Laminoplasty is a sophisticated spinal surgery primarily performed to relieve pressure on the spinal cord caused by various degenerative or structural abnormalities, especially within the cervical (neck) spine. This pressure often results from a condition called cervical myelopathy, which can lead to progressive neurological deficits if left untreated. Unlike laminectomy, where the lamina (the part of the vertebra that protects the spinal cord) is removed entirely, laminoplasty preserves and reshapes the lamina, offering spinal decompression without compromising spinal integrity.
Developed initially in Japan, laminoplasty has gained global attention for being a motion-preserving, less invasive alternative to spinal fusion. It is typically recommended when multiple levels of the cervical spine are affected and where maintaining spinal stability and mobility is vital. Laminoplasty has shown excellent outcomes in reducing symptoms, preventing further neurological deterioration, and enhancing the quality of life for patients suffering from spinal cord compression.
This guide is designed to walk you through every aspect of laminoplasty — from causes and diagnosis to treatment and life after surgery — helping patients and caregivers make informed decisions.
Although laminoplasty itself is a surgical intervention, understanding what necessitates it involves examining the underlying conditions that lead to spinal cord compression. These include:
Common Underlying Conditions:
-
Cervical Spondylotic Myelopathy (CSM):
-
Age-related wear and tear causes degeneration of vertebral discs and joints.
-
Leads to narrowing of the spinal canal and compresses the spinal cord.
-
-
Congenital Spinal Stenosis:
-
Some individuals are born with a narrower-than-normal spinal canal, predisposing them to compression with even minor disc herniations or trauma.
-
-
Herniated Discs:
-
Displaced discs may bulge into the spinal canal and exert pressure on the spinal cord and nerves.
-
-
Ossification of the Posterior Longitudinal Ligament (OPLL):
-
A condition often seen in East Asian populations where spinal ligaments harden and narrow the canal.
-
-
Spinal Tumors, Infections, or Trauma:
-
Rare causes that necessitate immediate surgical intervention.
-
Risk Factors:
-
Aging (especially over 50 years)
-
Previous spine surgeries or injuries
-
Occupations involving repetitive neck motion or strain
-
Genetic predisposition to spinal canal narrowing
-
Autoimmune diseases like rheumatoid arthritis
Patients who may benefit from laminoplasty typically present with a range of symptoms, some subtle and others more pronounced. These symptoms may worsen over time, and early recognition is essential.
Neurological Symptoms:
-
Neck pain or stiffness
-
Tingling, numbness, or weakness in the arms or hands
-
Poor coordination or clumsiness in hand movements
-
Frequent dropping of objects
-
Gait disturbances or difficulty walking
-
Unsteadiness while standing or climbing stairs
-
Urinary urgency or incontinence (in advanced cases)
Functional Impairment:
-
Inability to perform fine motor tasks such as buttoning shirts or writing.
-
Difficulty in lifting or moving arms overhead.
These signs often mimic other neurological disorders, making accurate diagnosis essential to avoid mismanagement.
The diagnosis process involves a thorough medical and neurological evaluation, coupled with advanced imaging techniques to pinpoint the exact cause and extent of spinal cord compression.
Clinical Evaluation:
-
Complete history of symptoms (onset, progression, daily impact)
-
Physical and neurological exams (reflexes, sensation, strength, balance)
Imaging and Diagnostic Tools:
-
MRI (Magnetic Resonance Imaging):
-
Provides detailed images of soft tissues, spinal cord, and nerve roots.
-
Confirms degree and level of spinal cord compression.
-
-
CT Scan (with or without Myelogram):
-
Offers a more detailed bone structure view.
-
Helpful in evaluating ossified ligaments or bone spurs.
-
-
X-rays:
-
Show spinal alignment, curvature, and bone abnormalities.
-
-
Electromyography (EMG) and Nerve Conduction Studies (NCS):
-
May be used to rule out peripheral nerve disorders like carpal tunnel syndrome.
-
Accurate diagnosis is key to determining if laminoplasty is the most appropriate treatment, particularly when multiple spinal levels are involved.
Laminoplasty is indicated in moderate to severe spinal stenosis with neurological symptoms affecting multiple levels of the cervical spine. It is often preferred over laminectomy and fusion in specific scenarios due to its motion-preserving advantage.
Types of Laminoplasty:
-
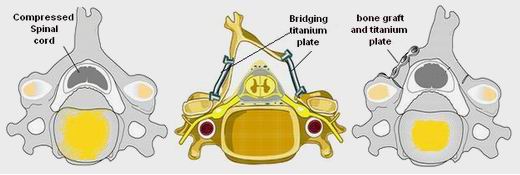
Open-Door Laminoplasty:
-
The lamina is cut on one side and hinged on the other to "open" the spinal canal.
-
The open side is held with a metal plate or bone spacer.
-
-
Double-Door (French-Door) Laminoplasty:
-
The lamina is split centrally, and both sides are opened like double doors.
-
Ideal for symmetrical decompression.
-
Procedure Overview:
-
Performed under general anesthesia
-
Involves 1–2 hours of surgery depending on complexity
-
Requires minimal bone removal
-
Postoperative drain may be placed temporarily
Postoperative Hospital Stay:
-
Most patients stay 2–3 days
-
Neck collar may be used for comfort
-
Pain is managed with analgesics and anti-inflammatories
Alternatives to Laminoplasty:
-
Laminectomy with Fusion: Complete removal of lamina and hardware insertion
-
Anterior Cervical Discectomy and Fusion (ACDF): For anterior compressive lesions
-
Non-surgical therapies: Reserved for early or mild cases
While congenital and degenerative causes of compression cannot always be prevented, spinal health and early intervention play a vital role in delaying or avoiding surgical interventions like laminoplasty.
Prevention Tips:
-
Maintain good posture (especially during long periods of sitting or computer work)
-
Regular stretching and strengthening exercises for neck and back
-
Use ergonomically designed chairs and desks
-
Avoid smoking — reduces bone health and disc hydration
-
Maintain healthy weight to reduce spinal pressure
Management After Laminoplasty:
-
Adherence to prescribed physical therapy and home exercises
-
Avoidance of high-impact activities during early recovery
-
Scheduled follow-ups with spine specialist
-
Regular imaging (X-ray or MRI) as advised
Like any surgical procedure, laminoplasty comes with certain risks and potential complications, although it is considered generally safe when performed by an experienced spine surgeon.
Possible Complications:
-
C5 palsy: Weakness in shoulder/arm muscles (usually temporary)
-
Neck stiffness or reduced motion
-
Infection at surgical site
-
Delayed wound healing or hematoma
-
Hardware issues (rarely)
-
Persistent symptoms if compression is not fully relieved
Risk Mitigation:
-
Preoperative planning with high-resolution imaging
-
Intraoperative neuromonitoring to protect spinal cord
-
Use of antibiotic prophylaxis
-
Post-surgical rehabilitation and monitoring
Recovery from laminoplasty is gradual and can take several months, but most patients regain functionality and enjoy significant symptom relief. The goal is not only to decompress the spinal cord but also to preserve motion and avoid the limitations of spinal fusion.
Recovery Timeline:
-
Weeks 1–2: Rest, pain management, limited activity
-
Weeks 3–6: Begin guided physical therapy, light activity
-
3 Months: Return to normal routine; motion improves
-
6–12 Months: Continued strengthening; full recovery for most
Lifestyle Adjustments:
-
Stay active with low-impact exercises like walking or swimming
-
Modify work environment to reduce strain on the neck
-
Prioritize spinal care in daily activities (lifting, posture)
-
Follow up annually or as recommended
Emotional and Psychological Aspects:
-
Anxiety and depression may accompany long-standing pain or disability
-
Counseling and support groups can assist with mental health
-
Patient education helps reduce fear and increase confidence
1. What is Laminoplasty and why is it performed?
Laminoplasty is a surgical procedure used to relieve pressure on the spinal cord in the neck region (cervical spine). It involves reshaping or repositioning the lamina — the back part of the vertebra — to create more space for the spinal cord. It is commonly performed to treat conditions like cervical spinal stenosis, ossification of the posterior longitudinal ligament (OPLL), or myelopathy caused by degenerative changes.
2. How is Laminoplasty different from Laminectomy?
Laminoplasty preserves the lamina by creating a "hinge" that keeps the bone in place, allowing for spinal cord decompression while maintaining spinal stability. In contrast, a laminectomy involves completely removing the lamina, which may require spinal fusion to maintain support, especially if multiple levels are treated. Laminoplasty is often preferred in younger or more active patients due to better preservation of spine motion.
3. Who is a suitable candidate for Laminoplasty?
Ideal candidates for laminoplasty are individuals with multi-level cervical spinal stenosis or myelopathy without significant spinal instability. It’s commonly recommended for patients who still have good alignment in the cervical spine and need decompression at multiple levels. Patients with kyphotic deformity or instability may not be suitable and might need alternative procedures.
4. What are the risks or complications of Laminoplasty?
Like any surgical procedure, laminoplasty carries some risks. Possible complications include:
-
Infection
-
Nerve root injury
-
C5 palsy (shoulder weakness)
-
Persistent pain
-
Reduced neck motion
-
Spinal instability in rare cases
-
Dural tear or cerebrospinal fluid (CSF) leakage
However, with proper surgical technique and post-operative care, most patients recover well.
5. How long does it take to recover from Laminoplasty?
Initial recovery typically takes 4 to 6 weeks, with gradual improvement in strength and mobility. Full recovery can take 3 to 6 months, depending on the individual’s overall health, the severity of pre-operative symptoms, and adherence to rehabilitation. Physical therapy is often recommended post-surgery to improve outcomes.
6. Will I lose mobility in my neck after Laminoplasty?
Some patients may experience a slight decrease in neck flexibility following laminoplasty, especially with multi-level surgeries. However, because the procedure preserves spinal structures, most patients retain a good range of motion. The extent of motion loss is usually minimal compared to procedures like spinal fusion.
7. Is Laminoplasty a permanent solution for spinal cord compression?
In many cases, laminoplasty provides long-term relief from spinal cord compression and prevents the progression of neurological symptoms. However, degenerative changes may continue with aging, and patients may need future treatment. Regular follow-ups and spine health maintenance are essential for long-term success.
8. What kind of anesthesia is used during Laminoplasty?
Laminoplasty is performed under general anesthesia. This means the patient is fully asleep and unaware during the procedure. The surgical team closely monitors vital signs and comfort throughout the surgery to ensure safety and effectiveness.
9. What should I expect during the hospital stay after Laminoplasty?
Most patients stay in the hospital for 2 to 4 days post-surgery. During this time, pain is managed with medication, and physical activity is gradually increased under supervision. Patients are encouraged to walk and perform light neck movements. Before discharge, patients receive instructions on wound care, medications, activity restrictions, and follow-up appointments.
10. Can Laminoplasty be done using minimally invasive techniques?
Yes, in some cases, minimally invasive laminoplasty can be performed, particularly with advanced surgical tools and techniques. These procedures use smaller incisions, result in less blood loss, and offer quicker recovery. However, the decision depends on the patient’s spinal anatomy, the extent of compression, and the surgeon’s expertise.
The other Neurology Procedures are:
Few Major Hospitals for Laminoplasty are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.



