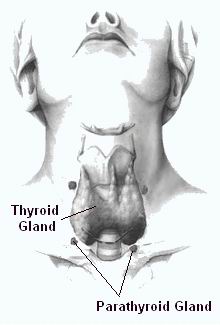
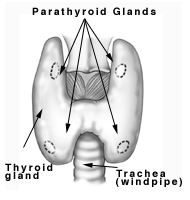
Parathyroid surgery is a medical procedure designed to treat disorders related to the parathyroid glands, which are small, oval-shaped glands located in the neck behind the thyroid. These glands are responsible for producing parathyroid hormone (PTH), which plays a crucial role in regulating the body’s calcium, phosphorus, and vitamin D levels. When these glands become overactive (a condition known as hyperparathyroidism) or develop abnormal growths (such as benign tumors or parathyroid adenomas), surgery may be required.
Parathyroid surgery typically involves the removal of one or more of the parathyroid glands affected by disease. The procedure is often performed on an outpatient basis and is highly effective in treating conditions such as primary hyperparathyroidism, secondary hyperparathyroidism, and parathyroid cancer. The goal of parathyroid surgery is to restore the balance of calcium in the body, alleviate symptoms, and prevent long-term complications such as kidney stones, bone loss, or cardiovascular issues.
With advancements in minimally invasive surgical techniques, parathyroid surgery has become a relatively safe procedure, with a high success rate and faster recovery times compared to traditional open surgery.
The need for parathyroid surgery arises primarily from conditions that affect the function of the parathyroid glands, leading to an overproduction of parathyroid hormone (PTH). The most common reasons for parathyroid surgery include:
1. Primary Hyperparathyroidism:
This condition occurs when one or more of the parathyroid glands become enlarged or form tumors, often benign (parathyroid adenomas). These tumors cause excessive secretion of PTH, resulting in elevated calcium levels in the blood (hypercalcemia). Primary hyperparathyroidism is the most common reason for parathyroid surgery, and it is usually diagnosed through routine blood tests showing abnormal calcium levels.
2. Secondary Hyperparathyroidism:
Secondary hyperparathyroidism develops as a compensatory response to low calcium levels in the body, often due to chronic kidney disease or vitamin D deficiency. In this condition, the parathyroid glands become enlarged in an effort to increase calcium levels. While secondary hyperparathyroidism is generally managed medically, surgery may be necessary if the condition becomes severe and unresponsive to medical treatments.
3. Parathyroid Cancer:
Though rare, parathyroid cancer can cause excessive PTH production and lead to severe hypercalcemia. Surgery is typically the primary treatment for parathyroid cancer, involving the removal of the affected gland(s) and possibly surrounding tissue.
4. Familial Hyperparathyroidism:
In some cases, hyperparathyroidism may be inherited as part of a genetic syndrome such as multiple endocrine neoplasia (MEN), which causes abnormal growth in various endocrine glands. Surgery is often required to remove the affected glands and prevent complications.
Risk Factors:
-
Age: Parathyroid disorders are most commonly diagnosed in people over 50 years old.
-
Gender: Women are more likely to develop primary hyperparathyroidism.
-
Family History: A family history of hyperparathyroidism or endocrine disorders increases the risk.
-
Chronic Kidney Disease: A significant risk factor for developing secondary hyperparathyroidism.
-
Genetic Conditions: Inherited conditions like MEN can increase the risk of developing parathyroid disorders.
Understanding these causes and risk factors is crucial for early diagnosis and determining whether parathyroid surgery is necessary.
When the parathyroid glands become overactive, the body’s calcium levels can become imbalanced, leading to a wide range of symptoms. Common signs of parathyroid disorders that may indicate the need for surgery include:
1. Symptoms of Hypercalcemia:
-
Fatigue and Weakness: Elevated calcium levels can cause feelings of extreme tiredness and muscle weakness.
-
Bone Pain and Fractures: High calcium levels can weaken bones, leading to pain, fractures, or osteoporosis.
-
Kidney Stones: Excessive calcium can cause the formation of kidney stones, leading to pain and urinary issues.
-
Nausea and Vomiting: Digestive issues like nausea, vomiting, and loss of appetite are common.
-
Abdominal Pain: High calcium levels can irritate the stomach and intestines.
-
Frequent Urination and Thirst: The kidneys may struggle to filter excessive calcium, causing increased urination and thirst.
-
Cognitive Issues: Memory problems, confusion, and difficulty concentrating are also possible.
2. Symptoms of Hypocalcemia (in secondary hyperparathyroidism):
-
Muscle Cramps and Spasms: Low calcium levels can cause muscle cramps and spasms, particularly in the hands and feet.
-
Tingling or Numbness: A sensation of tingling or numbness may occur around the mouth, hands, or feet.
-
Severe Weakness: Muscle weakness and fatigue may become more pronounced over time.
3. Symptoms of Parathyroid Cancer:
-
In cases of parathyroid cancer, symptoms may be more severe and include persistent neck lumps, hoarseness, difficulty swallowing, or unexplained weight loss.
If you experience any combination of these symptoms, it is important to seek medical attention promptly. Early detection and surgical intervention can significantly improve outcomes.
Diagnosing parathyroid disorders involves a combination of laboratory tests, imaging studies, and physical examination. The primary goal is to confirm abnormal calcium and PTH levels and identify the underlying cause of the dysfunction.
1. Blood Tests:
-
Serum Calcium: Elevated calcium levels are often the first indication of parathyroid dysfunction.
-
Parathyroid Hormone (PTH) Levels: A blood test measuring PTH levels helps confirm the diagnosis of primary or secondary hyperparathyroidism.
-
Vitamin D Levels: Vitamin D deficiency can contribute to secondary hyperparathyroidism.
2. Imaging Studies:
-
Ultrasound: Neck ultrasound is a non-invasive method to detect parathyroid adenomas or abnormal gland enlargement.
-
Sestamibi Scan (Scintigraphy): A nuclear medicine test that helps locate abnormal parathyroid glands by injecting a small amount of radioactive material.
-
CT Scan or MRI: These imaging tests are used in cases of suspected parathyroid cancer or complex anatomical conditions.
3. Fine Needle Aspiration (FNA):
In some cases, a needle biopsy of a suspicious lump may be performed to determine if it is cancerous.
An accurate diagnosis is crucial for determining the type of parathyroid disorder and the appropriate treatment approach, including surgery.
The primary treatment for parathyroid disorders is surgery, especially when the condition is causing symptoms or complications. The most common surgical options include:
1. Minimally Invasive Parathyroidectomy:
This technique uses small incisions (typically 1-2 cm) and is often performed under local anesthesia with sedation. A small camera (endoscope) is used to visualize the parathyroid glands and remove the affected tissue. This approach is less invasive and has a faster recovery time compared to traditional surgery.
2. Bilateral Neck Exploration:
In more complex cases or when multiple glands are affected, a larger incision may be made to explore both sides of the neck and remove abnormal tissue from one or more parathyroid glands.
3. Parathyroid Cancer Surgery:
For rare cases of parathyroid cancer, surgery involves removing the affected gland(s) along with any surrounding tissue that may be involved. In some cases, lymph nodes may also be removed to check for spread.
4. Reoperation for Recurrence:
In cases where hyperparathyroidism recurs after surgery, a second surgery may be necessary to locate and remove additional abnormal glands.
The choice of surgery depends on the type of parathyroid disorder, the number of glands affected, and the patient’s overall health.
While not all cases of parathyroid disorders can be prevented, certain lifestyle changes and medical treatments can help manage the condition and reduce the risk of complications.
Preventive Measures:
-
Adequate Calcium and Vitamin D Intake: Ensuring sufficient levels of calcium and vitamin D can help maintain healthy parathyroid function.
-
Regular Screenings: For those with a family history of parathyroid disorders or multiple endocrine neoplasia, regular blood tests and imaging studies are essential for early detection.
-
Manage Kidney Disease: If secondary hyperparathyroidism is caused by kidney disease, proper management of kidney function can prevent further complications.
Post-Surgical Management:
-
Calcium and Vitamin D Supplements: After surgery, some patients may need calcium and vitamin D supplements to maintain proper calcium levels.
-
Follow-up Care: Regular blood tests to monitor calcium and PTH levels are necessary to ensure the surgery was successful and to check for recurrence.
Parathyroid surgery is generally safe, but like any surgical procedure, it carries some risks:
Common Complications:
-
Infection: Infections can occur at the incision site.
-
Bleeding or Hematoma: Accumulation of blood in the surgical area.
-
Hypocalcemia (Low Calcium): Occurs if too much parathyroid tissue is removed, causing calcium levels to drop.
-
Nerve Injury: Injury to the recurrent laryngeal nerve can cause hoarseness or difficulty speaking.
-
Scarring: Though rare with minimally invasive surgery, scarring may occur.
Most complications are rare and can be managed effectively with early intervention.
After parathyroid surgery, most patients experience significant improvement in their symptoms, including reduced fatigue, improved bone health, and better overall well-being. However, ongoing management is necessary to ensure long-term success.
Recovery Timeline:
-
First Few Days: Most patients are able to go home the same day or within 24 hours after surgery.
-
First Month: It’s important to monitor calcium levels and avoid strenuous activities during this time.
-
3-6 Months: Full recovery is typically achieved, with most patients returning to their normal activities.
Long-Term Considerations:
-
Regular Follow-Up: Bone Health: Regular check-ups to assess bone density and calcium levels.
-
Lifestyle Modifications: Maintaining a balanced diet, staying physically active, and managing weight can all contribute to sustained health post-surgery.
1. What is Parathyroid Surgery?
Parathyroid surgery is a procedure performed to remove one or more of the parathyroid glands. These glands are located near the thyroid and are responsible for producing parathyroid hormone (PTH), which helps regulate calcium levels in the body. Surgery is typically recommended for conditions such as primary hyperparathyroidism, where the parathyroid glands produce too much PTH, leading to high calcium levels and various health problems.
2. Why is Parathyroid Surgery necessary?
Parathyroid surgery is necessary when a patient has an overactive parathyroid gland, a condition known as hyperparathyroidism. This can result from benign tumors (adenomas), hyperplasia (enlargement), or rarely, cancer. The surgery helps restore normal calcium balance and prevent complications such as bone loss, kidney stones, fatigue, and cognitive issues associated with high calcium levels.
3. How is Parathyroid Surgery performed?
Parathyroid surgery is typically performed under general anesthesia. The surgeon makes a small incision in the neck and carefully locates the parathyroid glands. If a tumor or abnormal gland is found, it is removed. In most cases, only one gland is removed, but if more than one is affected, multiple glands may need to be removed. The surgery usually takes about 1-2 hours, depending on the complexity of the case.
4. What are the risks and complications of Parathyroid Surgery?
While parathyroid surgery is generally safe, potential risks include:
-
Injury to the recurrent laryngeal nerve, which controls the vocal cords
-
Infection at the incision site
-
Bleeding
-
Low calcium levels (hypocalcemia) after surgery, which is temporary in most cases
-
Scar formation
-
Anesthesia-related risks
However, these complications are rare, and most patients experience a smooth recovery.
5. How long does it take to recover from Parathyroid Surgery?
Recovery from parathyroid surgery is relatively quick. Most patients can go home on the same day or the following day after surgery. The initial recovery period lasts about 1 to 2 weeks, during which patients are advised to avoid strenuous activities. Full recovery, including resuming normal activities, typically takes 4 to 6 weeks.
6. Will I experience pain after Parathyroid Surgery?
Post-surgical pain is usually minimal and well-managed with medication. Some patients experience a sore throat or mild discomfort at the incision site. Any discomfort is typically short-lived and can be alleviated with over-the-counter pain relievers or prescribed medication from the surgeon.
7. How will my calcium levels be managed after Parathyroid Surgery?
After parathyroid surgery, calcium levels are closely monitored. In most cases, calcium levels return to normal within a few days to weeks following surgery. Some patients may temporarily experience low calcium levels (hypocalcemia), which is managed with calcium supplements until the body adjusts. Your doctor will guide you through any necessary calcium management post-surgery.
8. What are the benefits of Parathyroid Surgery?
The primary benefit of parathyroid surgery is the relief from symptoms caused by high calcium levels, including fatigue, bone pain, kidney stones, and cognitive issues. Most patients experience a significant improvement in their symptoms after surgery, along with a return to normal calcium balance, reducing the risk of future complications.
9. Are there alternatives to Parathyroid Surgery?
For patients with mild hyperparathyroidism or those who are not good candidates for surgery, non-surgical options may be considered. These can include monitoring calcium levels regularly, lifestyle changes, and medications to manage calcium levels. However, surgery remains the most effective long-term solution for symptomatic hyperparathyroidism, especially when a tumor or other abnormalities are present.
10. What should I expect during the hospital stay after Parathyroid Surgery?
Most patients stay in the hospital for a day or two after parathyroid surgery. During this time, the medical team will monitor your vital signs, manage pain, and check your calcium levels. You will be given instructions on how to care for your incision, activity restrictions, and follow-up appointments. By the time you leave the hospital, you will have a clear plan for your recovery.
The other Neurology Procedures are:
Few Major Hospitals for Parathyroid Surgery are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.