure):
Colpocleisis is a procedure that is sometimes used in cases of severe pelvic organ prolapse, especially in older women who are no longer sexually active. It involves partially or completely closing the vagina to prevent prolapse of the pelvic organs.
6. Botox Injections:
In some cases, botulinum toxin (Botox) injections can be used to relax the vaginal muscles and improve vaginal tone. This is a less invasive option for women who experience vaginal tightness or discomfort.
While vaginal and perineal plastic surgeries are effective in treating various conditions, there are preventive measures that can help reduce the risk of requiring surgery:
1. Pelvic Floor Exercises:
Regular Kegel exercises help strengthen the pelvic floor muscles and improve vaginal tone. These exercises can prevent conditions like prolapse and incontinence, reducing the need for surgery.
2. Healthy Lifestyle:
Maintaining a healthy weight and staying physically active can reduce the risk of pelvic floor issues. Avoiding smoking, which weakens connective tissue, can also help preserve vaginal and perineal health.
3. Proper Childbirth Management:
Choosing the appropriate mode of delivery (vaginal birth vs. cesarean section) and following proper perineal care during labor can reduce the risk of perineal tears and damage.
4. Post-Surgery Care:
After vaginal or perineal surgery, proper aftercare is essential to ensure optimal healing. This may include avoiding sexual activity for a few weeks, using prescribed ointments, and performing pelvic floor exercises to maintain results.
While vaginal and perineal plastic surgeries are generally safe, there are potential complications:
-
Infection:
As with any surgery, there is a risk of infection. Proper post-operative care, including keeping the surgical area clean, is essential to reduce the risk of infection. -
Scarring:
Scarring is a common complication, particularly with excisional procedures. Some women may experience thickened or raised scars at the surgical site. -
Bleeding:
Post-operative bleeding is common but should subside in a few days. Excessive bleeding may require medical intervention. -
Recurrence of Symptoms:
In some cases, symptoms such as vaginal laxity or prolapse may recur after surgery, especially if preventive measures like pelvic floor exercises are not followed. -
Changes in Sensation:
Some women may experience changes in sexual sensation following surgery, such as decreased sensitivity or pain during intercourse.
Living with the outcomes of vaginal and perineal plastic surgery requires careful management of physical and emotional well-being:
-
Emotional Adjustment:
Many women feel a significant improvement in confidence and satisfaction after surgery, but there may be an emotional adjustment period as well. Counseling or support groups can help manage any emotional concerns. -
Sexual Health:
Following surgery, women may experience enhanced sexual satisfaction, but it’s important to wait for full healing before resuming sexual activity. Lubrication and communication with a partner can help ensure comfort and enjoyment. -
Long-Term Care:
To maintain the benefits of surgery, it’s important to continue pelvic floor exercises and practice healthy lifestyle habits, such as avoiding constipation and maintaining a healthy weight.
1. What is vaginal and perineal plastic surgery?
Vaginal and perineal plastic surgery, also known as vaginal rejuvenation or perineoplasty, refers to surgical procedures that aim to improve the appearance and function of the vaginal and perineal area. These procedures are often performed for aesthetic reasons, as well as to treat medical conditions resulting from childbirth, aging, or trauma.
2. Who is a good candidate for vaginal and perineal plastic surgery?
Ideal candidates for vaginal and perineal plastic surgery are individuals who are in good overall health, have realistic expectations, and are seeking improvement in the appearance or function of their vaginal and perineal areas. Women who have experienced vaginal laxity, perineal tears, or changes due to childbirth, aging, or sexual discomfort may consider these surgeries.
3. What conditions can vaginal and perineal plastic surgery treat?
Vaginal and perineal plastic surgery can address various conditions such as:
-
Vaginal laxity (looseness or stretching of the vaginal walls)
-
Perineal tears from childbirth
-
Labial hypertrophy (enlarged labia)
-
Vaginal prolapse (descent of the vaginal walls)
-
Scar tissue or damage from trauma or surgery
-
Urinary incontinence or sexual dysfunction
4. What are the different types of vaginal and perineal plastic surgeries?
Common procedures in vaginal and perineal plastic surgery include:
-
Labiaplasty: Surgical reduction of enlarged or uneven labia.
-
Vaginoplasty: Tightening of the vaginal walls to restore tone and improve sensation.
-
Perineoplasty: Reconstruction of the perineum to repair damage from childbirth or trauma.
-
Hymenoplasty: Reconstruction of the hymen, often for cultural or personal reasons.
5. What is the recovery process like after vaginal and perineal plastic surgery?
Recovery after vaginal and perineal plastic surgery typically involves:
-
Resting for a few days to a week.
-
Avoiding sexual activity and heavy physical activity for at least 6-8 weeks.
-
Taking pain medication as prescribed.
-
Applying prescribed ointments or creams for healing.
-
Attending follow-up appointments to monitor progress.
Healing times can vary depending on the procedure and individual factors.
6. Are the results of vaginal and perineal plastic surgery permanent?
While the results of vaginal and perineal plastic surgery are long-lasting, they may not be permanent. Factors like aging, hormonal changes, and future pregnancies may impact the outcomes. Some individuals may need additional treatments or procedures in the future to maintain results.
7. What are the risks and complications associated with vaginal and perineal plastic surgery?
As with any surgery, there are potential risks and complications, including:
-
Infection
-
Bleeding
-
Scarring
-
Nerve damage
-
Changes in sexual sensation
-
Wound healing problems
It’s essential to follow your surgeon's aftercare instructions to minimize these risks.
8. Can vaginal and perineal plastic surgery improve sexual satisfaction?
Many patients report improved sexual satisfaction after vaginal rejuvenation procedures such as vaginoplasty and labiaplasty. These procedures can help tighten the vaginal muscles, improve vaginal sensation, and enhance the aesthetic appearance of the genital area, leading to a boost in confidence and sexual pleasure.
9. Is vaginal and perineal plastic surgery covered by insurance?
Vaginal and perineal plastic surgery is typically considered a cosmetic procedure, which means it is usually not covered by insurance. However, if the surgery is performed for medical reasons, such as correcting a vaginal prolapse or treating incontinence, it may be partially covered by insurance. It’s essential to check with your insurance provider for specific coverage details.
10. How should I prepare for vaginal and perineal plastic surgery?
Preparation for vaginal and perineal plastic surgery typically involves:
-
A thorough consultation with a qualified surgeon to discuss your goals and medical history.
-
Undergoing any necessary lab tests or pre-surgical evaluations.
-
Avoiding smoking and certain medications that can affect healing.
-
Arranging for post-surgery care, including assistance during the recovery period.
Your surgeon will provide specific instructions tailored to your surgery.
The other Gynecology Procedures are:
Few Major Hospitals for Vaginal & Perineal Plastic Surgery are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


