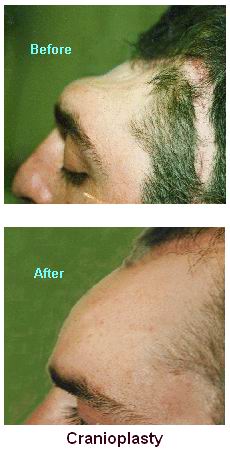
Cranioplasty is a surgical procedure performed to repair or reconstruct the skull, specifically after a traumatic injury, disease, or previous surgery that has caused a skull defect. The goal of cranioplasty is to restore the normal shape, structure, and function of the skull, as well as to protect the underlying brain. This surgery is typically performed when there is a gap or defect in the skull resulting from conditions such as trauma, brain surgery, tumors, or congenital abnormalities.
The cranioplasty procedure involves the use of a variety of materials, including metal, acrylic, or custom-fabricated implants, to fill in the defect. In certain cases, bone grafts from the patient or a donor may be used to repair the skull. Cranioplasty may be necessary to restore the skull's protective function, prevent complications like infection, and improve the cosmetic appearance of the patient.
Cranioplasty can be performed under general anesthesia, and the surgery's complexity depends on the size, location, and nature of the skull defect. The recovery time varies depending on the patient's overall health, the size of the defect, and the materials used for the reconstruction.
Cranioplasty is generally performed in response to an abnormality or defect in the skull. The causes of these defects may be trauma-related, congenital, or due to medical conditions requiring surgery. Below are some of the most common causes and risk factors that may lead to the need for cranioplasty:
1. Traumatic Brain Injury (TBI):
-
Traumatic brain injuries are among the leading causes of skull defects. In accidents, falls, or blunt force trauma, the skull may be fractured or shattered. If the injury leads to the removal of a portion of the skull, cranioplasty is often performed to repair the defect and restore the skull's protective function.
2. Brain Tumor Surgery:
-
Surgical removal of brain tumors (e.g., gliomas or meningiomas) may necessitate the removal of a portion of the skull. After the tumor is excised, cranioplasty is performed to restore the skull's integrity.
3. Aneurysms or Vascular Abnormalities:
-
In some cases, the treatment of cerebral aneurysms or vascular malformations involves removing part of the skull to access the brain. Once the underlying condition is addressed, cranioplasty is performed to close the defect.
4. Infection:
-
Infections such as osteomyelitis (infection of the bone) or brain abscesses can cause the bone to become weakened or damaged, necessitating surgical intervention to remove the infected tissue and reconstruct the skull.
5. Congenital Abnormalities:
-
Some individuals are born with congenital skull defects or cranial malformations that affect the shape and structure of the skull. These conditions may require cranioplasty for cosmetic, functional, or developmental reasons.
6. Previous Surgery:
-
In some cases, cranioplasty is required following earlier surgical procedures, particularly when a portion of the skull was removed for access to brain tissue or for medical treatment.
7. Skull Deformities:
-
Skull deformities caused by conditions such as craniosynostosis (premature fusion of skull sutures) can affect skull growth and require reconstructive surgery to restore normal skull shape.
The symptoms that indicate the need for cranioplasty typically arise after a brain injury, surgery, or abnormal skull development. Some of the signs and symptoms may include:
1. Skull Defects:
-
Visible gaps or depressions in the skull caused by trauma, surgery, or congenital abnormalities are the most apparent sign that cranioplasty may be necessary. These defects may vary in size and shape and can be seen or felt on physical examination.
2. Increased Risk of Infection:
-
An exposed skull or an incomplete skull can make the brain more vulnerable to infection. In cases of severe trauma, bone removal, or surgical procedures, the exposed brain tissue can become infected, necessitating cranioplasty to restore the skull's integrity and protect the brain from external pathogens.
3. Headaches:
-
Patients with skull defects may experience frequent headaches, especially if the defect is large enough to impact brain function or cause pressure changes inside the skull.
4. Neurological Symptoms:
-
In some cases, individuals with significant skull defects may experience neurological symptoms such as dizziness, difficulty concentrating, memory issues, or motor impairment. These symptoms may indicate that the skull defect is affecting brain function and may require surgical intervention to correct.
5. Cosmetic and Aesthetic Concerns:
-
Patients may seek cranioplasty for cosmetic reasons if they are self-conscious about visible skull defects caused by trauma, surgery, or birth defects.
The diagnosis that leads to cranioplasty typically follows an evaluation of the underlying cause of the skull defect. Several diagnostic tests and imaging studies are used to assess the defect and determine the appropriate treatment:
1. Physical Examination:
-
The doctor will perform a physical examination to assess the size, shape, and location of the skull defect. The examination may include a neurological evaluation to check for any associated symptoms such as weakness, numbness, or cognitive changes.
2. Imaging Studies:
-
CT Scan (Computed Tomography): A CT scan provides detailed images of the skull and brain, allowing doctors to assess the size and depth of the defect and any associated injuries or abnormalities. It can also be used to plan the cranioplasty procedure.
-
MRI (Magnetic Resonance Imaging): An MRI may be used to provide additional details about the brain and surrounding structures, particularly when there is concern about underlying neurological damage or conditions that require surgery.
-
3D Imaging: Some specialized centers use 3D imaging techniques to create precise maps of the skull defect. This allows for custom fabrication of implants that fit the skull defect perfectly.
3. Blood Tests:
-
Blood tests may be performed to assess the patient's overall health and check for any underlying infection, clotting disorders, or other medical issues that could affect the surgery or recovery process.
Cranioplasty is performed when a skull defect requires closure. Several treatment options are available depending on the nature and size of the defect, as well as the patient’s overall health:
1. Bone Flap Reconstruction:
-
In cases where a portion of the skull has been removed due to trauma or surgery, the original bone flap may be replaced. If the bone flap is preserved and not damaged, it can be reattached during cranioplasty.
2. Custom Implants:
-
For patients with larger or irregular skull defects, custom-made implants can be used. These implants are made from materials such as titanium, acrylic, or polymer composites and are designed to fit the specific shape and size of the defect. 3D printing technology is often used to create these implants with precise accuracy.
3. Bone Grafting:
-
In some cases, bone grafts from the patient or a donor may be used to fill in the skull defect. The bone graft may be harvested from the hip, ribs, or another part of the body.
4. Titanium Mesh:
-
Titanium mesh is often used for smaller defects or in areas where a solid bone graft may not be practical. The mesh is placed over the defect, providing structural support and protection to the brain.
5. Reconstruction for Cosmetic Reasons:
-
In some cases, cranioplasty is performed for cosmetic purposes to restore the appearance of the skull following trauma or surgery.
While cranioplasty is a necessary procedure to treat skull defects, certain steps can be taken to reduce the risk of developing skull abnormalities and ensure optimal recovery after surgery:
1. Preventing Skull Trauma:
-
Wearing protective gear during sports, biking, and high-risk activities can help prevent traumatic brain injuries that may require cranioplasty.
-
Seatbelt use while driving is crucial for preventing head trauma from car accidents.
2. Managing Underlying Conditions:
-
Individuals who have conditions such as bone infections, tumors, or vascular malformations should seek early treatment to prevent the need for cranioplasty due to complications from these diseases.
3. Post-Surgical Care:
-
After cranioplasty, wound care and pain management are essential. Patients may need physical therapy and rehabilitation if neurological damage occurred prior to surgery or as a result of the defect.
Although cranioplasty is generally safe, it carries risks, as all surgeries do. Some complications include:
1. Infection:
-
As with any surgery, there is a risk of infection at the incision site or in the implanted material. This is particularly a concern if bone grafts or implants are used.
2. Hematoma:
-
Hematomas (accumulation of blood) may occur after surgery, which could require further treatment.
3. Nerve Damage:
-
In rare cases, the surgery may lead to nerve damage, causing numbness, weakness, or motor impairment in the affected area.
4. Implant Rejection or Displacement:
-
In some cases, the implant may be rejected by the body or displaced, requiring a second surgery to correct the issue.
Living with a skull defect before cranioplasty or recovering after the surgery can be challenging. Here are some tips for individuals living with the condition:
1. Rehabilitation and Recovery:
-
Patients may need rehabilitation to recover from the neurological effects of the underlying condition that led to cranioplasty. Physical therapy, speech therapy, or occupational therapy can help restore function.
2. Psychological Support:
-
Psychological counseling or support groups can help individuals cope with the emotional and psychological challenges of living with a skull defect or undergoing brain surgery.
3. Regular Follow-ups:
-
Patients who have undergone cranioplasty should have regular follow-up appointments to monitor their recovery, check for complications, and ensure the implant or bone flap is functioning correctly.
1. What is Cranioplasty?
Cranioplasty is a surgical procedure in which a piece of the skull is repaired or reconstructed. This surgery is typically performed to restore the shape and structure of the skull after injury, infection, or surgery that has resulted in skull defects or deformities. It is used to improve both the aesthetic appearance of the skull and its protective function.
2. Why is Cranioplasty performed?
Cranioplasty is performed to treat skull defects caused by:
-
Trauma: Such as fractures from accidents, falls, or blunt force injury.
-
Brain surgery: After procedures like craniotomy where a part of the skull is removed to access the brain.
-
Congenital conditions: Skull deformities present from birth.
-
Infection: Infections that cause skull deformities or damage.
-
Tumor removal: When a portion of the skull is removed to remove a brain tumor.
The primary goal is to restore the integrity of the skull and protect the brain.
3. How is Cranioplasty performed?
Cranioplasty is typically performed under general anesthesia. The steps usually include:
-
Incision: The surgeon makes an incision in the scalp over the area that needs to be repaired.
-
Bone graft or prosthetic placement: A piece of bone (from the patient or a donor) or a synthetic material is used to repair the skull defect. In some cases, 3D-printed or customized prosthetics are used for better fitting.
-
Fixation: The new material is securely fixed in place using screws or other fixation devices.
-
Closure: The incision is closed, and the scalp is sutured.
4. What materials are used in Cranioplasty?
The materials used in cranioplasty vary depending on the patient’s condition and the surgeon’s preference, including:
-
Autografts: The patient’s own bone (often taken from another area of the skull or another bone in the body).
-
Allografts: Donor bone from a human cadaver.
-
Synthetic materials: Materials such as titanium, polymethyl methacrylate (PMMA), ceramic, or 3D-printed prosthetic implants.
The choice of material depends on factors such as the size and location of the defect, the patient’s medical history, and the aesthetic outcome desired.
5. What are the risks and complications of Cranioplasty?
While cranioplasty is generally safe, there are some risks and complications, including:
-
Infection: Infection at the surgical site or in the implanted material.
-
Bleeding: There is a risk of bleeding during or after the surgery.
-
Rejection or failure of the graft: The body may reject the implant, or the graft may not fully integrate with the skull.
-
Neurological complications: Rarely, there may be damage to the brain or nerves.
-
Cosmetic concerns: The repaired area may not achieve the desired aesthetic result.
6. How long does it take to recover from Cranioplasty?
Recovery from cranioplasty typically involves:
-
Hospital stay: Most patients stay in the hospital for 1 to 2 days for monitoring and pain management.
-
Physical activity: Patients should avoid heavy physical activity or strenuous movements for 4 to 6 weeks to allow proper healing.
-
Full recovery: Complete recovery can take several weeks to a few months. Follow-up appointments will be necessary to monitor the healing process.
7. What is the success rate of Cranioplasty?
The success rate of cranioplasty is generally high, with most patients experiencing successful restoration of skull integrity and no significant complications. However, success depends on several factors, including the size and location of the defect, the type of material used for reconstruction, and the patient’s overall health. In general, success rates are around 85-95%.
8. Can Cranioplasty be performed on children?
Yes, cranioplasty can be performed on children, especially if they have congenital skull deformities or have undergone surgery for brain tumors or trauma. In children, the procedure may also involve the use of customized implants to accommodate the growing skull. Early intervention is important to ensure proper brain development and prevent any potential developmental delays.
9. Is Cranioplasty a cosmetic procedure?
While cranioplasty can improve the cosmetic appearance of the skull, especially in cases of traumatic injury or deformities, its primary goal is to restore the protective function of the skull. The procedure is necessary to protect the brain from further injury and to address structural issues caused by trauma, surgery, or disease.
10. What should I expect during recovery after Cranioplasty?
During recovery from cranioplasty, patients may experience:
-
Pain or discomfort: Some pain or soreness around the incision and implanted material is common, but it is usually manageable with prescribed pain medications.
-
Swelling and bruising: Swelling or bruising around the surgical area is common and will subside over time.
-
Follow-up appointments: Regular visits to the surgeon will be necessary to monitor the healing process, check for signs of complications, and ensure the implant is securely in place.
The other Neurology Procedures are:
Few Major Hospitals for Cranioplasty are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


