
Spine fusion, also known as spinal fusion surgery, is a procedure in which two or more bones in the spine (vertebrae) are permanently joined together to eliminate motion between them. This procedure is commonly performed to stabilize the spine, alleviate pain, and correct deformities caused by conditions like degenerative disc disease, scoliosis, spinal stenosis, or spinal fractures.
The spine is made up of a series of bones called vertebrae, which are separated by discs that allow the spine to bend and move. When a person experiences a problem such as a herniated disc, disc degeneration, or other spinal abnormalities, movement between specific vertebrae may cause discomfort or further complications. Spine fusion eliminates this motion by fusing two or more vertebrae together using various techniques.
The goal of spine fusion surgery is to provide pain relief, restore function, and enhance the patient’s quality of life by promoting the fusion of the vertebrae, which reduces or eliminates painful motion.
Spine fusion is generally recommended for conditions where there is spinal instability, pain, or deformity that doesn't respond to conservative treatments. The causes of spinal problems requiring fusion, as well as risk factors that may lead to the need for surgery, include:
1. Degenerative Disc Disease
Degenerative disc disease occurs as a result of the natural wear and tear of the spinal discs. Over time, these discs lose their ability to cushion the vertebrae, leading to pain, stiffness, and potential instability in the spine. Spine fusion may be needed to stabilize the spine in cases where other treatments have failed.
2. Spinal Fractures
Fractures caused by trauma (such as from a fall, car accident, or sports injury) can destabilize the spine. When fractures affect the vertebrae, it may result in spinal instability or deformity. Spine fusion is often required to stabilize the spine and allow proper healing.
3. Scoliosis and Other Spinal Deformities
Scoliosis, a condition characterized by an abnormal curvature of the spine, may require fusion surgery if the curvature is severe or causing pain or respiratory issues. Similarly, conditions like kyphosis (excessive forward curvature of the spine) may also lead to spine fusion if conservative measures don’t provide relief.
4. Spinal Stenosis
Spinal stenosis refers to the narrowing of the spinal canal, which can cause nerve compression and lead to symptoms such as pain, numbness, or weakness in the legs. In severe cases, spine fusion may be needed to stabilize the spine and prevent further nerve compression.
5. Failed Back Surgery Syndrome (FBSS)
In some cases, spine surgery may not resolve the underlying issue, leading to continued pain. Failed back surgery syndrome refers to persistent pain after spine surgery, and spine fusion may be recommended as a solution to stabilize the spine and address the remaining issues.
6. Risk Factors
-
Age: While spine fusion can be performed at any age, older adults may be at higher risk for complications due to reduced bone density and slower healing times.
-
Obesity: Excess weight can place additional strain on the spine, increasing the risk of disc degeneration and spinal instability.
-
Smoking: Smoking can inhibit healing and reduce the success of the spine fusion procedure.
-
Existing Spine Conditions: People with conditions like spondylolisthesis (slippage of one vertebra over another) or chronic back pain may be at higher risk for needing spine fusion.
-
Previous Spinal Surgeries: If previous spine surgeries have not been successful or led to complications, fusion surgery may be required.
Spine fusion surgery is typically considered when the following symptoms and signs indicate that there is spinal instability, nerve compression, or deformity that cannot be managed through non-surgical methods:
1. Chronic Back or Neck Pain
Persistent and severe back or neck pain that doesn’t respond to medication, physical therapy, or other interventions may indicate the need for spine fusion. Pain caused by degenerated or misaligned discs may be alleviated by eliminating motion between the affected vertebrae.
2. Numbness, Tingling, or Weakness
Compression of the spinal cord or nerves, caused by disc herniation or other conditions, can result in numbness, tingling, or weakness in the arms or legs. If these symptoms are severe and debilitating, spine fusion may be recommended to stabilize the spine and relieve nerve pressure.
3. Difficulty with Movement
If spinal instability causes difficulty with movement, such as walking, bending, or lifting, it may be a sign that spine fusion is necessary to restore stability and function.
4. Progressive Deformity
In cases of spinal deformities such as scoliosis or kyphosis, worsening curvature or deformity may cause significant discomfort, breathing difficulties, or mobility issues. Spine fusion can correct the deformity and prevent further progression.
5. Failed Conservative Treatments
When conservative treatments such as physical therapy, medications, injections, and bracing have failed to provide relief, spine fusion surgery may be considered as a last resort.
The diagnosis of conditions requiring spine fusion involves several key steps:
1. Medical History and Physical Examination
A comprehensive medical history will help the doctor understand the patient’s symptoms, the duration of pain, any previous treatments or surgeries, and the impact of pain on daily activities. The physical exam will include assessing posture, range of motion, and neurological function.
2. Imaging Tests
-
X-rays: X-rays are often the first diagnostic tool used to assess the alignment of the spine and to look for signs of degeneration, fractures, or abnormal curvatures.
-
MRI (Magnetic Resonance Imaging): MRI scans provide detailed images of soft tissues, including discs, nerves, and the spinal cord. This helps doctors assess the severity of any nerve compression, disc degeneration, or abnormalities.
-
CT Scans: A CT scan may be used to provide a more detailed view of the bones and the spinal structures to help diagnose spinal issues that require fusion.
-
Discography: In some cases, discography may be performed to assess whether the intervertebral discs are causing pain.
3. Neurological Evaluation
If nerve damage is suspected, a neurological evaluation may be performed to test for weakness, numbness, tingling, or other symptoms caused by nerve compression or injury.
Once a diagnosis is made, and the need for spine fusion is confirmed, several treatment options exist:
1. Non-Surgical Treatment Options
Before considering spine fusion surgery, several non-surgical treatments may be tried:
-
Medications: Pain relievers, NSAIDs, or stronger narcotics may be prescribed to manage pain. In some cases, muscle relaxants or nerve medications may also help alleviate discomfort.
-
Physical Therapy: A physical therapist may design an exercise regimen to strengthen the back and improve flexibility. This may help reduce pain and improve posture.
-
Bracing: In some cases, wearing a back brace can provide support and alleviate pain by restricting movement, which may help prevent the condition from worsening.
-
Injections: Epidural steroid injections or nerve blocks can reduce inflammation and pain, helping individuals cope with chronic back pain before opting for surgery.
2. Surgical Treatment Options: Spine Fusion
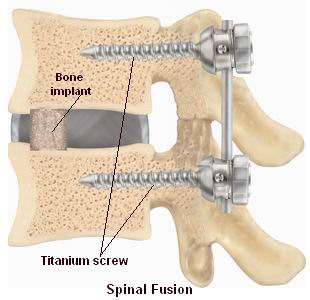
When conservative treatments fail, spine fusion surgery is the primary surgical intervention. The goal of this surgery is to eliminate pain by stabilizing the spine and improving function. Surgical techniques include:
-
Posterior Lumbar Fusion (PLF): A traditional method in which the surgeon approaches the spine from the back, removes any degenerated discs, and fuses the vertebrae together using rods, screws, and bone grafts.
-
Anterior Lumbar Interbody Fusion (ALIF): The surgeon accesses the spine through the abdomen (anterior approach) to remove the damaged disc and insert a bone graft or implant to promote fusion.
-
Transforaminal Lumbar Interbody Fusion (TLIF): A minimally invasive approach where the surgeon accesses the spine from the side to remove the damaged disc and insert a graft to stabilize the spine.
-
Minimally Invasive Spine Fusion: For some patients, a minimally invasive technique may be used, resulting in smaller incisions, reduced pain, and quicker recovery times.
3. Rehabilitation Post-Surgery
After surgery, rehabilitation is a critical part of the recovery process. It may involve physical therapy to regain strength and mobility and to prevent complications such as blood clots or muscle atrophy.
While some spinal conditions cannot be prevented, certain practices can help manage spinal health and reduce the risk of requiring spine fusion:
1. Maintaining a Healthy Weight
Excess weight can place added stress on the spine, contributing to degeneration and discomfort. Maintaining a healthy weight reduces the strain on the lower back and may help prevent spinal issues from progressing.
2. Regular Exercise
Engaging in regular low-impact exercises (like swimming or walking) can help strengthen the muscles supporting the spine. Core-strengthening exercises are especially important for spinal health.
3. Proper Posture
Maintaining good posture, especially while sitting, standing, and lifting, is essential for preventing strain on the spine. Using ergonomic furniture and adjusting the workstation can help avoid unnecessary spinal stress.
4. Smoking Cessation
Smoking can impede the healing process and decrease the success of spine fusion surgeries. Quitting smoking improves overall spinal health and enhances recovery after surgery.
While spine fusion surgery is generally safe, like any surgery, it carries risks and potential complications, including:
1. Infection
Infection at the surgical site or deeper in the spine is a possible complication. Preventive antibiotics are typically given to reduce the risk of infection.
2. Nerve Damage
There is a small risk of nerve injury during spine fusion surgery. If nerve damage occurs, it can result in numbness, tingling, weakness, or even paralysis in severe cases.
3. Blood Clots
Blood clots, particularly in the legs (deep vein thrombosis) or lungs (pulmonary embolism), are common after surgery. Early mobilization and, in some cases, blood thinners are used to prevent clot formation.
4. Hardware Failure
The rods, screws, or plates used in spine fusion surgery may break or loosen over time. If this occurs, additional surgery may be required to replace or adjust the hardware.
5. Non-Union or Pseudoarthrosis
In some cases, the spine may fail to fuse properly, leading to a condition known as pseudoarthrosis. This can result in persistent pain and may require further surgical intervention.
Living with spine fusion surgery requires adaptation, but it also offers significant pain relief and an improved quality of life. The following are key aspects of living with the condition:
1. Post-Operative Recovery
Recovery after spine fusion surgery typically involves a hospital stay of a few days, followed by physical therapy. During the recovery period, patients may need to avoid heavy lifting and high-impact activities to allow the spine to heal.
2. Long-Term Care
Regular follow-up visits with the surgeon are necessary to monitor healing progress and adjust any braces or devices used. Ongoing physical therapy may be necessary to regain strength and flexibility.
3. Lifestyle Adjustments
Lifestyle changes such as avoiding prolonged sitting, maintaining proper posture, and engaging in gentle exercise can significantly improve recovery and long-term outcomes.
1. What is spine fusion surgery?
Spine fusion surgery is a procedure used to permanently join two or more vertebrae in the spine to eliminate motion between them. The goal of the surgery is to stabilize the spine, reduce pain, and prevent further damage caused by conditions such as degenerative disc disease, spinal instability, or fractures. The surgery typically involves the use of bone grafts, which are either taken from the patient’s body or provided by a donor, combined with metal hardware like screws, rods, and plates to hold the vertebrae in place during healing.
2. Why is spine fusion surgery performed?
Spine fusion surgery is performed for a variety of reasons, including:
-
Degenerative disc disease: When the discs between the vertebrae wear out and cause pain.
-
Herniated discs: When the inner portion of a disc bulges out, pressing on nerves and causing pain, numbness, or weakness.
-
Spinal instability: A condition where the vertebrae in the spine no longer provide adequate support and stability.
-
Spinal fractures: Fractures of the spine that may require fusion for healing.
-
Scoliosis or spinal deformities: To correct abnormal spinal curvatures and restore alignment.
The procedure helps alleviate pain and improve spinal function by stabilizing the affected area.
3. How is spine fusion surgery performed?
Spine fusion surgery is typically performed under general anesthesia. The procedure involves the following steps:
-
Incision: A small incision is made near the area of the spine that requires fusion. The surgeon may approach the spine from the back (posterior), side (lateral), or front (anterior), depending on the location and type of fusion.
-
Disc removal: The damaged disc is removed, and any other tissues or bone spurs that may be causing pain or impeding movement are cleared away.
-
Bone graft placement: A bone graft, either from the patient’s own body or a donor, is placed in the empty disc space to promote fusion.
-
Metal hardware placement: Metal screws, rods, and plates are inserted to hold the vertebrae together and support the healing process.
-
Healing: Over time, the vertebrae fuse together, forming a solid bone structure.
The surgery typically lasts between 2 to 4 hours, depending on the complexity of the procedure.
4. What are the benefits of spine fusion surgery?
The primary benefits of spine fusion surgery include:
-
Pain relief: Spine fusion can significantly reduce pain caused by nerve compression, degenerative discs, or spinal instability.
-
Improved mobility: By stabilizing the spine, many patients experience improved function and reduced stiffness.
-
Spinal stability: Fusion prevents the vertebrae from moving abnormally, providing long-term stability to the spine.
-
Prevention of further damage: Spine fusion can help stop the progression of spinal conditions, preventing further deterioration of the vertebrae and discs.
5. What are the risks or complications associated with spine fusion surgery?
As with any surgery, spine fusion has potential risks and complications, including:
-
Infection: There is a risk of infection at the surgical site or deeper within the spine.
-
Nerve damage: Though rare, the surgery could damage nearby nerves, leading to weakness, numbness, or loss of function.
-
Blood clots: Patients may be at risk for blood clots, especially in the legs.
-
Non-union: In some cases, the vertebrae may not fuse properly, leading to ongoing pain and the need for additional surgery.
-
Hardware failure: The screws, rods, or plates used to stabilize the spine may fail or shift over time.
-
Complications from anesthesia: As with any procedure involving anesthesia, there is a risk of reactions or complications related to the anesthetic.
Your surgeon will take steps to minimize these risks and ensure the best possible outcome.
6. How long does it take to recover from spine fusion surgery?
Recovery from spine fusion surgery varies from person to person, but here are some general timelines:
-
Hospital stay: Most patients stay in the hospital for 2 to 5 days after surgery.
-
Initial recovery: Patients may need assistance with daily activities during the first few weeks after surgery. Light activities can usually be resumed within 4 to 6 weeks.
-
Full recovery: It can take 3 to 6 months for the spine to fully heal and for the fusion to occur. Some patients may require physical therapy to regain strength and mobility during this time.
-
Long-term recovery: Full recovery and the return to normal physical activities, such as exercise or heavy lifting, may take 6 months to a year.
7. What are the different types of spine fusion surgeries?
There are several types of spine fusion surgeries, including:
-
Posterior lumbar fusion (PLF): Performed through the back, where the surgeon removes the disc and fuses the vertebrae using metal rods and screws.
-
Anterior lumbar fusion (ALF): Accessed from the front of the body, often used to treat conditions in the lower back.
-
Transforaminal lumbar interbody fusion (TLIF): A minimally invasive technique performed through the back to remove the disc and place a graft between the vertebrae.
-
Lateral lumbar interbody fusion (LLIF): The surgeon approaches the spine from the side to avoid muscle disruption and access the disc.
-
Cervical spine fusion: Performed to treat conditions in the neck, often done via the anterior approach.
The choice of technique depends on the location and severity of the problem being treated.
8. Can spine fusion be performed on older adults?
Yes, spine fusion surgery can be performed on older adults, but certain considerations must be taken into account. Older adults may have other health conditions (such as osteoporosis or cardiovascular disease) that can impact recovery and surgical outcomes. However, spine fusion can still be effective for improving quality of life and relieving pain, particularly when conservative treatments have failed. Your surgeon will assess your overall health and tailor the treatment plan accordingly.
9. Will I be able to move normally after spine fusion surgery?
After spine fusion surgery, movement may be restricted initially to allow for proper healing. The goal of the surgery is to stabilize the spine, which may result in reduced range of motion in the affected area. However, many patients experience significant relief from pain and stiffness, which improves their overall mobility. The degree of restriction will depend on the location of the fusion and your recovery progress. Physical therapy may be recommended to help restore strength and flexibility.
10. How much does spine fusion surgery cost?
The cost of spine fusion surgery can vary significantly depending on factors such as the location, healthcare provider, and complexity of the procedure. On average, the cost of spine fusion surgery can range from $30,000 to $100,000 or more. This includes surgeon fees, anesthesia, hospital stay, and any post-surgical rehabilitation or follow-up care. Insurance may cover a significant portion of the costs if the surgery is deemed medically necessary, but it’s important to check with your provider to understand your coverage options.
The other Spine Surgery Procedures are:
Few Major Hospitals for Spinal Fusion are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


