Peripheral nerve surgery is a medical intervention aimed at addressing injuries, diseases, or disorders that affect the peripheral nervous system, which includes all nerves outside the brain and spinal cord. These nerves are responsible for transmitting signals between the central nervous system (CNS) and the limbs, organs, and other parts of the body, allowing for movement, sensation, and autonomic functions like breathing and heartbeat regulation.
Peripheral nerve disorders can significantly impair motor function, sensation, and overall quality of life. Common conditions that require peripheral nerve surgery include nerve compression, trauma, neuropathy, and tumors. Depending on the type of damage, peripheral nerve surgery may involve repairing nerve injuries, decompressing nerves, or removing tumors affecting nerve function.
Peripheral nerve surgery is critical for treating conditions such as carpal tunnel syndrome, sciatica, nerve injuries, neuropathies, and nerve tumors. In this guide, we will explore the causes, symptoms, diagnosis, treatment options, and the process of recovery from peripheral nerve surgery, providing valuable insights for patients considering surgical intervention.
Causes of Peripheral Nerve Disorders
Peripheral nerve damage can result from various causes, ranging from acute injuries to chronic conditions. Understanding these causes can help in both the prevention and treatment of nerve disorders requiring surgery.
-
Trauma and Injury:
-
Physical Injuries: Traumatic events such as car accidents, sports injuries, or falls can directly damage the peripheral nerves. Fractures, cuts, or blunt force trauma can sever or compress nerves, leading to symptoms like numbness, pain, and muscle weakness.
-
Surgical Complications: Sometimes, surgical procedures involving the spine or neck can inadvertently affect nearby nerves. Spinal surgeries, for example, may result in nerve damage if not properly handled.
-
-
Compression and Entrapment:
-
Nerve Compression Syndromes: When a nerve is compressed by surrounding tissues like muscles, bones, or ligaments, it can lead to impaired nerve function. Common examples include:
-
Carpal Tunnel Syndrome: Compression of the median nerve at the wrist.
-
Cubital Tunnel Syndrome: Compression of the ulnar nerve at the elbow.
-
Thoracic Outlet Syndrome: Compression of nerves and blood vessels between the neck and shoulder.
-
Radiculopathy: Compression of nerve roots in the spine, such as in sciatica, where the sciatic nerve is compressed in the lower back.
-
-
-
Systemic Diseases:
-
Diabetic Neuropathy: Chronic high blood sugar levels from diabetes can cause nerve damage, particularly in the legs and feet, leading to pain, tingling, or numbness.
-
Infections: Certain infections, such as shingles (herpes zoster), Lyme disease, and HIV, can affect peripheral nerves, causing pain and sensory disturbances.
-
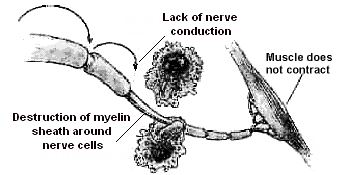
Autoimmune Diseases: Disorders like Guillain-Barré Syndrome or Multiple Sclerosis (MS) can affect the peripheral nervous system by attacking the nerves, leading to weakness, paralysis, and sensory disturbances.
-
-
Tumors:
-
Schwannomas: Tumors that develop from the Schwann cells (cells that form the myelin sheath around nerves). These benign tumors can compress the nerves, causing symptoms of nerve dysfunction.
-
Neurofibromas: Benign tumors that grow on nerve tissue, often associated with neurofibromatosis, a genetic condition that can lead to multiple tumors.
-
-
Genetic Disorders:
-
Charcot-Marie-Tooth Disease (CMT): A hereditary disorder that leads to progressive peripheral nerve damage, affecting muscles in the feet, legs, hands, and arms.
-
Risk Factors for Peripheral Nerve Disorders
While peripheral nerve damage can happen to anyone, several risk factors increase the likelihood of developing nerve conditions requiring surgery.
-
Age: Aging can contribute to degenerative nerve conditions. Peripheral nerve function tends to decline with age, making older adults more vulnerable to nerve damage.
-
Gender: Conditions like carpal tunnel syndrome are more common in women, especially during pregnancy or menopause.
-
Genetics: A family history of neuropathy, neurofibromatosis, or other genetic disorders increases the risk of developing peripheral nerve disorders.
-
Chronic Diseases: Diabetes, rheumatoid arthritis, and kidney disease are known to contribute to nerve damage over time.
-
Lifestyle Factors: Poor nutrition, excessive alcohol use, and smoking can all damage the peripheral nerves. Additionally, repetitive activities and poor ergonomics can increase the risk of nerve compression.
-
Physical Trauma: Direct physical injuries to the peripheral nerves increase the need for surgical intervention.
Peripheral nerve disorders can present a wide range of symptoms, depending on which nerve or nerve group is affected. The most common signs of nerve damage include:
Sensory Symptoms:
-
Numbness or Tingling: Often described as a "pins and needles" sensation, especially in the hands, feet, or legs.
-
Pain: Nerve pain can be sharp, burning, or shooting in nature. Common conditions like sciatica or trigeminal neuralgia can cause intense, shooting pain along the nerve pathway.
-
Loss of Sensation: Complete or partial loss of feeling in the affected area, which may affect the ability to detect hot or cold sensations.
Motor Symptoms:
-
Muscle Weakness: This occurs when nerves that control muscle function are damaged. Symptoms can include difficulty moving a limb or performing tasks that require fine motor control (e.g., buttoning a shirt or gripping objects).
-
Muscle Atrophy: If the nerve remains damaged, muscles may waste away due to lack of use, leading to further weakness.
-
Loss of Coordination: Difficulty walking or maintaining balance, as well as reduced ability to perform tasks requiring coordination (e.g., typing, writing).
Autonomic Symptoms:
-
Sweating Abnormalities: Damage to autonomic nerves may cause either excessive sweating or dry skin.
-
Digestive Issues: Nerve damage can affect the digestive system, leading to symptoms like constipation, bloating, and difficulty swallowing.
Severe Symptoms:
-
Paralysis: In cases of severe nerve damage, loss of motor control can lead to paralysis in the affected limb.
-
Bladder and Bowel Dysfunction: Nerve damage can affect control over bladder or bowel function, especially in cases of spinal cord injuries or severe neuropathy.
Diagnosing peripheral nerve disorders typically involves a comprehensive clinical evaluation, supported by various diagnostic tests to pinpoint the exact cause and severity of nerve damage.
Clinical Evaluation:
-
Patient History: The doctor will gather a detailed history of the patient’s symptoms, including their onset, progression, and severity. Information about trauma, lifestyle, and family history is also crucial.
-
Physical and Neurological Examination: The doctor will perform tests to assess muscle strength, coordination, sensation, and reflexes. The affected nerves are tested to determine the extent of damage.
Diagnostic Tests:
-
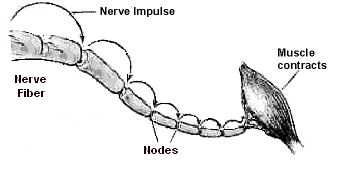
Nerve Conduction Studies (NCS): Measures the electrical impulses in the nerves and assesses their ability to transmit signals. This test helps identify nerve damage or slowing of nerve function.
-
Electromyography (EMG): This test evaluates the electrical activity in muscles to determine whether muscle weakness is due to nerve damage or muscle-related issues.
-
Magnetic Resonance Imaging (MRI): An MRI provides detailed images of soft tissues and nerves, allowing doctors to identify any structural damage, such as compression, tumors, or abnormalities affecting the nerves.
-
Ultrasound: Used to visualize the affected nerve, particularly in cases of entrapment or compression (e.g., carpal tunnel syndrome).
-
Biopsy: In some cases, a biopsy of the nerve may be necessary to confirm the diagnosis, particularly when tumors or neuropathy are suspected.
Genetic Testing:
If a genetic disorder such as Charcot-Marie-Tooth Disease or neurofibromatosis is suspected, genetic testing may be conducted to confirm the diagnosis.
Treatment for peripheral nerve disorders depends on the specific diagnosis, severity, and location of the nerve damage. In cases where conservative treatments (e.g., physical therapy, medications) fail, surgery may be necessary.
Surgical Options:
-
Nerve Decompression Surgery:
-
Carpal Tunnel Release: Involves cutting the ligament that is compressing the median nerve at the wrist, providing relief from carpal tunnel syndrome.
-
Foraminal Decompression: Used in spinal nerve compression, where bone or disc material is removed to free the compressed nerve roots.
-
-
Nerve Repair and Reconstruction:
-
Nerve Grafting: In cases of complete nerve rupture, a nerve graft may be required to reconnect the severed ends.
-
Nerve Transposition: Nerves can be moved from one location to another to avoid compression or injury, especially in cases of thoracic outlet syndrome.
-
-
Tumor Removal:
-
Schwannoma or Neurofibroma Resection: Benign nerve tumors that cause pain or nerve compression may need to be surgically removed.
-
-
Spinal Nerve Surgery:
-
Spinal Nerve Root Resection: In cases where nerve roots are compressed by a herniated disc, part of the nerve root may be removed to relieve pain.
-
-
Peripheral Nerve Stimulation:
-
Nerve Stimulation: Electrical stimulation of the affected nerve may be used to help reduce pain and improve function after surgery.
-
Non-Surgical Options:
-
Physical Therapy: Often prescribed to improve muscle strength, coordination, and flexibility post-surgery.
-
Pain Management: Anti-inflammatory medications, nerve blockers, and topical pain relief may help manage symptoms.
-
Nerve Blocks: Injection of local anesthetics or steroids to reduce inflammation and pain.
Preventing peripheral nerve disorders involves addressing risk factors like diabetes, poor ergonomics, and trauma. After surgery, managing nerve health and preventing future damage is essential for long-term recovery.
Preventive Measures:
-
Proper Ergonomics: Use correct posture and ergonomically designed workstations to avoid nerve compression.
-
Exercise and Stretching: Regular exercise, particularly strengthening and stretching exercises for the back, neck, and hands, can prevent nerve compression.
-
Healthy Lifestyle: Proper nutrition, vitamin intake (especially B12), and avoidance of smoking and excessive alcohol consumption can help prevent nerve damage.
-
Control of Chronic Conditions: Proper management of conditions like diabetes and autoimmune diseases can help reduce the risk of neuropathy.
Post-Surgical Management:
-
Physical Therapy: Essential for recovery, helping to restore function and strength to the affected limb.
-
Ongoing Monitoring: Regular follow-up with a healthcare provider to assess recovery progress and detect any recurrence of symptoms.
-
Pain Management: Depending on the recovery progress, pain medications or nerve-blocking agents may be prescribed.
Although peripheral nerve surgery is generally safe, there are risks associated with any surgical procedure.
-
Nerve Injury: There is a small risk of further nerve damage during surgery.
-
Infection: Like any surgery, there is a risk of infection at the incision site.
-
Scarring: Scarring at the surgery site, particularly with larger incisions.
-
Persistent Symptoms: In some cases, patients may continue to experience symptoms such as pain or weakness, despite surgery.
-
Recurrence: In conditions like carpal tunnel syndrome, nerve compression may recur if not adequately addressed.
After peripheral nerve surgery, patients typically experience significant improvement in their symptoms, but full recovery can take time. The recovery process may involve physical therapy, lifestyle modifications, and ongoing medical care to ensure the best possible outcomes.
Recovery Timeline:
-
Immediate Post-Surgery: Rest and monitoring to ensure no complications arise.
-
1–3 Months: Gradual increase in activity and physical therapy to strengthen muscles and restore function.
-
6 Months: Full recovery, with most patients regaining most or all of their previous function.
Long-Term Considerations:
-
Exercise and Rehabilitation: Staying active with low-impact activities can help maintain nerve health.
-
Avoiding Recurrence: Patients are encouraged to continue with ergonomic practices and manage risk factors to prevent future damage.
1. What is Peripheral Nerve Surgery?
Peripheral nerve surgery is a procedure performed to repair or treat damage to the peripheral nerves, which are the nerves located outside the brain and spinal cord. These nerves are responsible for transmitting signals between the central nervous system and the rest of the body. The surgery aims to repair nerve injuries, release nerve compression, or address conditions such as nerve tumors, nerve entrapments, or neuropathies.
2. Why would I need Peripheral Nerve Surgery?
Peripheral nerve surgery is often needed when there is nerve damage due to trauma, compression, or disease. Common conditions that may require surgery include:
-
Carpal tunnel syndrome (compression of the median nerve in the wrist)
-
Nerve injuries from accidents or trauma
-
Tumors affecting peripheral nerves
-
Peripheral neuropathies (nerve damage due to diabetes, infections, or other causes)
-
Nerve entrapments causing weakness, numbness, or pain
3. How is Peripheral Nerve Surgery performed?
Peripheral nerve surgery is typically performed under local or general anesthesia, depending on the location and extent of the surgery. The surgeon makes an incision near the affected nerve, identifies the damaged nerve, and either removes the damaged tissue, releases nerve compression, or repairs the nerve using sutures or grafts. In cases of nerve injury, nerve grafts may be taken from another part of the body to help restore function.
4. What are the risks and complications of Peripheral Nerve Surgery?
As with any surgery, peripheral nerve surgery carries some risks. Potential complications include:
-
Infection at the incision site
-
Nerve damage or incomplete repair
-
Scarring or stiffness
-
Persistent pain or numbness
-
Blood clots or bleeding
However, these complications are rare, and most patients experience good recovery with proper care.
5. How long does it take to recover from Peripheral Nerve Surgery?
The recovery time after peripheral nerve surgery depends on the severity of the nerve damage and the type of procedure performed. In general, initial recovery takes a few weeks, during which you may need to rest and avoid heavy lifting. Full recovery, including regaining nerve function and strength, can take several months. Physical therapy is often recommended to help restore movement and function.
6. Will I experience pain after Peripheral Nerve Surgery?
It is normal to experience some pain or discomfort after peripheral nerve surgery, especially during the initial recovery phase. However, the pain is usually well-controlled with pain medications and should subside as healing progresses. Some patients may experience numbness or tingling, but these symptoms typically improve over time as the nerve heals.
7. What can I do to speed up my recovery after Peripheral Nerve Surgery?
To speed up your recovery, it is important to follow your surgeon’s post-operative care instructions. These may include:
-
Taking prescribed medications as directed
-
Attending physical therapy sessions to regain strength and mobility
-
Avoiding activities that could strain the surgical site
-
Keeping the surgical area clean and dry
-
Gradually increasing activity as recommended by your surgeon
8. Can Peripheral Nerve Surgery restore full function?
In many cases, peripheral nerve surgery can restore significant function and relieve symptoms such as pain, weakness, or numbness. However, the extent of recovery depends on several factors, including the severity of the nerve damage, how soon the surgery was performed after injury, and the type of nerve involved. While many patients experience full or partial recovery, some may have lingering symptoms.
9. Is Peripheral Nerve Surgery always necessary?
Peripheral nerve surgery is typically considered when non-surgical treatments, such as physical therapy, medication, or lifestyle changes, have not provided sufficient relief. In some cases, nerve injuries may heal on their own with conservative treatment. However, surgery may be recommended if the nerve is severely compressed, damaged, or if there is a risk of permanent nerve loss.
10. What should I expect during the hospital stay after Peripheral Nerve Surgery?
After peripheral nerve surgery, you may need to stay in the hospital for a short period, typically 1-2 days, depending on the complexity of the surgery. During your hospital stay, the medical team will monitor your vital signs, manage pain, and check for any signs of complications. You will be given instructions on how to care for your incision, when to resume normal activities, and follow-up appointments for further evaluation.
The other Neurology Procedures are:
Few Major Hospitals for Peripheral Nerve Surgery are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.