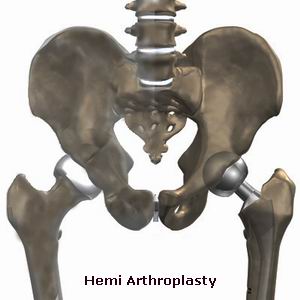
Hemi-arthroplasty, also known as partial joint replacement, is a surgical procedure that involves replacing part of a joint, typically the ball (femoral head) of the hip or humeral head of the shoulder, with an artificial component, while preserving the other part of the joint (i.e., the socket). This procedure is commonly performed for patients who have severe arthritis, fractures, or degenerative conditions that affect a specific part of the joint but leave the other part of the joint relatively intact.
Hemi-arthroplasty is generally recommended for individuals who have damage to one side of the joint but not the other. For example, in the case of the hip joint, if the femoral head (ball) is severely damaged due to arthritis or fracture, but the acetabulum (socket) remains intact, hemi-arthroplasty can restore function and alleviate pain. Hemi-arthroplasty is commonly performed in the hip and shoulder joints, though it can be done in other joints as well.
The procedure involves removing the damaged part of the joint and replacing it with a prosthetic component. Unlike total joint replacement, where both the ball and socket are replaced, hemi-arthroplasty preserves the uninjured portion of the joint. This procedure can provide significant pain relief, restore function, and improve mobility, particularly for individuals who are not candidates for total joint replacement due to other health conditions or age.
Hemi-arthroplasty is typically indicated in patients who have joint damage that affects only one part of the joint. The most common causes and risk factors leading to the need for hemi-arthroplasty include:
1. Osteoarthritis (OA)
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, swelling, and loss of motion. In cases of hip osteoarthritis, the femoral head can become damaged, while the acetabulum remains relatively unaffected. Similarly, shoulder osteoarthritis can affect the humeral head without significant damage to the glenoid (socket). When one part of the joint becomes severely damaged, hemi-arthroplasty can be an effective option.
2. Hip Fractures
In older adults, hip fractures often occur due to osteoporosis or falls. A fracture in the femoral head may necessitate hemi-arthroplasty, especially when the bone is not suitable for fixation. In these cases, replacing the femoral head with a prosthesis can restore mobility and alleviate pain while preserving the acetabulum.
3. Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune condition that causes inflammation in the joints, leading to joint destruction and deformities. RA can affect various joints, including the hip and shoulder, leading to partial damage. Hemi-arthroplasty may be performed if only one part of the joint is affected, while the other part remains intact.
4. Avascular Necrosis (AVN)
Avascular necrosis (AVN) is a condition in which the blood supply to the bone is disrupted, leading to bone death and collapse. In the hip joint, AVN typically affects the femoral head, causing pain and limiting motion. If the femoral head is severely damaged but the acetabulum is intact, hemi-arthroplasty can help restore function and alleviate pain.
5. Previous Joint Injury or Trauma
Joint injuries, such as fractures, dislocations, or severe ligament damage, can lead to long-term damage in the affected joint. In cases where a single part of the joint is damaged due to trauma, hemi-arthroplasty may be performed to replace the damaged portion, particularly in the hip or shoulder.
6. Age and Activity Level
Hemi-arthroplasty is often recommended for younger patients or those with specific joint damage who do not need full joint replacement. For example, in younger, active individuals, replacing only the femoral head (hip) or humeral head (shoulder) can offer significant relief, allowing them to return to normal activities without the need for full joint replacement.
The symptoms and signs that may indicate the need for hemi-arthroplasty typically involve pain, stiffness, and decreased function in the affected joint. These symptoms can interfere with daily activities, such as walking, lifting, or reaching overhead. Common symptoms include:
1. Chronic Joint Pain
Persistent pain is the most common sign that a joint may require hemi-arthroplasty. In cases of osteoarthritis, fractures, or AVN, the joint pain may be constant and worsen with activity. In hip osteoarthritis, the pain may be felt in the groin, thigh, or buttocks, while shoulder pain is often felt in the upper arm or around the shoulder blade.
2. Stiffness and Limited Range of Motion
As joint damage progresses, the ability to move the joint may become restricted. Stiffness in the hip or shoulder joint can make it difficult to perform simple tasks such as sitting down, standing up, reaching overhead, or getting dressed.
3. Weakness in the Joint
Damage to the joint structures, including the muscles and ligaments, can cause weakness and difficulty in supporting the body weight or moving the joint properly. In the hip, this may result in difficulty walking or standing for long periods, while in the shoulder, weakness can affect the ability to lift objects.
4. Swelling and Tenderness
Joint inflammation, which occurs in conditions like rheumatoid arthritis or following a joint fracture, can lead to swelling and tenderness around the joint. This may be associated with increased pain, especially after prolonged activity.
5. Instability or Feeling of "Giving Way"
In some cases, a joint that is damaged may feel unstable, causing the patient to feel like the joint might "give way" under pressure. This sensation can occur in the hip and shoulder when the ball-and-socket joint is no longer functioning properly due to damage to one of its components.
The diagnosis of a joint condition requiring hemi-arthroplasty involves a comprehensive evaluation, including a detailed medical history, physical examination, and imaging studies. Common diagnostic steps include:
1. Medical History and Physical Examination
The physician will begin by asking about the patient’s symptoms, such as the onset and duration of pain, limitations in mobility, previous injuries, or any other underlying health conditions like arthritis or osteoporosis. A physical examination will be conducted to assess the joint's range of motion, strength, and stability. The doctor will also check for signs of swelling, tenderness, or deformity.
2. X-rays
X-rays are used to visualize the bones and joint space of the affected area. They can show signs of joint degeneration, bone fractures, or abnormalities in the joint structure. In cases of hip arthritis or fractures, X-rays can help determine the extent of the damage and guide treatment decisions.
3. MRI (Magnetic Resonance Imaging)
MRI is often used to obtain more detailed images of soft tissues, such as cartilage, ligaments, and muscles, that may be affected by injury or disease. MRI can be particularly useful for diagnosing rotator cuff tears in the shoulder or identifying cartilage damage in the hip joint.
4. CT Scan
In some cases, a CT scan may be used to evaluate the bones and joints in greater detail, especially if fractures or structural abnormalities are suspected. CT scans are often used in preoperative planning to assess the alignment and condition of the bones.
Treatment for conditions requiring hemi-arthroplasty usually begins with conservative measures, but when these are insufficient, surgery is considered. Treatment options include:
1. Conservative Treatment
Before surgery, doctors typically recommend non-surgical treatments to manage symptoms:
-
Physical Therapy: Strengthening exercises and stretching techniques can improve joint function, increase range of motion, and alleviate pain.
-
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications such as ibuprofen can help reduce pain and inflammation in the joint.
-
Corticosteroid Injections: Injections of corticosteroids into the joint may provide temporary relief from pain and inflammation.
-
Joint Support Devices: Braces or orthotic devices may be used to provide additional support to the joint and reduce strain during movement.
2. Hemi-Arthroplasty Surgery
When conservative treatments fail, hemi-arthroplasty may be recommended. During surgery, the damaged portion of the joint is removed and replaced with an artificial prosthetic component. Depending on the joint, the surgeon may perform the procedure through:
-
Anterior Approach: The most common approach for hip hemi-arthroplasty, performed through the front of the hip.
-
Posterior Approach: Used for shoulder hemi-arthroplasty, where the surgeon accesses the joint from the back.
3. Post-Surgery Rehabilitation
Rehabilitation after hemi-arthroplasty is crucial for restoring strength, mobility, and function to the joint. This typically includes physical therapy and exercises designed to strengthen the muscles around the joint, improve range of motion, and reduce stiffness. Post-operative care and rehabilitation may last several weeks or months, depending on the individual’s healing progress.
While some joint conditions may be inevitable, especially due to age or trauma, certain measures can help reduce the risk of developing conditions that may require hemi-arthroplasty:
1. Regular Exercise
Engaging in regular, low-impact exercise such as swimming or walking can help maintain joint flexibility and strengthen the muscles surrounding the joint. Exercise also helps maintain a healthy weight, reducing stress on weight-bearing joints like the hip and knee.
2. Weight Management
Maintaining a healthy weight can reduce excess pressure on the joints and lower the risk of developing osteoarthritis and other joint conditions. Weight management can be achieved through a combination of proper diet and regular physical activity.
3. Avoiding High-Impact Activities
Activities that place significant strain on the joints, such as running or jumping, can increase the risk of joint wear and tear. If you have an existing joint condition, it is important to modify activities that exacerbate symptoms.
4. Joint Protection
Using joint protection techniques, such as avoiding repetitive movements, using assistive devices, or wearing protective gear, can help prevent further joint injury and degeneration.
While hemi-arthroplasty is generally safe, there are potential risks and complications associated with the surgery:
1. Infection
Infection at the surgical site is a potential risk following any surgery. Antibiotics are prescribed before, during, and after surgery to reduce the risk of infection.
2. Nerve or Blood Vessel Damage
During surgery, there is a risk of damage to nearby nerves or blood vessels, which can cause numbness, weakness, or circulation problems.
3. Prosthesis Failure
Over time, the artificial component of the joint may wear out, loosen, or break, requiring revision surgery to replace the prosthetic component.
4. Blood Clots
Blood clots (deep vein thrombosis) can form in the legs after surgery. Early mobilization and the use of compression stockings or blood thinners can help prevent this complication.
After undergoing hemi-arthroplasty, many patients experience significant improvements in pain relief and function. However, recovery and long-term care are essential for optimal results:
1. Post-Surgery Rehabilitation
Adhering to a rehabilitation program, including physical therapy, is critical for a successful recovery. It helps restore strength, mobility, and range of motion to the joint.
2. Activity Modification
While most patients can return to normal activities after surgery, high-impact or strenuous activities should be avoided to prevent stress on the artificial joint.
3. Regular Check-Ups
Follow-up appointments with the orthopedic surgeon are essential for monitoring the condition of the joint and ensuring that the prosthesis remains in good working order.
1. What is hemi-arthroplasty?
Hemi-arthroplasty is a type of joint replacement surgery where only one part of the joint is replaced, typically the ball (the femoral head) of the hip or shoulder joint, while the socket (acetabulum or glenoid) is left intact. This procedure is often used for patients with joint fractures, arthritis, or other conditions where only one part of the joint is damaged. Hemi-arthroplasty helps relieve pain, restore joint function, and improve mobility.
2. Why is hemi-arthroplasty performed?
Hemi-arthroplasty is commonly performed when:
-
Osteoarthritis or rheumatoid arthritis causes severe pain and dysfunction in one part of the joint.
-
Fractures: It is often used for fractures of the femoral head in the hip or the ball of the shoulder joint.
-
Avascular necrosis: A condition where blood flow to the bone is disrupted, leading to bone death and collapse.
-
Degenerative joint diseases: When only one part of the joint is severely damaged, hemi-arthroplasty may provide a solution without the need for a total joint replacement.
It is typically considered for younger patients or those with significant damage to only one side of the joint.
3. How is hemi-arthroplasty performed?
Hemi-arthroplasty is typically performed under general anesthesia. The procedure involves:
-
Incision: The surgeon makes an incision to access the joint.
-
Removal of the damaged part: The damaged femoral head (in the hip) or the ball of the shoulder joint is removed.
-
Implantation of the prosthesis: A metal or ceramic prosthetic ball is placed in the femoral socket (in the hip) or the humeral head (in the shoulder). The socket of the joint may remain intact.
-
Stabilization: The joint is stabilized with the prosthetic part, and the incision is closed with sutures or staples.
The procedure usually takes 1 to 2 hours, depending on the complexity and the joint being treated.
4. Is hemi-arthroplasty painful?
Hemi-arthroplasty is typically performed under anesthesia, so there is no pain during the surgery itself. After surgery, some pain, swelling, and discomfort are expected as the body heals. Pain is generally manageable with medications, ice therapy, and rest. Most patients experience significant pain relief after the initial recovery period, particularly if the surgery was performed to treat joint degeneration or fractures.
5. How long does it take to recover from hemi-arthroplasty?
Recovery from hemi-arthroplasty can vary based on the type of joint involved and the patient’s overall health, but generally:
-
Hospital stay: Patients typically stay in the hospital for 1 to 3 days after surgery.
-
First few weeks: A period of rest and restricted movement is usually required. You may need crutches or a walker, especially in the first few days or weeks.
-
Physical therapy: Physical therapy usually begins soon after surgery to restore strength, flexibility, and mobility.
-
Full recovery: Most patients can return to light daily activities within 6 to 8 weeks, while more strenuous activities may take 3 to 6 months to resume.
Complete recovery may take up to 6 months, depending on the patient’s healing and the type of joint replaced.
6. What are the risks and complications of hemi-arthroplasty?
Like any surgery, hemi-arthroplasty carries some risks, including:
-
Infection: There is a risk of infection at the incision site or within the joint.
-
Blood clots: Post-operative blood clots, particularly in the legs (deep vein thrombosis), can develop.
-
Dislocation: The prosthetic joint may become dislocated, particularly in the early stages of recovery.
-
Implant loosening: Over time, the implant may become loose or wear out, requiring revision surgery.
-
Nerve or blood vessel damage: There is a small risk of injury to surrounding nerves or blood vessels during surgery.
-
Joint stiffness: Some patients may experience reduced mobility or stiffness in the joint after surgery.
However, the overall success rate for hemi-arthroplasty is high, and complications are rare.
7. How long will the hemi-arthroplasty prosthesis last?
The lifespan of a hemi-arthroplasty prosthesis can vary based on the patient’s age, activity level, and overall health. On average, the implant can last 10 to 15 years. However, more active individuals or younger patients may experience wear and tear on the implant sooner, while older patients or those with lower activity levels may experience longer-lasting results. If the implant wears out or loosens, a revision surgery may be required.
8. What is the difference between hemi-arthroplasty and total joint replacement?
The primary difference between hemi-arthroplasty and total joint replacement is the amount of the joint that is replaced:
-
Hemi-arthroplasty: Only one part of the joint (usually the femoral head in the hip or the humeral head in the shoulder) is replaced, and the socket remains intact.
-
Total joint replacement: Both the ball (femoral head in the hip or humeral head in the shoulder) and the socket (acetabulum in the hip or glenoid in the shoulder) are replaced with prosthetic components.
Hemi-arthroplasty is typically considered when only one part of the joint is damaged, whereas total joint replacement may be necessary when both the ball and socket are severely affected.
9. Will I need physical therapy after hemi-arthroplasty?
Yes, physical therapy is an essential part of the recovery process after hemi-arthroplasty. Rehabilitation focuses on:
-
Restoring range of motion: Exercises will help improve flexibility and prevent stiffness in the joint.
-
Strengthening muscles: Strengthening the muscles around the joint helps improve stability and function.
-
Improving function: Gradual progression of exercises to help the patient return to normal daily activities, including walking and lifting.
A structured rehabilitation program is key to achieving the best possible outcomes after surgery.
10. Can hemi-arthroplasty be prevented or avoided?
While not all conditions requiring hemi-arthroplasty can be prevented, certain steps can help reduce the risk of joint damage:
-
Maintain a healthy weight: Excess weight puts added stress on the joints, especially the hip and shoulder.
-
Exercise regularly: Strengthening the muscles around the joint can provide better support and reduce wear on the joint.
-
Protect the joint from injury: Use proper techniques during physical activity to avoid injury or excessive strain on the joints.
-
Early treatment of joint pain: Seeking medical attention early for joint pain or discomfort can help prevent the progression of joint damage and delay the need for surgery.
The other Orthopedic Procedures are:
Few Major Hospitals for Hemiarthroplasty are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


