Urinary incontinence refers to the involuntary leakage of urine, a condition that can significantly impact an individual’s quality of life. One of the advanced treatments for urinary incontinence, especially for those suffering from stress urinary incontinence (SUI), is the artificial urinary sphincter (AUS). This device is primarily used for individuals who cannot control their urinary function due to weak or damaged bladder sphincters.
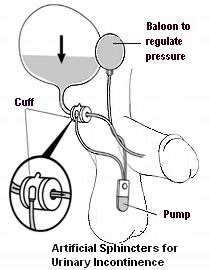
The artificial urinary sphincter works by mimicking the function of a healthy, natural sphincter. The device consists of a cuff, a pump, and a pressure-regulating balloon, and it is typically implanted around the urethra to control the flow of urine. Once activated, the artificial sphincter helps prevent urine leakage by compressing the urethra until the patient is ready to urinate. The patient can control the sphincter by pressing a pump that releases the pressure from the cuff, allowing for normal urination.
While the device is highly effective in treating incontinence caused by sphincter weakness, it is often considered only after conservative treatments, such as medications or physical therapy, have failed. It is most commonly used in men who have developed incontinence after prostate surgery or spinal cord injuries. However, women with severe incontinence may also be candidates for an artificial sphincter.
Several factors contribute to urinary incontinence, and in particular, the need for an artificial sphincter. Understanding these causes and risk factors is key to determining the appropriateness of the device for managing the condition.
1. Damage to the External Sphincter
The external urinary sphincter is a muscle that plays a crucial role in holding urine in the bladder. When this muscle is damaged due to injury or surgery, it may no longer be able to control urine flow, leading to incontinence. For example, prostate surgery or pelvic surgery can damage the sphincter, and an artificial sphincter can be an effective solution.
2. Nerve Damage
Damage to the nerves controlling the bladder and sphincter muscles can lead to incontinence. This damage can occur due to spinal cord injuries, diabetes, stroke, or multiple sclerosis. The nerves may fail to send proper signals to the bladder or sphincter, causing urine leakage.
3. Age-Related Weakening of the Sphincter
As people age, the muscles and tissues of the bladder and sphincters may weaken. This natural deterioration can contribute to the development of urinary incontinence. Older adults may have a higher incidence of stress urinary incontinence, making artificial sphincters an effective option in some cases.
4. Prostate Cancer and Surgery
Prostate cancer treatments, especially prostatectomies (removal of the prostate), are one of the leading causes of male urinary incontinence. Damage to the nerves or muscles around the urethra during these surgeries can result in significant leakage of urine. An artificial sphincter provides a solution to this issue, helping men regain control over their urinary functions.
5. Childbirth-Related Trauma (Women)
Although less common than in men, women may develop incontinence after childbirth due to damage to the pelvic muscles and nerves. In severe cases of stress urinary incontinence, an artificial sphincter may be considered when other treatment options have not worked.
While the artificial sphincter itself is a device used to manage symptoms, understanding the symptoms of urinary incontinence that lead to the use of this device is essential.
1. Involuntary Urine Leakage
The primary symptom of urinary incontinence is involuntary urine leakage. This can range from occasional dribbles to complete loss of bladder control. For patients with damaged sphincters, urine leakage often occurs during physical activities like sneezing, coughing, lifting, or exercise (stress incontinence).
2. Constant Dripping or Wetness
Some individuals with sphincter-related incontinence may experience constant dribbling of urine, even when they are not exerting themselves. This symptom is typically more severe and may indicate the need for an artificial sphincter.
3. Frequent and Urgent Urination
Patients with incontinence may also experience frequent urges to urinate, even when the bladder is not full. The urge may be so strong that the individual cannot reach the bathroom in time, resulting in accidents.
4. Leakage during Specific Activities
For many patients, the leakage of urine only occurs during specific actions, such as standing up from a seated position, laughing, or physical exertion. This is commonly seen in those with stress incontinence resulting from sphincter muscle weakness.
5. Difficulty Holding Urine
Some individuals may feel as if they cannot hold urine, particularly if they are near a toilet or feel the urge to urinate. This is a common symptom seen in individuals with nerve damage or weakened sphincters.
To determine if an artificial sphincter is an appropriate solution, a series of diagnostic steps are taken:
1. Medical History and Symptom Review
The healthcare provider will begin by reviewing the patient’s medical history and conducting a thorough evaluation of the symptoms. This includes asking questions about the frequency of incontinence, its triggers, and its impact on the patient’s quality of life.
2. Physical Examination
A physical exam is conducted to assess the pelvic area, check for signs of muscle weakness, and evaluate the patient’s ability to hold urine. In men, this may include a prostate exam to rule out other possible causes of urinary incontinence.
3. Urodynamic Testing
Urodynamics is a test that measures how well the bladder, sphincters, and urethra are functioning. This includes evaluating how much urine the bladder can hold, how efficiently it empties, and if there is leakage. This test helps to assess the severity of incontinence and whether an artificial sphincter is needed.
4. Imaging Tests
Imaging techniques such as ultrasound or MRI may be used to visualize the urinary tract and detect any structural abnormalities or injuries that could be contributing to incontinence.
5. Cystoscopy
A cystoscopy involves inserting a thin tube with a camera into the bladder to inspect the internal structures. This procedure is useful for identifying issues such as bladder injuries, tumors, or abnormalities in the sphincter.
Once the diagnosis is confirmed, there are several treatment options for urinary incontinence, and an artificial sphincter may be one of the most effective solutions for certain patients.
1. Conservative Treatment (Non-Surgical)
Before considering surgery, conservative treatments such as pelvic floor exercises (Kegel exercises), behavioral therapies, bladder training, and medications may be recommended. These approaches can strengthen the sphincter muscles and reduce the frequency of incontinence.
2. Surgical Treatment: Artificial Urinary Sphincter (AUS)
The artificial sphincter is a mechanical device that helps control urinary incontinence by mimicking the function of the natural sphincter. The procedure involves implanting a cuff around the urethra, a pump in the scrotum (for men) or labia (for women), and a pressure-regulating balloon in the abdomen. The pump is used by the patient to control the flow of urine by inflating or deflating the cuff.
3. Other Surgical Options
In some cases, other surgeries may be performed to treat the underlying cause of incontinence. These include slings, bladder neck suspension, or urethral bulking agents, which aim to reinforce the urethra and prevent urine leakage.
While urinary incontinence is not always preventable, there are several management strategies to minimize its impact and improve overall quality of life after receiving an artificial sphincter.
1. Follow-Up Care
Regular follow-up appointments with the surgeon or urologist are essential to ensure the artificial sphincter is functioning properly. Patients may need adjustments to the device or further evaluation if they experience issues.
2. Pelvic Floor Exercises
Even after the surgery, pelvic floor exercises remain important to strengthen the muscles around the bladder and urethra, supporting the artificial sphincter and reducing the risk of complications.
3. Maintaining a Healthy Weight
Obesity can put extra pressure on the bladder and exacerbate incontinence. Maintaining a healthy weight through diet and exercise can help minimize incontinence symptoms.
4. Avoiding Bladder Irritants
Certain foods and drinks, like caffeine, alcohol, and spicy foods, can irritate the bladder and worsen incontinence. Avoiding these can help in managing symptoms.
While artificial sphincters are effective in managing urinary incontinence, they can have complications. Some potential risks and complications include:
1. Infection
Infections around the implant site or in the urinary tract can occur, especially shortly after surgery. Prompt medical attention is necessary to avoid serious complications.
2. Device Malfunction
Over time, the artificial sphincter may fail, requiring adjustments or replacement. The cuff may also lose pressure, leading to incontinence.
3. Urinary Retention
In rare cases, the sphincter may cause difficulty in urination or urinary retention, which requires further treatment or adjustments to the device.
4. Blood Clots
As with any surgery, there is a risk of blood clots, particularly in the legs, which could travel to the lungs (pulmonary embolism) if not treated promptly.
Living with an artificial sphincter requires significant lifestyle adjustments and regular monitoring to ensure the device functions optimally.
1. Lifelong Management
After surgery, patients will need to learn how to use the device and follow up regularly with their healthcare provider to ensure everything is functioning properly.
2. Emotional Support
Dealing with urinary incontinence and undergoing surgery can be emotionally challenging. Psychological support and counseling may be beneficial in managing self-esteem and body image concerns.
3. Diet and Hydration
Maintaining a healthy diet and staying hydrated is important for bladder health and can help prevent complications such as infections or urinary retention.
1. What is an artificial sphincter for urinary incontinence?
An artificial sphincter is a medical device used to treat urinary incontinence, a condition where an individual loses control over their bladder. The artificial sphincter is typically used for patients who have severe incontinence due to a weakened or damaged external sphincter (the muscle controlling the release of urine). The device consists of a cuff that is placed around the urethra, a pump implanted in the scrotum (for men) or labia (for women), and a pressure-regulating balloon, all of which work together to control urine flow.
2. Who is a candidate for an artificial sphincter?
An artificial sphincter is typically recommended for individuals who:
-
Suffer from severe urinary incontinence that does not respond to conservative treatments such as medications or pelvic floor exercises.
-
Have damaged or weakened external sphincter muscles, often due to prostate surgery, pelvic injury, or nerve damage.
-
Are in good overall health and able to undergo surgery.
-
Have a realistic understanding of the procedure, including the need for long-term management of the device.
A consultation with a urologist is necessary to determine if an artificial sphincter is a suitable option.
3. How does an artificial sphincter work?
An artificial sphincter works by mimicking the function of the natural urinary sphincter, which controls the flow of urine. The device consists of:
-
A cuff: Placed around the urethra to control urine flow by squeezing the urethra shut.
-
A pump: Implanted in the scrotum or labia that the patient can press to release or close the cuff.
-
A pressure-regulating balloon: Positioned in the abdomen to maintain the cuff’s pressure.
When the patient needs to urinate, they press the pump to deflate the cuff, allowing urine to pass through. Once the patient is finished, the cuff automatically inflates to stop the flow of urine.
4. What are the benefits of using an artificial sphincter?
The primary benefits of an artificial sphincter for urinary incontinence include:
-
Restoration of bladder control: The device helps patients regain control over their urinary function and prevents unwanted leakage.
-
Improved quality of life: Many patients experience a significant improvement in their daily life, with less worry about incontinence.
-
Long-term solution: The artificial sphincter offers a long-lasting solution for those who have not had success with other treatments like medications or lifestyle changes.
-
Minimal invasiveness: While it requires surgery to implant, the procedure is minimally invasive compared to other surgical options.
5. How is the artificial sphincter implanted?
The implantation of an artificial sphincter typically involves the following steps:
-
Anesthesia: The patient is given general or spinal anesthesia to ensure they are comfortable and pain-free during the procedure.
-
Surgical incision: The surgeon makes small incisions to access the urethra and surrounding tissues. For men, the incision is usually made near the scrotum, while for women, the incision may be made near the labia.
-
Placement of the device: The cuff is placed around the urethra, the pump is positioned in the scrotum or labia, and the pressure-regulating balloon is inserted into the abdomen.
-
Testing: The device is tested to ensure proper function and placement.
-
Closing the incisions: Once the device is implanted and functioning correctly, the incisions are closed.
The surgery typically takes 1 to 2 hours, and patients may stay in the hospital for 1 to 2 days.
6. What is the recovery time after artificial sphincter surgery?
Recovery time after artificial sphincter surgery varies but generally includes:
-
Hospital stay: Most patients stay in the hospital for 1 to 2 days after surgery for monitoring and pain management.
-
Initial recovery: Patients may experience swelling, bruising, and discomfort in the surgical area for the first few weeks. Pain medications are typically prescribed.
-
Physical activity: Patients are advised to avoid strenuous activities and heavy lifting for about 4 to 6 weeks to allow the device to settle and the body to heal.
-
Full recovery: It can take 4 to 6 weeks for patients to return to normal activities, and 6 months for the device to function optimally.
Physical therapy or pelvic floor exercises may be recommended to improve muscle strength and support recovery.
7. Are there any risks or complications associated with artificial sphincters?
As with any surgical procedure, there are risks and complications associated with artificial sphincters, including:
-
Infection: There is a risk of infection at the surgical site or inside the body, especially in the early stages after surgery.
-
Device malfunction: The cuff, pump, or balloon may malfunction, requiring further surgery to repair or replace the device.
-
Urinary retention: In some cases, patients may have difficulty fully emptying their bladder after surgery.
-
Erosion or displacement: The device may erode into surrounding tissues or shift out of place, requiring revision surgery.
-
Bleeding or hematoma: Some patients may experience bleeding at the surgical site, leading to bruising or swelling.
Choosing an experienced surgeon can help reduce the risks of complications.
8. How does the artificial sphincter improve urinary incontinence?
The artificial sphincter improves urinary incontinence by mimicking the function of the natural urinary sphincter, which controls the flow of urine. By placing the cuff around the urethra, the device helps to prevent urine leakage. The patient can manually control the release of urine by pressing the pump, which deflates the cuff to allow for urination. Once the patient is finished, the cuff automatically inflates to close the urethra and prevent further leakage. This provides a functional, controllable solution for those suffering from severe urinary incontinence.
9. How long does an artificial sphincter last?
An artificial sphincter is designed to last for several years, typically 5 to 10 years, depending on factors such as the patient’s health, activity level, and the device’s maintenance. Over time, wear and tear may lead to device malfunction, and it may need to be replaced or repaired. Regular follow-up visits with the urologist are essential to monitor the device’s function and address any issues before they become serious.
10. How much does artificial sphincter surgery cost?
The cost of artificial sphincter surgery can vary widely depending on factors like location, surgeon, and the complexity of the case. On average, the procedure may cost between $10,000 and $20,000. This cost typically includes the surgeon’s fees, anesthesia, hospital stay, and follow-up care. Insurance may cover a significant portion of the cost if the surgery is deemed medically necessary, but it’s important to check with your insurance provider for specific coverage details.
These FAQs provide a comprehensive overview of Artificial Sphincters for Urinary Incontinence, covering the procedure, benefits, risks, recovery, and costs. Feel free to adjust the content based on your medical website’s tone and audience!
Diagnosis
Medical History
The first step in solving a
urinary problem is talking with your health care provider. Your general medical history,
including any major illnesses or surgeries and details about your continence problem and
when it started will help your doctor determine the cause. You should talk about how much
fluid you drink a day and whether you use alcohol or caffeine. You should also talk about
the medicines you take, both prescription and nonprescription, because they might be part of
the problem.
Voiding Diary
You may be asked to keep a voiding diary, which is a record of
fluid intake and trips to the bathroom, plus any episodes of leakage. Studying the diary
will give your health care provider a better idea of your problem and help direct additional
tests.
Physical Examination
A physical exam will check for prostate enlargement or nerve
damage. In a digital rectal exam, the doctor inserts a gloved finger into the rectum and
feels the part of the prostate next to it. This exam gives the doctor a general idea of the
size and condition of the gland. To check for nerve damage, the doctor may ask about
tingling sensations or feelings of numbness and may check for changes in sensation, muscle
tone and reflexes.
EEG and EMG
Your doctor might recommend other tests, including an
electroencephalogram (EEG), a test where wires are taped to the forehead to sense
dysfunction in the brain. In an electromyogram (EMG), the wires are taped to the
lower abdomen to measure nerve activity in muscles and muscular activity that may be related
to loss of bladder control.
Ultrasound
For an ultrasound, or sonography, a technician holds a device, called a transducer, that sends harmless sound waves into the body and catches them as they bounce back off the organs inside to create a picture on a monitor. In abdominal ultrasound, the technician slides the transducer over the surface of your abdomen for images of the bladder and kidneys. In transrectal ultrasound, the technician uses a wand inserted in the rectum for images of the prostate.
Urodynamic Testing
Urodynamic testing focuses on the bladder’s ability to store urine and empty steadily and completely and on your sphincter control mechanism. It can also show whether the bladder is having abnormal contractions that cause leakage. The testing involves measuring pressure in the bladder as it is filled with fluid through a small catheter. This test can help identify limited bladder capacity, bladder overactivity or underactivity, weak sphincter muscles, or urinary obstruction. If the test is performed with EMG surface pads, it can also detect abnormal nerve signals and uncontrolled bladder contractions.
Treatment
No single treatment works for everyone. Your treatment will depend on the type and severity of your problem, your lifestyle, and your preferences, starting with the simpler treatment options. Many men regain urinary control by changing a few habits and doing exercises to strengthen the muscles that hold urine in the bladder. If these behavioral treatments do not work, you may choose to try medicines or a continence device—either an artificial sphincter or a catheter. For some men, surgery is the best choice.
Behavioral Treatments
For some men, avoiding incontinence is as simple as limiting fluids at certain times of the day or planning regular trips to the bathroom—a therapy called timed voiding or bladder training. As you gain control, you can extend the time between trips. Bladder training also includes Kegel exercises to strengthen the pelvic muscles, which help hold urine in the bladder. Extensive studies have not yet conclusively shown that Kegel exercises are effective in reducing incontinence in men, but many clinicians find them to be an important element in therapy for men.
Kegel exercises
The first step is to find the right muscles. Imagine that you are trying to stop yourself from passing gas. Squeeze the muscles you would use. If you sense a “pulling” feeling, those are the right muscles for pelvic exercises.
Do not squeeze other muscles at the same time or hold your breath. Also, be careful not to tighten your stomach, leg, or buttock muscles. Squeezing the wrong muscles can put more pressure on your bladder control muscles. Squeeze just the pelvic muscles.
Pull in the pelvic muscles and hold for a count of 3. Then relax for a count of 3. Repeat, but do not overdo it. Work up to 3 sets of 10 repeats. Start doing your pelvic muscle exercises lying down. This position is the easiest for doing Kegel exercises because the muscles then do not need to work against gravity. When your muscles get stronger, do your exercises sitting or standing. Working against gravity is like adding more weight.
Be patient. Do not give up. It takes just 5 minutes, three times a day. Your bladder control may not improve for 3 to 6 weeks, although most people notice an improvement after a few weeks.
Medicines
Medicines can affect bladder control in many ways. Some medicines help prevent incontinence by slowing the production of urine, while others block abnormal nerve signals that make the bladder contract at the wrong time. Still others relax the bladder or shrink the prostate. Your doctor may consider changing a prescription that you already take before prescribing medicine to treat incontinence.
The other Urology Procedures are:
Few Major Hospitals for Treatment of Urinary Incontinence are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Laparoscopic Sterilization| Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


