Vasectomy reversal is a surgical procedure performed to restore fertility in men who have previously undergone a vasectomy, a procedure that is typically done as a permanent form of male contraception. During a vasectomy, the vas deferens, the tubes that carry sperm from the testicles to the urethra, are cut or blocked to prevent sperm from entering the semen. While vasectomy is considered a permanent method of contraception, some men may later desire to father children and seek a Vasectomy reversal.
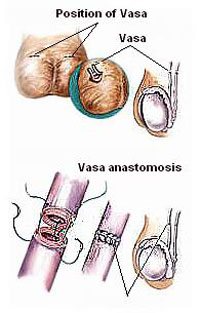
The goal of Vasectomy reversal is to reconnect the vas deferens, allowing sperm to once again be included in the semen. There are two primary types of Vasectomy reversal procedures: vasovasostomy, where the two ends of the vas deferens are directly reconnected, and vasoepididymostomy, which is performed when there is a blockage in the epididymis (the tube where sperm is stored) and involves connecting the vas deferens to the epididymis.
The procedure is typically performed under general anesthesia or spinal anesthesia and involves small incisions in the scrotum. The surgeon carefully identifies and reconnects the vas deferens, using microsurgical techniques to minimize tissue damage and improve the chances of successful sperm flow restoration. The procedure is highly specialized and requires a skilled microsurgeon to ensure the best outcomes.
Vasectomy reversal can be successful in restoring sperm flow, but the chances of regaining fertility depend on several factors, including how much time has passed since the original vasectomy, the method used during the initial procedure, and the age and health of the man and his partner. Generally, the success rate of Vasectomy reversal is higher when the procedure is performed within 10 years of the vasectomy, but successful pregnancies can still occur even after longer periods.
While Vasectomy reversal offers a chance at restored fertility, it does not guarantee that the couple will conceive, as other factors, such as female fertility, may also play a role. In some cases, assisted reproductive technologies, like in vitro fertilization (IVF), may be recommended if the reversal does not result in pregnancy.
Overall, vasectomy reversal provides an option for men who regret their decision for permanent contraception and wish to restore their ability to father children. However, it is important to have realistic expectations and discuss the procedure thoroughly with a urologist to understand the potential risks, success rates, and recovery process.
The primary reason men seek vasectomy reversal is a change in their reproductive plans. However, several factors may contribute to the desire for a vasectomy reversal, and understanding the causes and risk factors can help in the decision-making process.
1. Change in Relationship Status
A man who has undergone a vasectomy may later enter into a new relationship where the desire to have children arises. Whether due to remarriage or a desire to expand the family, men may opt for a vasectomy reversal if they wish to have biological children with a new partner.
2. Regret of Permanent Contraception
Some men experience regret after undergoing a vasectomy, particularly if their family size was completed prematurely. In these cases, men may seek a reversal procedure in order to preserve their options for future fertility.
3. Medical Conditions
In rare cases, some medical conditions or complications following a vasectomy, such as sperm granulomas or infection, can contribute to the decision for a reversal. These conditions may lead to concerns about long-term fertility or discomfort.
4. Female Partner's Desire for Biological Children
In cases where a woman, who is in a relationship with a man who has had a vasectomy, desires children, a vasectomy reversal may be considered to help fulfill her reproductive goals.
Typically, there are no "symptoms" associated with a need for a vasectomy reversal. However, the most common signs indicating a desire for reversal typically arise from changes in family planning or partner preferences:
1. Desire for Fertility
The most common sign is the desire to have children after previously choosing permanent contraception. If a man has had a vasectomy and now wishes to father a child, the option of a vasectomy reversal becomes a consideration.
2. Change in Relationship Goals
A change in relationship status, such as remarriage or new partnership, may bring about a desire for biological children, prompting a man to consider a reversal.
3. Regret and Emotional Consideration
Some men may experience emotional or psychological regret over their decision to undergo a vasectomy. The desire to reverse the procedure and regain fertility is often rooted in these feelings.
Before undergoing vasectomy reversal, it is important for men to undergo a thorough evaluation to ensure the procedure's success. The following diagnostic steps are involved in preparing for a vasectomy reversal:
1. Medical History and Physical Examination
The doctor will start by gathering the patient’s medical history, including details about the vasectomy procedure, any prior health concerns, and fertility history. A physical examination of the genital area will also be performed to assess the condition of the scrotum, testicles, and vas deferens.
2. Semen Analysis
One of the first diagnostic tests is a semen analysis, which evaluates sperm count, quality, and motility. This test will help assess whether sperm is still present in the semen after the vasectomy and if the patient has normal sperm production. If no sperm is present in the semen, a procedure known as sperm retrieval may be necessary for assisted reproductive treatments.
3. Ultrasound of the Scrotum
An ultrasound of the scrotum may be performed to check for any structural issues or complications related to the vasectomy site, such as blocked or dilated tubes.
4. Vasography
A vasography (X-ray of the vas deferens) is a procedure used to evaluate the presence of any blockages in the vas deferens and to assess whether the tube is suitable for reconnection during the reversal procedure.
5. Hormonal Tests
Hormonal tests may be performed to assess testosterone levels and to ensure there is no underlying hormonal imbalance that could affect sperm production.
The treatment for restoring fertility after a vasectomy involves the surgical procedure of vasectomy reversal, which can be performed in different methods:
1. Microsurgical Vasovasostomy
This is the most common and preferred technique. During vasovasostomy, the surgeon uses a microscope to reconnect the two ends of the vas deferens. The procedure is done through a small incision and is highly effective when the vas deferens are intact and sperm can flow through.
2. Microsurgical Vasoepididymostomy
If the vas deferens is blocked, or if sperm cannot be found in the semen, a vasoepididymostomy may be performed. This procedure involves connecting the vas deferens directly to the epididymis (the tube behind the testicle where sperm mature). This procedure is more complex than the vasovasostomy and is typically used when the vas deferens is blocked or damaged beyond repair.
3. Sperm Retrieval and IVF/ICSI
In some cases, if the vasectomy reversal is not successful or if sperm cannot be found in the semen, sperm may be retrieved directly from the testicle using a procedure called testicular sperm extraction (TESE). The sperm can then be used in assisted reproductive techniques such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
There are no guaranteed ways to prevent the need for a vasectomy reversal, but the following can help manage the process effectively:
1. Consult a Fertility Specialist
Before undergoing a vasectomy, it is essential for men to discuss potential future fertility goals with a fertility specialist to fully understand the consequences of the procedure. Some men may choose to store sperm in a sperm bank for future use.
2. Follow Post-Surgical Instructions
After undergoing vasectomy reversal, it is important to follow post-surgical care instructions, including rest, wearing supportive underwear, and avoiding strenuous activity to allow for optimal healing and reduce complications.
3. Monitor Recovery and Follow-up Care
Regular follow-up appointments with the surgeon will help monitor the success of the procedure, evaluate sperm production, and ensure that healing is progressing properly.
While vasectomy reversal is a generally safe procedure, there are some potential complications to be aware of:
1. Infection
As with any surgery, there is a risk of infection. Post-operative care and proper hygiene can help minimize this risk.
2. Hematoma or Swelling
Some swelling or a hematoma (blood collection) may occur in the scrotum after surgery. This typically resolves on its own but may require medical attention if severe.
3. Failed Reconnection
In some cases, the vas deferens may not heal properly after the procedure, and the reconnection may fail. This can result in the failure of the procedure to restore fertility.
4. Chronic Pain
Some men may experience chronic testicular or scrotal pain after the procedure, which may require additional treatment.
5. Low Sperm Count
Even after a successful reversal, some men may not regain normal sperm count or quality, affecting fertility.
After a vasectomy reversal, it may take time to determine the success of the procedure. Men undergoing this surgery should be prepared for a recovery period and potential emotional and psychological adjustments:
1. Recovery and Rest
Post-surgery, patients should focus on proper recovery. This includes rest, avoiding heavy lifting, and wearing supportive undergarments to protect the surgical site.
2. Patience in Achieving Fertility
It can take several months to a year to see if sperm production has returned to normal levels, so patience is key. Follow-up sperm analysis will help monitor the recovery of sperm production.
3. Emotional and Psychological Support
The decision to undergo a vasectomy reversal is often influenced by emotional factors, such as the desire for children or relationship changes. Support from a partner, family members, or a counselor can be valuable during this time.
1. What is a vasectomy reversal?
A vasectomy reversal is a surgical procedure that restores the flow of sperm through the vas deferens, which were previously cut or blocked during a vasectomy. The goal of the procedure is to reconnect the tubes and allow sperm to enter the semen again, making it possible for the man to father children naturally.
2. Why would someone choose to have a vasectomy reversal?
A vasectomy reversal is often performed when:
-
The man changes his mind about fathering children after having a vasectomy.
-
Marriage or relationship changes: A man may want to have children with a new partner.
-
Health considerations: Sometimes men want to restore fertility after realizing that they would like more children.
-
Regret: Some men experience regret after their vasectomy and opt for a reversal to restore their fertility.
3. How is a vasectomy reversal performed?
A vasectomy reversal is typically done under general anesthesia or local anesthesia with sedation. The procedure involves:
-
Incisions: The surgeon makes small incisions in the scrotum to access the vas deferens (the tubes that carry sperm from the testicles to the urethra).
-
Reconnection of the vas deferens: The surgeon carefully reconnects the two ends of the vas deferens by stitching them together. In some cases, the surgeon may need to remove any scar tissue.
-
Micro-surgical technique: The use of a microscope allows the surgeon to make precise incisions and connect the tubes accurately, ensuring the highest chances of success.
The surgery typically lasts between 2 to 4 hours depending on the complexity.
4. What are the chances of success with a vasectomy reversal?
The success of a vasectomy reversal depends on several factors:
-
Time since the vasectomy: The chances of success are generally higher if the vasectomy was performed within 10 years. After 15 or more years, the likelihood of success decreases, though some men still achieve successful reversals.
-
Age of the woman: The age of the woman and her fertility health can also impact the success of the reversal.
-
Surgeon’s experience: The skill and experience of the surgeon performing the procedure play a significant role in the success rate.
-
Type of vasectomy performed: The technique used in the original vasectomy may affect the reversal’s success.
On average, success rates for vasectomy reversals are around 70% to 90% in terms of sperm returning to the semen, with 40% to 60% of couples achieving a pregnancy within 2 years following the procedure.
5. Is vasectomy reversal painful?
Vasectomy reversal is typically not very painful, especially since the procedure is done under anesthesia. After surgery, mild discomfort or soreness in the scrotal area is common and can be managed with over-the-counter pain medications. Swelling and bruising may also occur but usually resolve within a week or two. Most men are able to return to normal activities within 1 to 2 weeks, although heavy physical activities should be avoided for about 4 to 6 weeks.
6. What are the risks and complications of vasectomy reversal?
As with any surgical procedure, vasectomy reversal carries some risks, including:
-
Infection: Infection at the incision site or within the scrotum.
-
Bleeding or hematoma: Swelling or blood collection in the scrotum, which can cause discomfort.
-
Scar tissue formation: Scarring inside the scrotum may affect the success of the surgery or future sperm flow.
-
Failure of the reversal: In some cases, the reconnection of the vas deferens may not work, and sperm may not return to the semen.
-
Chronic pain: Some men may experience ongoing scrotal pain after the procedure.
-
Epididymitis: Swelling of the epididymis (the tube that stores sperm) due to irritation or infection.
It’s important to discuss these risks with your surgeon before deciding on the procedure.
7. How soon after the vasectomy reversal can I expect to see sperm in my semen?
After a vasectomy reversal, it can take some time for sperm to return to the semen. In most cases, sperm can be found in the semen within 3 to 6 months after surgery, although it may take longer. In some cases, men may need to undergo follow-up procedures or sperm retrieval techniques if sperm do not appear after the reversal. Regular semen analysis will be conducted by your doctor to monitor the progress.
8. How long will it take to recover from a vasectomy reversal?
The initial recovery from a vasectomy reversal typically takes 1 to 2 weeks, during which time the patient should avoid strenuous physical activity, heavy lifting, and sexual intercourse. Most men can return to work within 3 to 7 days, though they should avoid activities that put strain on the surgical site. Full recovery, including the resumption of normal activities, generally occurs within 4 to 6 weeks.
9. How much does a vasectomy reversal cost?
The cost of a vasectomy reversal varies widely based on factors such as location, the experience of the surgeon, and whether the procedure is performed in a hospital or an outpatient surgical center. On average, the procedure can cost anywhere from $5,000 to $15,000. This cost typically includes the surgeon’s fees, anesthesia, facility charges, and follow-up care. Health insurance usually does not cover the cost of vasectomy reversal as it is considered an elective procedure.
10. Is there a guarantee that I will get my partner pregnant after vasectomy reversal?
There is no guarantee that a vasectomy reversal will result in pregnancy, even if sperm is found in the semen after the procedure. Several factors can influence the chances of pregnancy, including:
-
Sperm quality: Even if sperm is present, its quality and ability to fertilize an egg may be impacted by age, health, or previous injury to the vas deferens.
-
Female fertility: The fertility of the woman and her reproductive health also play a significant role.
-
Timing: It may take several attempts at conception before pregnancy occurs, and assisted reproductive techniques (ART) like in vitro fertilization (IVF) may be recommended if natural conception does not happen.
The success of a vasectomy reversal depends on many variables, but many couples are able to conceive naturally within 1 to 2 years following the procedure.
The other Urology Procedures are:
Few Major Hospitals for Vasectomy Reversal are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Vasectomy Reversal | Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


