Introduction to Radical Prostatectomy
Radical prostatectomy is a surgical procedure primarily used to treat prostate cancer by removing the entire prostate gland along with some of the surrounding tissue, including the seminal vesicles. The prostate is a small gland located beneath the bladder in men, and its primary function is to produce seminal fluid that nourishes and transports sperm. When cancer develops in the prostate, it can grow and spread to nearby tissues, making prostate removal an important treatment option for localized prostate cancer.
The procedure is typically recommended for men diagnosed with prostate cancer that is confined to the prostate gland and has not spread to other parts of the body. Radical prostatectomy can significantly improve the chances of curing the cancer and is often performed when other treatments, such as radiation therapy or active surveillance, are not viable or have not been successful.
Radical prostatectomy can be performed using various techniques, including open surgery, laparoscopic surgery, or robotic-assisted surgery. Open radical prostatectomy involves a single large incision in the lower abdomen to access and remove the prostate. Laparoscopic and robotic-assisted surgeries are minimally invasive approaches that involve smaller incisions and the use of specialized instruments, including a robotic system, to enhance precision and reduce recovery time. Robotic-assisted surgery, in particular, has become increasingly popular due to its ability to provide greater accuracy and quicker recovery times.
After radical prostatectomy, patients may experience side effects, such as incontinence (difficulty controlling urine) and erectile dysfunction. However, advances in surgical techniques, such as nerve-sparing prostatectomy, have helped reduce the risk of these complications by preserving the nerves that control bladder and sexual function. The recovery process typically involves hospital stays of a few days, followed by several weeks of recovery at home. Post-surgery, patients often require physical therapy or rehabilitation to manage urinary function and regain strength.
Radical prostatectomy is considered a highly effective treatment for localized prostate cancer, offering patients the potential for long-term cancer-free survival. However, as with any major surgery, it carries risks such as bleeding, infection, or complications related to anesthesia, and requires careful consideration and consultation with an experienced urologist or oncologist.
Radical prostatectomy is primarily performed as a treatment for prostate cancer, which can be caused by several factors, some of which increase a man’s risk for developing the disease. The main causes and risk factors include:
1. Age
The likelihood of developing prostate cancer increases with age, particularly after age 50. Prostate cancer is rare in men under 40, but the risk significantly rises as men grow older.
2. Family History
Having a family history of prostate cancer can increase a man’s risk of developing the disease. Men with a father or brother who had prostate cancer are at a higher risk of being diagnosed.
3. Genetics
Certain genetic mutations can increase the likelihood of prostate cancer. For instance, mutations in genes like BRCA1 and BRCA2, which are more commonly associated with breast and ovarian cancer, have been linked to an increased risk of prostate cancer.
4. Race and Ethnicity
Prostate cancer is more common in African-American men than in men of other races. African-American men are also more likely to have a more aggressive form of the disease.
5. Diet
Dietary factors may play a role in prostate cancer development. A diet high in red meat, high-fat dairy, and processed foods has been linked to an increased risk, though the exact relationship is not fully understood.
6. Hormonal Factors
Testosterone, a hormone that fuels prostate cancer cell growth, is often involved in the development and progression of prostate cancer. Elevated levels of testosterone may increase the likelihood of developing prostate cancer.
7. Obesity
Being overweight or obese has been associated with an increased risk of developing more aggressive prostate cancer, which may affect treatment options like radical prostatectomy.
Prostate cancer, especially in its early stages, may not present noticeable symptoms. However, as the disease progresses, there are some symptoms and signs that may prompt a doctor to recommend radical prostatectomy:
1. Frequent Urination
One of the early signs of prostate cancer is increased urinary frequency, especially during the night (nocturia). This happens because the enlarged prostate may press against the bladder, leading to the sensation of needing to urinate more often.
2. Painful Urination
Dysuria, or pain during urination, is another sign that might suggest prostate issues, including cancer. It could be caused by inflammation or blockage in the urethra.
3. Blood in Urine or Semen
Finding blood in the urine (hematuria) or semen (hematospermia) is a concerning symptom that may require immediate medical evaluation. While it does not always indicate cancer, it is important to investigate the cause.
4. Erectile Dysfunction
Prostate cancer can interfere with the blood flow to the penis or the nerves that control an erection. As a result, erectile dysfunction is a common symptom.
5. Pain in the Pelvis, Hips, or Lower Back
As prostate cancer spreads, it can affect nearby bones and tissues. Pain in the pelvic area, lower back, or hips may indicate cancer spread to the bones.
6. Weak or Interrupted Urine Flow
A reduction in the strength of the urine stream or difficulty starting urination could be a sign of prostate enlargement, which may be related to cancer.
Before performing radical prostatectomy, doctors use a variety of diagnostic tests to confirm the presence of prostate cancer and evaluate its extent:
1. Digital Rectal Exam (DRE)
A digital rectal exam is a routine screening procedure where the doctor inserts a gloved finger into the rectum to feel the prostate gland for abnormalities such as lumps or hard areas that may indicate cancer.
2. Prostate-Specific Antigen (PSA) Test
The PSA test measures the level of prostate-specific antigen in the blood. Elevated PSA levels may suggest the presence of prostate cancer, though other factors such as benign prostatic hyperplasia (BPH) can also cause elevated PSA.
3. Biopsy
A prostate biopsy is used to confirm the diagnosis of prostate cancer. During the biopsy, small samples of prostate tissue are removed using a needle and examined for cancerous cells.
4. Imaging Tests
-
Transrectal Ultrasound (TRUS): Used to guide the biopsy needle to the prostate, this imaging test helps identify abnormal areas within the prostate.
-
CT Scan (Computed Tomography): A CT scan may be used to determine if the cancer has spread to nearby lymph nodes or other organs.
-
MRI (Magnetic Resonance Imaging): MRI can offer detailed images of the prostate and surrounding tissues, providing critical information about the extent of cancer.
5. Bone Scan
If there is suspicion that the cancer has spread to the bones, a bone scan may be done to detect metastasis.
The primary treatment for localized prostate cancer is radical prostatectomy, which may be performed using one of the following approaches:
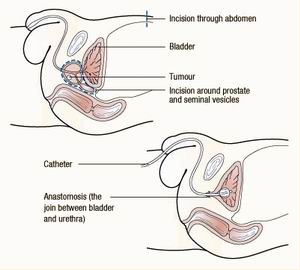
1. Open Radical Prostatectomy
This traditional method involves a large incision in the lower abdomen to access the prostate. It is most often recommended for larger tumors or when other procedures are not feasible.
2. Laparoscopic Prostatectomy
In this minimally invasive technique, small incisions are made, and special instruments are used to remove the prostate. The surgeon is guided by a camera to perform the surgery with high precision.
3. Robotic-Assisted Prostatectomy
A form of laparoscopic surgery, robotic-assisted prostatectomy uses a robotic system to allow for greater precision and control. It results in smaller incisions, reduced blood loss, and quicker recovery.
4. Radiation Therapy
For patients who may not be candidates for surgery, or as an adjunct to surgery, radiation therapy may be used. It can target prostate cancer cells and shrink the tumor.
5. Hormone Therapy
Hormone therapy, also known as androgen deprivation therapy (ADT), is used to lower testosterone levels, which can help shrink or slow the growth of prostate cancer cells.
6. Chemotherapy
Chemotherapy is an option when prostate cancer has spread beyond the prostate gland. It is used to kill cancer cells throughout the body.
Although prostate cancer cannot always be prevented, certain lifestyle changes and regular screenings can help manage risk:
1. Regular Screening
Men at high risk of prostate cancer should undergo regular PSA testing and digital rectal exams (DRE) to detect potential problems early.
2. Healthy Lifestyle
Adopting a healthy lifestyle by eating a balanced diet, exercising regularly, and avoiding smoking can help reduce the risk of prostate cancer.
3. Hormonal Control
For patients at risk of hormone-sensitive cancers, treatments that control or reduce testosterone levels may be beneficial.
Though radical prostatectomy is generally effective, it carries potential risks and complications, such as:
1. Erectile Dysfunction
One of the most common complications after prostate surgery is erectile dysfunction (ED). The nerves that control erections can be damaged during surgery, leading to difficulty achieving or maintaining an erection.
2. Urinary Incontinence
Urinary incontinence, or the inability to control urination, is another common issue after prostate surgery. It may improve over time, but some patients may need additional treatments.
3. Infection
As with any surgery, there is a risk of infection at the surgical site or in the urinary tract.
4. Blood Loss
Blood loss during surgery is a concern, although it is minimized through modern techniques such as laparoscopic and robotic-assisted surgery.
After radical prostatectomy, patients can expect to have a period of recovery, followed by long-term management:
1. Recovery and Rehabilitation
-
The recovery process typically involves rest, pain management, and physical therapy to regain bladder control and mobility.
-
Many patients experience temporary incontinence and erectile dysfunction, but these can improve over time with appropriate treatment and rehabilitation.
2. Regular Follow-ups
-
Patients should attend follow-up appointments to monitor recovery, assess for complications, and screen for cancer recurrence. PSA levels will be monitored regularly after surgery to ensure no cancer remains.
3. Psychological Support
-
Emotional and psychological support is important during recovery, especially for managing the effects of erectile dysfunction and urinary incontinence. Counseling and support groups can be helpful.
1. What is radical prostatectomy?
Radical prostatectomy is a surgical procedure in which the entire prostate gland is removed. It is typically performed to treat prostate cancer that is confined to the prostate. The surgery involves removing the prostate along with some surrounding tissues, such as the seminal vesicles, and sometimes the lymph nodes, to ensure all cancerous tissue is excised. Radical prostatectomy can be performed via open surgery, laparoscopic surgery, or robotic-assisted surgery.
2. Why is radical prostatectomy performed?
Radical prostatectomy is primarily performed to treat localized prostate cancer, particularly when the cancer is confined to the prostate and has not spread to other parts of the body. It is used when:
-
The cancer is localized (limited to the prostate gland) and the patient’s overall health is good enough for surgery.
-
The patient has a long life expectancy and the benefits of surgery outweigh the potential risks.
-
Other treatment options like radiation or watchful waiting are not ideal for the patient’s condition.
The procedure aims to remove the cancerous tissue completely to improve the patient’s chances of recovery and survival.
3. How is radical prostatectomy performed?
Radical prostatectomy is typically performed under general or spinal anesthesia. The procedure can be done through different surgical approaches:
-
Open surgery: A single, large incision is made in the lower abdomen to access and remove the prostate.
-
Laparoscopic surgery: Small incisions are made, and a camera (laparoscope) and instruments are used to remove the prostate.
-
Robot-assisted surgery: A robotic system is used to perform the surgery with high precision through small incisions, offering benefits like shorter recovery time and less blood loss.
The surgeon removes the prostate and any affected tissues, and the urethra is reconnected to the bladder to restore urinary function.
4. What are the benefits of robotic-assisted radical prostatectomy?
Robotic-assisted radical prostatectomy offers several advantages over traditional open surgery, including:
-
Smaller incisions: Minimally invasive surgery uses small incisions, leading to less tissue damage and scarring.
-
Reduced blood loss: The precision of robotic systems often results in less bleeding during surgery.
-
Shorter recovery time: Patients tend to recover more quickly and experience less pain after robotic surgery.
-
Increased precision: The robotic system allows for more precise dissection of tissues, which is especially important for nerve-sparing procedures that help preserve erectile function and urinary continence.
Overall, robotic-assisted surgery may offer a quicker and less painful recovery compared to traditional surgery.
5. What are the risks and complications of radical prostatectomy?
As with any surgery, radical prostatectomy carries some risks, including:
-
Infection: Risk of infection at the surgical site or in the urinary tract.
-
Bleeding: Some bleeding is common, but excessive blood loss may occur.
-
Urinary incontinence: Difficulty controlling urination after surgery is a common concern, though most patients regain control over time.
-
Erectile dysfunction: Nerve damage during surgery can lead to temporary or permanent erectile dysfunction.
-
Damage to surrounding tissues: In rare cases, nearby structures, such as the bladder or rectum, can be accidentally injured.
-
Lymphocele: Fluid-filled sacs that can form in the lymph nodes after surgery.
Your surgeon will discuss the risks and the steps taken to minimize complications before the procedure.
6. How long does it take to recover from radical prostatectomy?
The recovery time after radical prostatectomy depends on the type of surgery and the patient's overall health:
-
Hospital stay: Most patients stay in the hospital for 1 to 3 days after surgery, depending on the surgical approach and recovery.
-
Initial recovery: Mild discomfort, swelling, and fatigue are common after surgery. Most patients can return to light activities within 2 to 4 weeks.
-
Full recovery: It can take 6 to 8 weeks to fully recover from surgery. During this time, patients are encouraged to gradually return to normal activities, avoiding strenuous exercise or heavy lifting.
-
Urinary function: Some patients may experience urinary incontinence after surgery, but most will see improvement within a few months.
Your surgeon will provide specific post-surgery instructions to help with recovery.
7. What are the long-term effects of radical prostatectomy?
While many men recover well after radical prostatectomy, there are potential long-term effects, including:
-
Urinary incontinence: Some men may experience temporary or permanent difficulty controlling urination, though many regain normal function within a few months.
-
Erectile dysfunction: Nerve damage during surgery can result in difficulty achieving or maintaining an erection. However, some men recover erectile function over time with therapy or medications.
-
Fertility issues: Since the prostate is removed, fertility is affected. Men who want to have children after surgery may consider sperm banking prior to the procedure.
-
Psychological effects: The emotional impact of the surgery, such as changes in sexual function and body image, can affect some men.
Your doctor will provide strategies for managing these effects and offer support during recovery.
8. How effective is radical prostatectomy in treating prostate cancer?
Radical prostatectomy is one of the most effective treatments for localized prostate cancer, particularly for men with cancer confined to the prostate gland. The success rate of the surgery depends on factors such as:
-
Cancer stage: The earlier the cancer is detected, the more successful the surgery tends to be.
-
Surgical technique: Robotic or laparoscopic surgery often offers better outcomes than traditional open surgery due to its precision.
-
Overall health: Patients who are otherwise healthy and have no other medical conditions may experience better outcomes.
In general, if the cancer is confined to the prostate, radical prostatectomy has a high cure rate and offers a good chance of long-term survival.
9. Will I need follow-up treatment after radical prostatectomy?
Yes, follow-up care is essential after radical prostatectomy:
-
Monitoring for cancer recurrence: Your doctor will monitor for signs of cancer recurrence, usually through regular blood tests (such as PSA tests) and imaging studies.
-
Urinary and sexual function: Follow-up visits will assess urinary continence and erectile function. Physical therapy or medications may be prescribed to help with recovery.
-
Lifestyle changes: Your doctor may recommend lifestyle modifications, including dietary changes and exercise, to promote recovery and overall health.
Follow-up visits are typically scheduled for the first 6 months to 1 year after surgery, with ongoing monitoring as needed.
10. How much does radical prostatectomy cost?
The cost of radical prostatectomy can vary widely depending on the facility, location, and type of surgery (open vs. robotic-assisted). On average, the procedure may cost between $10,000 and $30,000, which includes:
-
Surgeon’s fees
-
Hospital or surgical facility fees
-
Anesthesia
-
Post-surgery care and follow-up visits
Insurance may cover a significant portion of the cost if the surgery is deemed medically necessary, so it's important to check with your insurance provider for specific details.
The other Urology Procedures are:
Few Major Hospitals for Radical Prostatectomy are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Vasectomy Reversal | Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


