Transurethral resection of bladder tumor (TURBT) is a minimally invasive surgical procedure commonly used to diagnose and treat bladder cancer. It involves the removal of tumors from the bladder through the urethra, without the need for external incisions. This technique is typically used to treat superficial or early-stage bladder tumors that have not spread deeply into the bladder wall. TURBT is often the first line of treatment for patients diagnosed with bladder cancer and can be both diagnostic and therapeutic, helping to remove visible tumors and collect tissue samples for further analysis.
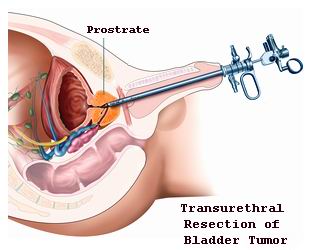
During the procedure, a cystoscope, a thin, flexible tube with a camera, is inserted into the bladder through the urethra. The surgeon can visualize the tumor and use specialized instruments to remove the tumor or tumor tissue. In some cases, the resection may be followed by the use of a laser or electric current to ensure complete removal of the tumor. TURBT not only helps in the diagnosis of bladder cancer by enabling the surgeon to assess the size and location of the tumor but also allows for the treatment of small or localized tumors, reducing the risk of further spread or recurrence.
TURBT is typically performed under general or spinal anesthesia, and the recovery time is generally shorter compared to more invasive surgeries. Most patients can go home the same day or after a short hospital stay. After the procedure, patients may experience temporary discomfort, including blood in the urine, a frequent urge to urinate, or mild pain. These symptoms usually resolve within a few days.
While TURBT is an effective procedure for treating early-stage bladder tumors, follow-up care is crucial. Bladder cancer has a high recurrence rate, so patients often require regular cystoscopies to monitor for any new growths or signs of recurrence. Depending on the extent of the tumor and the patient's individual case, additional treatments such as chemotherapy or immunotherapy may be recommended after TURBT to reduce the risk of cancer returning.
Overall, TURBT is a highly effective, minimally invasive option for treating bladder cancer, offering patients a faster recovery and a better quality of life compared to traditional open surgery. However, as with any surgical procedure, there are risks and potential complications, including bleeding or infection, and it is essential for patients to have a thorough consultation with their urologist to determine the best treatment approach for their condition.
The primary reason for performing TURBT is the presence of bladder cancer, though other conditions, such as bladder cysts or benign tumors, may also be treated through this method. Bladder cancer is the fourth most common cancer in men and occurs in the cells lining the bladder. The exact cause of bladder cancer is still unclear, but several risk factors are known to increase the likelihood of developing it:
1. Smoking
Smoking is the most significant risk factor for bladder cancer. The carcinogens in tobacco smoke pass through the urine and damage the cells in the bladder, significantly increasing the risk of cancer.
2. Age and Gender
Bladder cancer is more common in older adults, particularly those over the age of 55. Men are at a higher risk than women, with a ratio of 3:1 in favor of men.
3. Occupational Hazards
Exposure to certain chemicals in the workplace, especially in industries like dye, rubber, textile manufacturing, and petroleum refining, can increase the risk of developing bladder cancer. These chemicals include aromatic amines, which are harmful when absorbed by the body.
4. Chronic Urinary Infections
Frequent urinary tract infections (UTIs) or bladder inflammation (cystitis), especially when combined with a history of urinary stones, may increase the risk of bladder cancer.
5. Previous Cancer Treatments
Individuals who have undergone radiation or chemotherapy for previous cancers, particularly those affecting the pelvis, are at an increased risk of developing bladder cancer due to the damage caused to bladder tissue.
6. Family History and Genetics
A family history of bladder cancer or specific genetic mutations, such as those found in the TP53 gene, can also increase a person's risk of developing bladder tumors.
7. Chronic Use of Certain Medications
Certain medications, like pioglitazone (used to treat diabetes), have been linked to an increased risk of bladder cancer when used long-term.
In the early stages, bladder cancer may not present significant symptoms, but as the tumor grows, it can cause a variety of signs. Common symptoms and signs that may indicate bladder tumors requiring TURBT include:
1. Hematuria (Blood in Urine)
Hematuria, or blood in the urine, is the most common and most noticeable symptom of bladder tumors. The blood may be visible (gross hematuria) or microscopic, requiring laboratory tests to detect. Hematuria is not always indicative of cancer but should always be investigated.
2. Painful Urination (Dysuria)
Patients may experience pain or discomfort during urination, a symptom that can be associated with bladder cancer or other urological conditions like urinary tract infections.
3. Frequent Urination or Urgency
The presence of a tumor in the bladder may cause an increased urge to urinate or a sensation of needing to urinate frequently, particularly at night (nocturia).
4. Weak Urine Stream
A blockage caused by a tumor may lead to a weakened urine stream or difficulty starting urination. This can result in incomplete emptying of the bladder.
5. Pelvic or Lower Abdominal Pain
As the tumor grows, it may put pressure on surrounding organs, causing pelvic discomfort or a dull ache in the lower abdomen.
6. Fatigue and Unexplained Weight Loss
In more advanced stages, bladder cancer can cause systemic symptoms like fatigue, unexplained weight loss, or general malaise as the body responds to the disease.
The diagnosis of bladder tumors and the decision to perform TURBT involve a combination of clinical examination, imaging, and tissue sampling:
1. Urinalysis
A urinalysis is performed to detect blood, abnormal cells, or other substances in the urine. It can help identify hematuria or other signs of bladder issues.
2. Cystoscopy
The primary diagnostic tool for bladder cancer is cystoscopy, a procedure where a thin, flexible tube with a camera (cystoscope) is inserted into the bladder through the urethra. This allows the physician to directly visualize the bladder lining and identify abnormal growths or tumors.
3. Biopsy
During cystoscopy, if a tumor or suspicious area is found, a biopsy is often performed to obtain tissue samples for examination under a microscope. This helps determine whether the tumor is benign or malignant and guides treatment planning.
4. Imaging Studies
-
CT Scan (Computed Tomography): A CT scan can provide detailed images of the bladder and surrounding structures, helping assess the tumor's size, location, and spread to nearby lymph nodes.
-
Ultrasound: Bladder ultrasound may be used to identify abnormal masses or growths in the bladder.
-
MRI (Magnetic Resonance Imaging): An MRI may be used to further evaluate the bladder and surrounding tissues, especially for large tumors.
Transurethral resection of bladder tumor (TURBT) is the main treatment option for most bladder tumors, particularly those in the superficial layers. Other treatments may include:
1. TURBT (Transurethral Resection of Bladder Tumor)
-
TURBT involves inserting a resectoscope into the bladder through the urethra. The surgeon uses this instrument to remove the tumor and obtain tissue samples (biopsy) for further analysis.
-
The procedure may be done under local anesthesia for smaller tumors or general anesthesia for larger or deeper tumors.
-
TURBT is often followed by intravesical therapy, such as chemotherapy or immunotherapy, to reduce the risk of recurrence.
2. Intravesical Therapy
After TURBT, some patients may require intravesical therapy to treat remaining cancer cells. Chemotherapy drugs like mitomycin C or BCG (Bacillus Calmette-Guerin) are delivered directly into the bladder to reduce the risk of cancer returning.
3. Radical Cystectomy
If the tumor is deep or widespread, radical cystectomy may be needed, which involves the removal of the entire bladder along with surrounding tissues. This may be combined with urinary diversion procedures to allow for normal urination.
4. Radiation Therapy
In cases where surgery is not possible or when cancer has spread to nearby tissues, radiation therapy may be used to target and shrink tumors.
While not all cases of bladder cancer can be prevented, several strategies can help reduce the risk and manage the disease:
1. Regular Screening
Men and women at high risk for bladder cancer, especially smokers or those with a family history, should undergo regular screenings, including urine tests and cystoscopy.
2. Quitting Smoking
Since smoking is the leading cause of bladder cancer, quitting smoking significantly reduces the risk of developing the disease.
3. Diet and Hydration
Drinking plenty of fluids, especially water, helps dilute urine and reduce irritation to the bladder. A balanced diet rich in fruits and vegetables may also lower the risk of cancer.
4. Occupational Safety
Minimizing exposure to chemicals, particularly those found in industries such as dyeing, rubber, and petroleum, can reduce the risk of bladder cancer.
While TURBT is generally a safe and effective procedure, it may be associated with some complications:
1. Infection
Infection, particularly in the urinary tract, is a potential risk after TURBT. Antibiotics are often prescribed to prevent infections.
2. Bleeding
Some bleeding is common after TURBT, but excessive bleeding may require further intervention or transfusion.
3. Bladder Perforation
In rare cases, the bladder may be accidentally perforated during the procedure, leading to leakage of urine into surrounding tissues. This may require additional surgery to repair.
4. Recurrence of Tumors
Bladder tumors have a high rate of recurrence. Patients may require follow-up cystoscopies and additional treatments to ensure that cancer does not return.
Life after TURBT may require several lifestyle adjustments and follow-up care:
1. Regular Follow-Up Appointments
After TURBT, patients must attend regular follow-up appointments with their urologist to monitor for any recurrence of cancer. This may include urine tests, cystoscopies, and other imaging studies.
2. Lifestyle Adjustments
Maintaining a healthy lifestyle by staying hydrated, eating a balanced diet, and avoiding smoking is essential for managing the risk of recurrence and improving overall health.
3. Psychological Support
Living with bladder cancer and the possibility of recurrence can be emotionally challenging. Counseling and support groups may help patients cope with anxiety, stress, and the emotional aspects of their diagnosis.
1. What is Transurethral Resection of Bladder Tumor (TURBT)?
Transurethral resection of bladder tumor (TURBT) is a surgical procedure used to diagnose and treat bladder cancer. During TURBT, a surgeon uses a thin, flexible tube called a cystoscope, which is inserted through the urethra, to access the bladder. The tumor or abnormal tissue is then removed or resected using specialized instruments. TURBT is commonly used for superficial bladder cancers that are confined to the bladder lining or muscle layer but have not spread to other parts of the body.
2. Why is TURBT performed?
TURBT is primarily performed for the treatment of bladder tumors, particularly superficial bladder cancer. It serves both diagnostic and therapeutic purposes, including:
-
Diagnosis of bladder cancer: TURBT allows the doctor to take tissue samples (biopsies) for testing and to confirm the presence of cancer.
-
Treatment of bladder tumors: The procedure removes visible tumors from the bladder lining, which can help relieve symptoms like blood in the urine (hematuria), pain, and frequent urination.
-
Staging and grading: TURBT helps assess how far the cancer has spread within the bladder, which is important for determining further treatment options.
-
Preventing recurrence: Removing tumors early can reduce the likelihood of cancer returning in the future.
3. How is TURBT performed?
TURBT is a minimally invasive procedure typically performed under local or general anesthesia. The steps involved include:
-
Preparation: The patient is positioned on the operating table, and anesthesia is administered. A local anesthetic is used to numb the urethra and bladder, or general anesthesia may be used if the procedure is more complex.
-
Insertion of the cystoscope: A cystoscope (a long, flexible tube with a light and camera) is inserted through the urethra into the bladder.
-
Resection of the tumor: Once inside the bladder, the surgeon uses a specialized tool passed through the cystoscope to remove or resect the tumor(s). The tumor is either removed in small pieces or cauterized to prevent bleeding.
-
Completion: The surgeon may use a catheter to help drain urine and ensure proper healing, and the procedure is completed.
The entire procedure typically takes 30 to 60 minutes, depending on the size and location of the tumor.
4. Is TURBT painful?
During the procedure, the patient is under anesthesia, so no pain is felt. Afterward, mild discomfort, a burning sensation while urinating, or some bladder spasms may occur as the area heals. These symptoms usually subside within a few days to a week. Some patients may experience mild bleeding or blood in the urine for a short period, which is normal. Pain medications and anti-spasmodic drugs are often prescribed to manage any post-surgery discomfort.
5. What are the risks and complications of TURBT?
While TURBT is generally considered safe, there are some risks and potential complications, including:
-
Infection: There is a risk of infection in the urinary tract, bladder, or at the site of the procedure.
-
Bleeding: Some bleeding is common during or after the procedure, though excessive bleeding may require additional treatment.
-
Perforation: Rarely, the cystoscope or instruments may accidentally perforate (puncture) the bladder or surrounding organs.
-
Bladder spasm: Some patients may experience spasms in the bladder, leading to discomfort or urgency.
-
Recurrence of cancer: There is a risk of cancer recurrence after TURBT, which is why regular follow-up visits and surveillance are necessary.
Your urologist will take steps to minimize these risks and monitor you closely after the procedure.
6. How long does it take to recover from TURBT?
Recovery time after TURBT is generally quick:
-
Hospital stay: TURBT is usually performed on an outpatient basis, meaning patients can go home the same day.
-
Initial recovery: Mild discomfort, burning sensations, or blood in the urine may last for a few days to a week after the procedure.
-
Return to normal activities: Most patients can resume light activities within 1 to 2 days, but more strenuous activities, heavy lifting, or sexual activity should be avoided for 2 to 4 weeks.
-
Follow-up care: Regular follow-up visits are necessary to monitor for signs of cancer recurrence and to ensure proper healing.
7. How effective is TURBT in treating bladder cancer?
TURBT is highly effective for treating superficial bladder cancer that is confined to the bladder lining or muscle layer. The procedure can:
-
Remove visible tumors: TURBT helps remove cancerous growths in the bladder and provides immediate relief from symptoms.
-
Assess cancer stage: The procedure allows for staging and grading of the cancer, which guides further treatment decisions (such as chemotherapy or immunotherapy).
-
Prevent recurrence: Early and thorough removal of tumors can reduce the likelihood of cancer returning.
However, in some cases, the cancer may return, so follow-up visits and regular cystoscopies are important for ongoing monitoring.
8. What are the alternatives to TURBT for treating bladder tumors?
While TURBT is the most common and effective treatment for bladder tumors, other options may be considered in certain cases:
-
Intravesical therapy: This involves administering chemotherapy or immunotherapy directly into the bladder to target and kill cancer cells.
-
Cystectomy: In more advanced cases, when the cancer is not confined to the bladder lining, partial or radical cystectomy (removal of part or the entire bladder) may be necessary.
-
Laser therapy: Laser surgery can be used to vaporize tumors in the bladder, though it is typically reserved for smaller, localized tumors.
Your urologist will determine the best treatment option based on the type and stage of the bladder tumor.
9. How long do I need follow-up care after TURBT?
Follow-up care is essential after TURBT to ensure the cancer does not recur:
-
Initial follow-up: Patients typically have a follow-up appointment 3 to 6 weeks after TURBT to assess healing and check for any signs of recurrence through cystoscopy (a camera examination of the bladder).
-
Regular surveillance: After the initial follow-up, cystoscopies are usually scheduled every 3 to 6 months during the first few years, especially for patients with higher-risk tumors.
-
Additional treatments: If cancer is found to be recurring, further treatments such as intravesical chemotherapy or radical cystectomy may be recommended.
Long-term surveillance may be necessary for up to 5 years or more to monitor for recurrence, especially in high-risk cases.
10. How much does TURBT cost?
The cost of TURBT varies depending on factors such as the healthcare facility, location, and whether additional treatments are needed. On average, the cost for a TURBT procedure ranges between $2,000 to $10,000, which includes the surgeon’s fees, anesthesia, hospital stay, and follow-up visits. Additional costs may apply if further treatments, such as intravesical chemotherapy or additional procedures, are required. Insurance often covers TURBT if it is medically necessary, so it’s important to check with your insurance provider for specific coverage details.
The other Urology Procedures are:
Few Major Hospitals for Transurethral Resection of Bladder Tumor are:
Thailand, Malaysia, Singapore, Turkey and India are the most cost effective locations that offer up to almost 80% savings in comparison to the US.
SurgeryPlanet facilitates a plethora of services to the medical treatment traveler also which includes, a hassle free and discounted travel option, a welcome hand at the airport on arrival, travel in an air-conditioned car, round the clock service & support. Your medical evaluation is pre arranged with the least of waiting time. Once your assessment is complete and found medically fit, the procedure is immediately scheduled without a waiting period. Please read through our Services and Testimonials to understand and select your best options.
Major Treatments Abroad: Obesity / Bariatric Surgery | Spine Surgery | Stem Cell therapy | Fertility treatment | Knee replacement in India and Thailand | Heart Surgery | Organ transplant | Ayurveda Treatment | Heart valve replacement | Hip resurfacing | Hospitals in India and Thailand for Vasectomy Reversal | Best hospitals in Asia | JCI & ISO certified Hospitals | Cost effective medical procedures | Healthcare tourism | Complete privacy for affordable cost | Weight loss procedures | Infertility treatment | Board certified physicians | Low cost surgeries.
SurgeryPlanet is an Healthcare Facilitator and not a Medical service provider. The information provided in this website is not to be used for diagnosis or treatment of any medical condition or use for any medical purposes. We provide information solely for medical travel facilitation and do not endorse any particular health care provider, hospital, facility, destination or any healthcare service or treatment listed. We are not an agent for, or affiliated to any health care provider, or service listed in our website and is not responsible for health care services provided by them. Choice of hospital or doctor for your healthcare services is your independent decision. Consult your domestic licensed health care provider before seeking the services of any health care provider you learn about from our website.


