Brachial plexus surgery is a specialized procedure aimed at treating injuries to the brachial plexus, a network of nerves that control the muscles of the shoulder, arm, and hand. The brachial plexus consists of five nerve roots (C5, C6, C7, C8, and T1), which originate from the spinal cord in the neck and extend into the arm. Injuries to these nerves can result in loss of function or feeling in the affected arm.
Brachial plexus injuries can be caused by trauma, such as car accidents, falls, or sports injuries. In some cases, injuries may also result from birth-related trauma or tumors pressing on the nerve roots. Depending on the severity of the injury, the damage to the brachial plexus can range from mild nerve compression to complete nerve rupture.
Brachial plexus surgery aims to restore function and sensation by repairing, reconstructing, or rerouting damaged nerves. The goal is to improve muscle strength, function, and sensation in the affected arm, ultimately enhancing the patient's quality of life.
This surgery can be highly complex and often requires a multi-disciplinary approach involving neurosurgeons, plastic surgeons, and rehabilitation specialists to achieve the best possible outcomes.
Brachial plexus injuries can result from various causes, including trauma, congenital conditions, and medical complications. Understanding the causes and risk factors is crucial for diagnosing and managing these injuries.
1. Traumatic Injuries:
-
Motor Vehicle Accidents: The most common cause of brachial plexus injuries is trauma from motor vehicle accidents, where the head and neck are forced into extreme positions, stretching or tearing the brachial plexus.
-
Sports Injuries: Contact sports such as football, rugby, and hockey can lead to brachial plexus injuries due to direct impacts, neck hyperextension, or shoulder dislocation.
-
Falls: Accidents involving falls, especially from a height, can also lead to damage to the brachial plexus, particularly when the arms are stretched out to break the fall.
2. Birth-Related Injuries:
-
Erb’s Palsy: One of the most common forms of brachial plexus injury in newborns is Erb’s palsy, which typically occurs during a difficult delivery. It is caused when excessive pulling on the baby’s neck during birth stretches or tears the brachial plexus nerves.
-
Shoulder Dystocia: In some cases, shoulder dystocia (when the baby’s shoulder gets stuck during delivery) can result in brachial plexus injury.
3. Medical Conditions:
-
Tumors or Masses: Tumors or mass lesions near the brachial plexus, including neck tumors or lung cancers, can compress the nerves and lead to functional impairment.
-
Infections: Infections such as herpes zoster (shingles) can also cause damage to the brachial plexus nerves, resulting in pain and weakness in the arm.
4. Other Risk Factors:
-
Age: Older individuals may be more susceptible to brachial plexus injuries due to degenerative conditions such as spinal stenosis or cervical disc disease, which can put pressure on the brachial plexus nerves.
-
Chronic Conditions: Certain neurological conditions such as diabetes may increase the risk of nerve damage due to poor blood circulation and nerve degeneration.
The symptoms and signs of a brachial plexus injury vary depending on the location and severity of the nerve damage. The hallmark of these injuries is weakness or paralysis in the arm, but additional symptoms may occur as well.
1. Common Symptoms:
-
Weakness or Paralysis: The most noticeable symptom of brachial plexus injury is weakness or paralysis in the arm or hand. The individual may find it difficult to move the arm, grasp objects, or lift the hand.
-
Loss of Sensation: Nerve damage may lead to numbness or tingling in the arm, shoulder, or hand, depending on which nerves are affected.
-
Pain: In some cases, a brachial plexus injury can cause sharp or burning pain, particularly when the nerves are stretched or irritated. This pain is typically felt in the shoulder or upper arm.
-
Shoulder and Hand Dysfunction: Loss of function in the shoulder, elbow, or wrist is common, leading to difficulties with everyday tasks such as lifting, writing, or dressing.
2. Specific Signs Based on Nerve Damage:
-
C5-C6 Injury (Upper Brachial Plexus): Affects the shoulder and biceps. Symptoms include difficulty with shoulder abduction (lifting the arm), weak biceps, and limited elbow flexion.
-
C7 Injury (Middle Brachial Plexus): Affects the triceps and wrist extensors, leading to weakness in wrist extension and difficulty straightening the arm.
-
C8-T1 Injury (Lower Brachial Plexus): Affects the hand and fingers, leading to weak grip strength, finger dexterity loss, and possible claw hand deformity.
The diagnosis of a brachial plexus injury begins with a thorough medical history and physical examination to evaluate muscle strength, sensation, and reflexes. Several diagnostic tests can help confirm the extent and location of the injury:
1. Neurological Examination:
-
A detailed neurological examination is conducted to assess muscle strength, sensation, reflexes, and coordination in the affected arm.
-
The doctor may test specific nerve functions to identify which branches of the brachial plexus are affected.
2. Imaging Tests:
-
MRI (Magnetic Resonance Imaging): MRI can provide detailed images of the brachial plexus, spinal cord, and surrounding structures. It helps identify any structural abnormalities, tumors, or herniated discs that may be pressing on the nerves.
-
CT Scan (Computed Tomography): A CT scan can be used to examine the bones and tissues around the brachial plexus, helping to identify fractures or other injuries.
3. Electromyography (EMG) and Nerve Conduction Studies:
-
EMG measures the electrical activity of muscles and can help assess nerve damage by detecting abnormal signals from affected muscles.
-
Nerve conduction studies test how well the nerves transmit electrical impulses. These tests help determine the extent of nerve damage and whether the injury is located at the nerve root, brachial plexus, or peripheral nerve.
4. Surgical Consultation:
-
A neurosurgeon or plastic surgeon specializing in nerve injuries will perform a detailed evaluation and discuss surgical options if necessary.
Brachial plexus surgery is used to repair, reconstruct, or reroute damaged nerves to restore function and sensation. There are several treatment options, and the choice of procedure depends on the severity of the injury, the specific nerves involved, and the time elapsed since the injury.
1. Nerve Repair or Reconstruction:
-
Nerve Grafting: If the nerves are severed, nerve grafting is often performed to repair the damage. Healthy nerve tissue is taken from another part of the body (often the sural nerve in the leg) and grafted to reconnect the damaged nerves.
-
Nerve Transfer: In some cases, nearby healthy nerves can be rerouted to replace damaged ones, improving function in the affected muscles.
2. Muscle Transfer:
-
If nerve repair is not feasible, a muscle transfer can be performed. This involves moving a healthy muscle from another part of the body to restore function in the shoulder or arm.
3. Tendon or Joint Surgery:
-
Tendon transfers or joint stabilization surgery may be performed in cases where the muscles are weakened or paralyzed. This can help restore some function and improve mobility.
4. Rehabilitation and Physical Therapy:
-
After surgery, physical therapy and occupational therapy are critical for restoring strength, flexibility, and function in the arm. Rehabilitation can help patients regain motor skills and adapt to any long-term functional deficits.
Although some brachial plexus injuries are caused by unavoidable accidents, certain preventive measures can reduce the risk of injury:
1. Preventing Trauma:
-
Wearing protective gear in high-risk activities such as sports (football, rugby, etc.) or during motor vehicle travel can prevent traumatic injuries to the neck and shoulders.
-
Proper techniques in lifting and manual labor can help avoid strain on the neck and shoulders.
2. Managing Existing Conditions:
-
For individuals with underlying conditions such as cervical spine issues, herniated discs, or degenerative changes, early intervention and conservative treatment can prevent the progression of nerve compression.
3. Post-Surgical Rehabilitation:
-
Early and consistent physical therapy is essential for maximizing recovery and preventing complications such as contractures (tightening of muscles) or frozen shoulder.
Although brachial plexus surgery can significantly improve outcomes, there are potential complications:
1. Infection:
-
As with any surgical procedure, there is a risk of infection at the incision site. This risk is minimized with proper surgical techniques and post-operative care.
2. Nerve Injury:
-
While nerve repair aims to restore function, there is always a risk of further nerve damage during surgery, especially if the nerves are fragile or scar tissue is present.
3. Incomplete Recovery:
-
Despite surgery, some individuals may experience only partial recovery of function. Regeneration of nerves is a slow process, and full recovery may take months or even years, with some individuals experiencing persistent weakness or numbness.
4. Muscle Weakness or Atrophy:
-
If muscles are not properly reconnected to healthy nerves or if rehabilitation is inadequate, muscle weakness or atrophy (muscle wasting) may persist.
Living with a brachial plexus injury and undergoing surgery can be challenging, but with the right support and rehabilitation, individuals can regain functionality and improve their quality of life.
1. Emotional and Psychological Support:
-
The physical and emotional toll of brachial plexus injury and surgery can be significant. Support from family, friends, and mental health professionals can help individuals cope with the challenges of recovery.
2. Long-Term Rehabilitation:
-
Long-term physical therapy and occupational therapy are essential for optimizing recovery and regaining strength and mobility in the affected arm.
3. Adaptive Equipment:
-
In cases where full recovery is not possible, adaptive devices such as specialized grips, prosthetics, or assistive technology can help improve daily function and independence.
1. What is brachial plexus surgery?
Brachial plexus surgery is a procedure used to treat injuries or damage to the brachial plexus, a network of nerves that controls movement and sensation in the shoulder, arm, and hand. This surgery aims to repair or reconstruct the damaged nerves to restore function in the affected limb. It is often necessary when the brachial plexus is injured due to trauma, birth injuries, or other conditions.
2. What causes brachial plexus injury?
Brachial plexus injuries can occur due to various reasons, including:
-
Trauma: Such as a motor vehicle accident, sports injuries, or falls.
-
Birth-related injuries: The most common cause in infants is shoulder dystocia, where the baby’s shoulder gets stuck during delivery.
-
Tumors: Growths or lesions pressing on the brachial plexus nerves.
-
Repetitive strain: Injuries from repetitive movements in activities like heavy lifting or overhead motions.
-
Neurological conditions: Certain diseases that affect nerve function, like plexopathy or neuropathy.
3. What are the symptoms of a brachial plexus injury?
Symptoms of a brachial plexus injury can vary depending on the severity and type of injury but generally include:
-
Weakness or paralysis in the shoulder, arm, or hand.
-
Loss of sensation or tingling in the affected limb.
-
Pain or burning sensations in the arm or shoulder.
-
Inability to lift or move the arm properly.
-
Muscle atrophy or wasting in severe cases.
4. When is brachial plexus surgery necessary?
Brachial plexus surgery is typically considered when:
-
Conservative treatments like physical therapy and medication do not improve function.
-
The injury involves nerve rupture or complete loss of function in the affected limb.
-
Nerve recovery is unlikely without surgical intervention.
-
In cases of birth injuries, when early intervention is crucial for proper arm development.
5. What types of brachial plexus surgery are available?
The type of surgery depends on the location and extent of the nerve injury. Common surgeries include:
-
Nerve grafting: A portion of healthy nerve tissue is used to replace the damaged section.
-
Nerve transfer: A nearby healthy nerve is rerouted to restore function to the injured nerve.
-
Nerve repair: In some cases, the damaged nerve can be surgically reattached.
-
Muscle and tendon transfers: If nerve repair is not possible, nearby muscles or tendons may be repositioned to help improve arm movement.
-
Debulking or tumor removal: If the injury is caused by a tumor, it may be surgically removed to relieve pressure on the brachial plexus.
6. How is brachial plexus surgery performed?
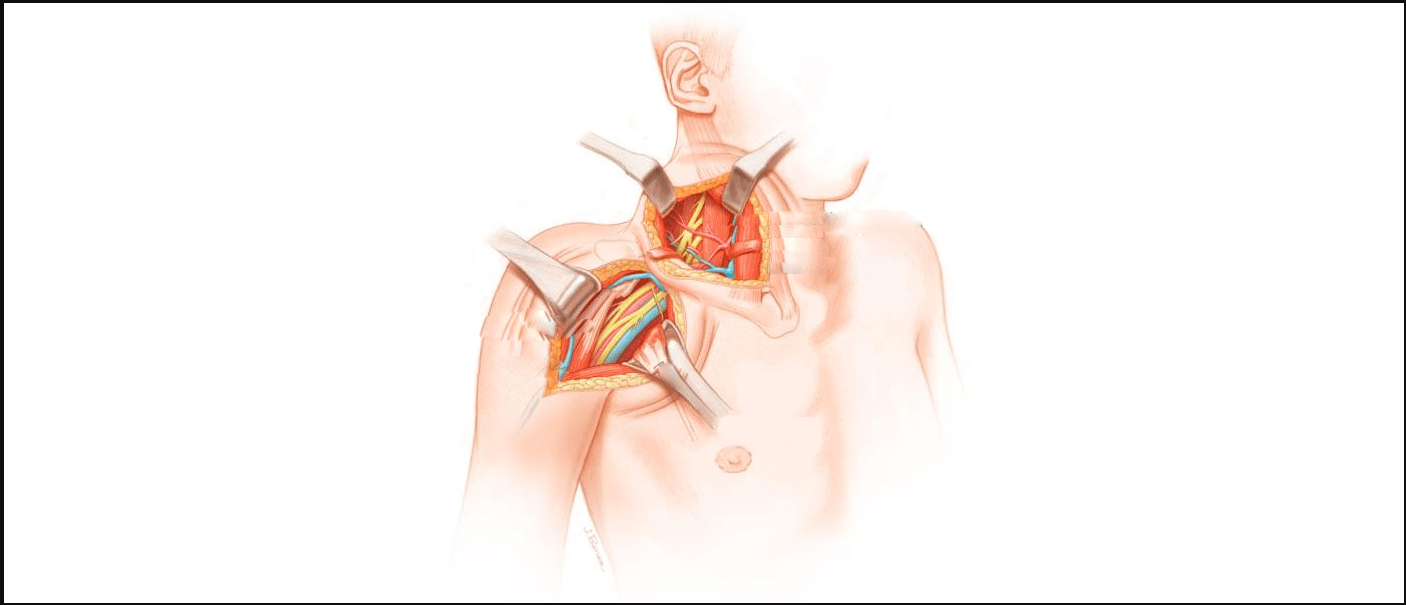
Brachial plexus surgery is typically performed under general anesthesia. The surgeon may approach the injury through an incision in the neck, shoulder, or upper chest, depending on where the damage occurred. In the case of nerve grafting, healthy nerve tissue is harvested, prepared, and used to reconnect the injured nerves. The surgery may take several hours, depending on the complexity of the injury.
7. What is the recovery process after brachial plexus surgery?
Recovery from brachial plexus surgery involves:
-
Hospital stay: Typically, patients stay in the hospital for several days for monitoring and pain management.
-
Physical therapy: Rehabilitation and physical therapy are essential to regain strength, improve range of motion, and retrain muscles.
-
Recovery time: Recovery can take several months to years, depending on the severity of the injury and surgery. Nerve regeneration is a slow process, and full recovery may not be possible in all cases.
8. What are the risks of brachial plexus surgery?
Like any surgery, brachial plexus surgery carries some risks, including:
-
Infection: At the site of the incision or within the nerves.
-
Nerve injury: In rare cases, additional nerve damage can occur during surgery.
-
Scarring: Some patients may develop significant scarring that could limit movement.
-
Incomplete recovery: Full function may not always be restored, depending on the extent of the nerve damage.
-
Blood clots: As with any surgery, there is a risk of deep vein thrombosis (DVT) or pulmonary embolism (PE).
9. How long does it take to see results from brachial plexus surgery?
It can take several months to a few years to see the full benefits of brachial plexus surgery. Nerve regeneration is a slow process, with improvement often occurring over time. The initial recovery phase may involve muscle strengthening and physical therapy, and patients may begin to notice gradual improvements in muscle function and sensation. Full recovery can take up to 18-24 months in some cases, depending on the extent of the injury and surgery.
10. Can brachial plexus surgery restore full function of the arm?
While brachial plexus surgery can significantly improve function and reduce symptoms, full recovery may not always be achievable, especially if the injury is severe. In cases where nerve regeneration is slow or incomplete, patients may still experience some weakness or limited function in the arm. However, with appropriate surgical intervention, physical therapy, and rehabilitation, many individuals can regain significant function and improve quality of life.
The other Neurology Procedures are:
Few Major Hospitals for Brachial Plexus Surgery are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.